Published online Jan 28, 2020. doi: 10.3748/wjg.v26.i4.416
Peer-review started: September 5, 2019
First decision: September 19, 2019
Revised: December 31, 2019
Accepted: January 8, 2020
Article in press: January 8, 2020
Published online: January 28, 2020
Incidence and severity variations of inflammatory bowel disease (IBD) have been reported from Western populations between continents and regions of the same countries. However, no data were available from other countries.
To investigate the regional differences in the IBD profiles of pediatric patients from the Kingdom of Saudi Arabia.
Data from a national multicenter IBD study were used. The incidence, time trend, and clinical presentation of Crohn’s disease (CD) and ulcerative colitis (UC) in the Central region (CR), Western region (WR), and Eastern region (ER) were analyzed and compared. Statistical analysis included Poisson regression analysis for incidence variation and Chi-square test for demographic and clinical parameters. A P < 0.05 was considered significant.
The prevalence of positive family history was lower in children with CD from the ER than the CR or the WR. Consanguinity rate was higher in children with CD and UC from the CR and the ER, respectively. The incidences and time trends of CD and UC were not significantly different between regions. In the ER, a significantly higher percentage of children with CD presented with abdominal pain (P < 0.001), blood in stools (P = 0.048), stricturing or penetrating disease (P = 0.029), higher erythrocyte sedimentation rate (P < 0.001), higher C-reactive protein (P < 0.001), higher anemia (P = 0.017), and lower albumin level (P = 0.014). For children with UC from the ER, a significantly higher percentage presented with anemia (P = 0.006) and a lower percentage with pancolitis (P < 0.001).
The most important finding is the identification of significantly more severe presentation of CD in the ER of the Kingdom of Saudi Arabia. Prospective studies are needed to explain such variations.
Core tip: This article reports regional variations of Crohn’s disease and ulcerative colitis in the Central region, Western region, and the Eastern region of the Kingdom of Saudi Arabia. Although incidence trend was increasing in all regions, children from the Eastern region presented with a significantly more severe Crohn’s disease than those from the Central region and Western region. Regional analysis in other countries may reveal significant variations indicating the need for prospective studies to identify the causes of such variations.
- Citation: El Mouzan MI, AlEdreesi MH, Hasosah MY, Al-Hussaini AA, Al Sarkhy AA, Assiri AA. Regional variation of pediatric inflammatory bowel disease in Saudi Arabia: Results from a multicenter study. World J Gastroenterol 2020; 26(4): 416-423
- URL: https://www.wjgnet.com/1007-9327/full/v26/i4/416.htm
- DOI: https://dx.doi.org/10.3748/wjg.v26.i4.416
Inflammatory bowel disease (IBD) and its main phenotypes, Crohn’s disease (CD) and ulcerative colitis (UC), are reported with a globally increasing trend[1-4]. Incidence variations with the west-east and north-south falling gradients have been observed across the European continent and within individual countries[5,6]. Over the past three decades, developing countries are reporting more cases of pediatric onset IBD, with a few incidence studies emerging from this part of the world[7-10]. In the Kingdom of Saudi Arabia (KSA), the incidences, time trends, and clinical and laboratory profiles of pediatric IBD have been reported on a national basis[11-17]. However, in view of the different cultures and environments of the three main regions of KSA [Central region (CR), Western region (WR), and Eastern region (ER)], we hypothesize that there may be differences in the IBD profile of the children from these regions. Therefore, the objective of this study was to investigate the regional variability of Pediatric CD and UC profile in the KSA.
The national multicenter pediatric IBD research project was a retrospective descriptive study of children from birth to 17 years of age with confirmed diagnosis of IBD (CD, UC, IBD-U) from 17 medical centers located mainly in the CR, WR, and ER of the KSA. The diagnosis of CD and UC was confirmed based on clinical, laboratory, imaging, endoscopic, and histopathologic findings in accordance to standard guidelines[18]. All children were diagnosed and managed by gastroenterologists. The CR is represented by the greater Riyadh region, the WR is represented by the Makkah region, including Makkah, Jeddah and Taif cities, and the ER includes Dammam, Al Hasa, Al Khobar, Dhahran, Qatif, and Jubail cities. Two age groups were analyzed; the denominator data of the first group, birth to 14 years of age, were available and were analyzed for incidence and time trend. The second group, which included the whole cohort from birth to 17 years of age, was analyzed for demographics, clinical, and laboratory presentations.
Incidence and time trend were analyzed for the age group from birth to 14 years of age only. This is because, in the KSA, adult gastroenterologists managed most children above 15 years of age and were not part of the national multicenter study. Hence, available data from patients above 15 years could not be analyzed for incidence and time trend; however, they were added to those below 15 years to form a cohort from birth to 17 years suitable for the analysis of demographic, clinical, and laboratory presentation. We used the officially published census reports of the Central Department of Statistics and Information denominators for incidence calculations[19]. To investigate the incidence time trend, the yearly incidence of CD and UC in each region were calculated and compared to each other. In addition to this, the incidence trend was evaluated for each region using two intervals: interval 1 (2003-2007) and interval 2 (2008-2012).
In the cohort of children from birth to 17 years of age, demographic features including gender distribution, family history of IBD, consanguinity, duration of illness, age at diagnosis, and diagnostic delay were analyzed. The clinical presentation and selected laboratory markers of severity were compared between regions. These included the proportion of children presenting with weight loss, abdominal pain, diarrhea, blood in stools, complicated presentation in CD (fistulae, strictures), and pancolitis in UC. Laboratory markers included anemia, low albumin, high erythrocyte sedimentation rate, and high C-reactive protein.
Data were analyzed using Statistical Package for Social Studies (SPSS 22; IBM Corp., New York, NY, United States). Categorical variables were expressed as percentages. Chi square test and Fisher exact test were used for categorical variables. Generalized linear Poisson Regression model was used to assess the changes in the incidence rates of UC and CD cases by adjusting region (CR, WR, and ER) and using time period (2003-2012) as the offset variable. A P < 0.05 was considered statistically significant.
The statistical methods of this study were reviewed by Ahmad H. Al sharqawi, Biostatistician, Investigator Support Unit, Prince Naif Health Research Center, King Saud University, Kingdom of Saudi Arabia.
The study is part of the Multicenter Saudi National Pediatric IBD research project approved by the Institutional Review Board of the College of Medicine (No. 10/2647/IRB), King Saud University, Riyadh, Kingdom of Saudi Arabia.
From January 2003 to December 2012, a total number of 459 IBD cases from birth to 17 years (309 CD, 147 UC, 3 IBD-U) were diagnosed. However, because of small numbers, the IBD-U cases were not included in this analysis. The remaining 456 were distributed according to regions: CR 226 (156 CD, 70 UC), WR 134 (80 CD, 54 UC), and ER 96 (73 CD, 23 UC).
The main demographic comparative features are shown in Table 1, indicating a higher number of males with CD and UC from the CR and ER, respectively. The prevalence of positive family history was lower in children with CD from the ER than from the CR or the WR; however, there was no difference in children with UC between the regions. Consanguinity rate was higher in children with CD and UC from the CR and the ER, respectively. The children diagnosed with CD and UC from the ER were characterized by a shorter duration of symptoms before presentation, younger age at diagnosis, and shorter diagnostic delay compared to those diagnosed in the CR or the WR.
| Parameters | Crohn’s disease | Ulcerative colitis | ||||
| Central | West | East | Central | West | East | |
| Number of patients | 156 | 80 | 73 | 70 | 54 | 73 |
| Gender, % males | 94.6 | 44.6 | 37.6 | 39.6 | 21.4 | 17.7 |
| Family history, % positive | 17.5 | 16.2 | 13.9 | 9.2 | 9.3 | 9.5 |
| Consanguinity, % positive | 47 | 31.2 | 33.8 | 41.9 | 24.1 | 52.6 |
| Duration of symptoms (mo): mean ± SD | 17.5 ± 21.8 | 10.8 ± 9.9 | 7.8 ± 9.2 | 8.7 ± 10.1 | 5.8 ± 3.9 | 4.5 ± 3.0 |
| Age at diagnosis (yr): mean ± SD | 14.3 ± 3.5 | 10.0 ± 4.7 | 12.3 ± 3.4 | 9.6 ± 5.0 | 8.9 ± 4.3 | 9.0 ± 3.9 |
| Diagnostic delay (mo): Median (IQR) | 12 (4-25) | 6 (4-12) | 6 (3-6) | 5 (2-9) | 6 (3-9) | 3 (2-6) |
There were 390 children from birth to 14 years of age diagnosed with IBD in the three regions. Fifty-five non-Saudi nationals were excluded from the analysis because of the unavailability of denominator data, while two patients were excluded because of the missing data. The remaining 333 Saudi children constituted the study cohort: The CR 39.6% (132/333), the WR 36.4% (121/333), and the ER 24% (80/333).
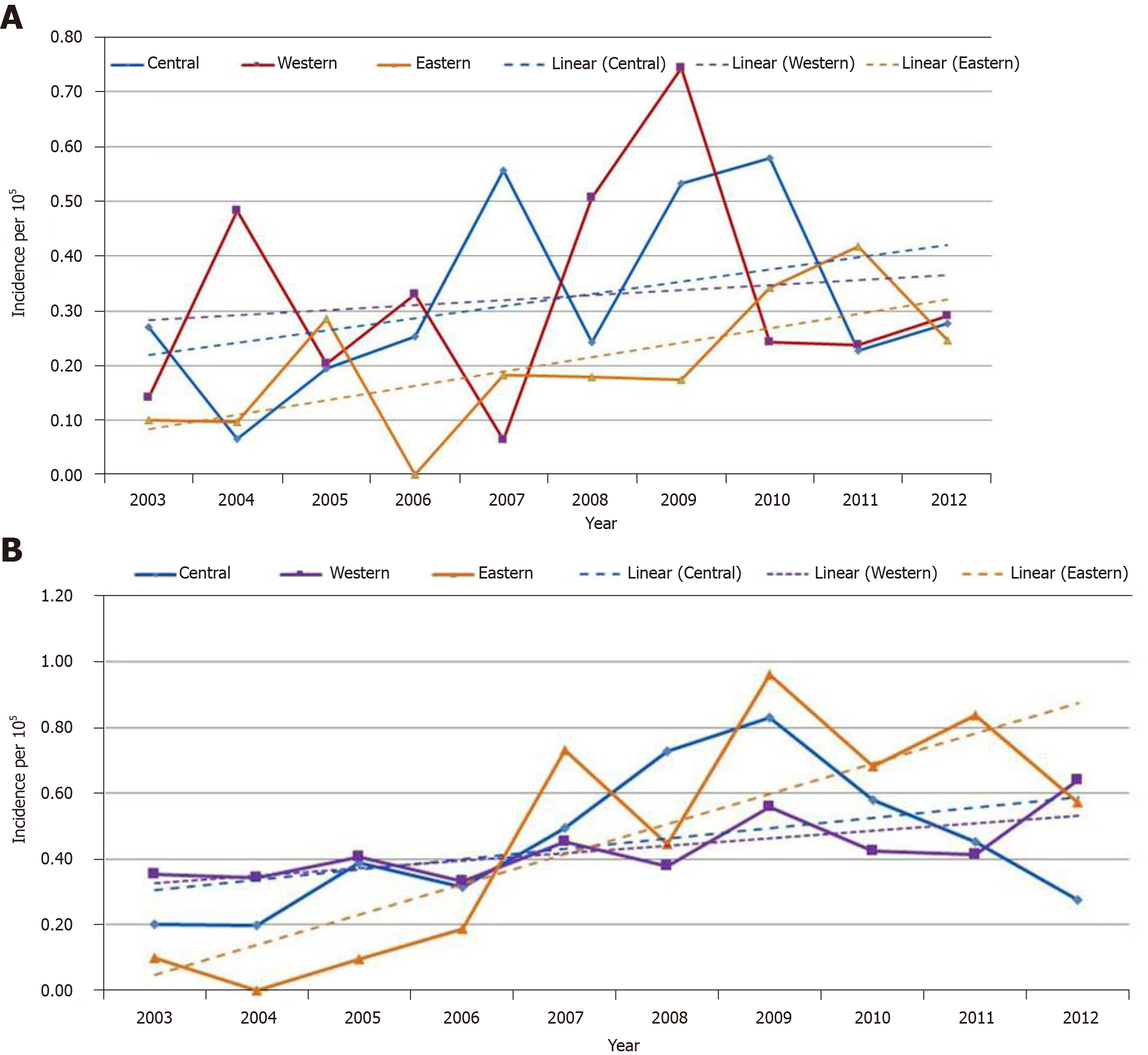
Comparison of the annual mean incidence of UC and CD in the three regions is shown in Figures 1, showing an increasing trend in all regions with no significant difference between them. Comparison of the prevalence trends of two periods (2003-2007 and 2008-2012) between regions presented in Table 2 showed a high trend; however, it was not statistically significant.
| Parameters/time periods | Incidence rates (95%)/100000 | |
| 2003-2007 | 2008-2012 | |
| Ulcerative colitis | ||
| Central region | 0.27 (0.17-0.41) | 0.37 (0.25-0.52) |
| Western region | 0.24 (0.14-0.38) | 0.38 (0.26-0.54) |
| Eastern region | 0.13 (0.05-0.27) | 0.27 (0.16-0.44) |
| Crohn’s disease | ||
| Central region | 0.32 (0.21-0.48) | 0.37 (0.25-0.52) |
| Western region | 0.38 (0.25-55) | 0.46 (0.33-0.63) |
| Eastern region | 0.23 (0.12-0.40) | 0.70 (0.50-0.95) |
Clinical presentation in children with CD is shown in Table 3. This indicates that a significantly higher proportion of children presented with abdominal pain (P = 0.005), complications such as fistula or stenosis (P = 0.029), higher anemia (P = 0.003), higher erythrocyte sedimentation rate (P < 0.001), higher C-reactive protein (P < 0.001), less blood in stools (P = 0.048), and lower albumin levels (P = 0.014) in the ER. For children with UC, clinical and laboratory features are presented in Table 4, indicating a significantly higher percentage of children in the WR presented with diarrhea (P = 0.033), whereas a significantly lower percentage of children in the ER presented with pancolitis (P < 0.001), and a higher percentage presented with anemia (P = 0.006).
| Parameters | Central, % | Western, % | Eastern, % | P value |
| Weight loss | 41.5 | 31.4 | 43.5 | 0.467 |
| Abdominal pain | 87.8 | 75 | 94.3 | 0.005a |
| Diarrhea | 68.9 | 75 | 71.7 | 0.723 |
| Blood in stool | 39.2 | 29.4 | 18.9 | 0.048a |
| Complicated presentation | 22.2 | 20.3 | 40.4 | 0.029a |
| High CRP | 52 | 84.3 | 97.1 | < 0.001a |
| High ESR | 65.6 | 63 | 91.7 | < 0.001a |
| Low serum albumin | 58.3 | 72.4 | 87 | 0.014a |
| Anemia | 46.3 | 54.7 | 77.6 | 0.003a |
| Parameters | Central, % | Western, % | Eastern, % | P value |
| Weight loss | 41.5 | 31.4 | 43.5 | 0.467 |
| Abdominal pain | 67.9 | 52.9 | 73.9 | 0.139 |
| Diarrhea | 73.6 | 92.2 | 78.3 | 0.033a |
| Blood in stool | 92.5 | 96.1 | 91.3 | 0.64 |
| Pancolitis at presentation | 67.9 | 23.5 | 43.5 | < 0.001a |
| High CRP | 58.8 | 71.4 | 45.5 | 0.347 |
| High ESR | 71.4 | 75 | 83.3 | 0.605 |
| Low serum albumin | 48.6 | 30.4 | 52.9 | 0.247 |
| Anemia | 57.4 | 55.6 | 90.9 | 0.006a |
To our knowledge, this is the first study to describe the regional variation in the characteristics of pediatric IBD from a non-Western population. The hypothesis on the possible variations was based on the differences in culture and environment of the main regions of KSA (CR, WR, ER). Most of the population of the CR is tribal, and the environment is dominated by a desert climate and lifestyle. The WR is located near the Red Sea, with a different coastal climate, and the population is less tribal with a different kind of lifestyle. Similarly, the population of the ER, which is located on the Arabian Gulf, is different from the CR and WR in terms of culture. Dominated by oil production and related petrochemical industry, the environment has a coastal climate, and the lifestyle is different from the WR and CR.
Positive family history and consanguinity are considered indirect indicators of genetic susceptibility. In this study, the higher prevalence of positive family history in children with CD and UC in the ER provided a clue for a genetic risk. However, literature suggests that positive family history of pediatric IBD plays a minimal role among the regions[20]. Similarly, comparison of the relatively constant rate of consanguinity in KSA between 1995 and 2013 and the increasing incidence of CD and UC makes the role of consanguinity highly unlikely[21,22]. A previous report from the same population supported this assumption, suggesting that there is no relationship between consanguinity and pediatric IBD[23].
Though it is not statistically significant, the mean annual incidences of CD and UC were increasing in all regions. These findings are consistent with reports of no regional differences in the prevalence of CD between the Northeast and the South, with a higher prevalence of UC in the South of the United States[24].
The most important finding in the study is the significant differences in clinical and laboratory markers at presentation between regions. Compared with the children from the CR and the WR, children from the ER presented with a more severe and complicated CD, a finding that confirms the general impression of some gastroenterologists from the ER (personal communication). The causes of severe CD in the ER were not clear. Late presentation and late diagnosis are unlikely because of the shorter duration of symptoms and shorter diagnostic delay in children from the ER. The ethnic/racial role in the varying profiles of IBD has been reported from different countries emphasizing differences in the incidences and phenotypes between the Blacks, the Hispanics, and the Asians from the United States[24]; between the non-Hispanic Whites, the US-born Hispanics, and the foreign-born Hispanics in the United States[25]; between the Arabs and the Jewish children[26]; and between the Southern Asians living in North West London[27]. However, ethnic/racial factors are unlikely the causes in this relatively homogenous population among all the regions of KSA; instead, it is more likely due to the environmental factors, particularly the lifestyle and microbiota, in the ER.
The most important limitation was the retrospective data collection. As a result of this, we were not able to address more specific markers of severity such as documentation the pediatric activity indices over the course of the illness, use of immuno-suppressants or biological agents, the number of hospitalizations, and the need for surgical interventions; instead, we used indirect clinical and laboratory measures of severity in the three regions.
In this study, the most prominent finding is the severe presentation of CD in the Eastern region of the KSA. Regional exploration of IBD profiles within countries may reveal significant differences, which indicates the need for prospective studies that focus on environmental factors, specifically in the form of dietary lifestyle and microbiota analysis. The result of such studies may increase our understanding of IBD.
Inflammatory bowel disease (IBD) has been reported most commonly in Western populations and rarely in others. Increasing reports from developing countries including the Kingdom of Saudi Arabia (KSA) attracted global interest in the search of factors implicated in the pathogenesis of IBD. The present report, exploring IBD profile in different regions may reveal important regional variations undetectable in global national studies.
Although increasing incidence trend of Pediatric IBD is well known in the KSA, regional variation in culture and lifestyle may be involved in variation of IBD profile. The result may direct further research to clarify the causes of regional variation.
The main objective of this report was to explore regional variations in the profile of pediatric IBD in the KSA. The finding of significantly more severe Crohn’s disease (CD) presentation in children from the Eastern region indicates the need for prospective studies to uncover the causes of this variation from the other regions. The results of such studies may increase our understanding of the pathogenesis of IBD.
Data from a national multicenter study of pediatric IBD were used. The incidence, time trend, and clinical presentation of CD and ulcerative colitis (UC) in the Central, Western, and Eastern regions of the KSA were analyzed, and regional comparison was performed. Poisson regression analysis was used to assess regional incidence and Chi-square test for demographic and clinical parameters. A P < 0.05 was considered significant.
We found increasing incidence trend of pediatric UC and CD in all regions of the KSA. However, comparison with other regions, children with CD from the ER presented with significantly higher prevalence of complications such as fistula or stenosis, higher anemia, erythrocyte sedimentation rate, and C-reactive protein; as well as less blood in stools and lower albumin levels. The causes of this finding of more disease presentation of CD remains to be studied.
In this study, the more severe clinical profile of CD in children from the ER of the KSA is a new finding. We hypothesize that lifestyle and microbiota variation are potential causes. Regional analysis is recommended as it may reveal significant variations undetectable by overall national studies. Prospective studies focusing on environmental factors are needed to search the cause. Identification of factors implicated in the severe clinical presentation in CD may lead to preventive and therapeutic recommendations.
This study revealed significantly more severe clinical presentation of CD in one of the regions (ER) of the KSA. This finding indicates the need for prospective studies to search the causes of this clinical picture.
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Saudi Arabia
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Can G, Ribaldone DG, Souza JLS S-Editor: Dou Y L-Editor: A E-Editor: Qi LL
| 1. | Martín-de-Carpi J, Rodríguez A, Ramos E, Jiménez S, Martínez-Gómez MJ, Medina E, Navas-López VM; SPIRIT-IBD Working Group of SEGHNP (Sociedad Española de Gastroenterología Hepatología Nutrición Pediátrica). The complete picture of changing pediatric inflammatory bowel disease incidence in Spain in 25 years (1985-2009): the EXPERIENCE registry. J Crohns Colitis. 2014;8:763-769. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 30] [Cited by in F6Publishing: 56] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 2. | Malaty HM, Fan X, Opekun AR, Thibodeaux C, Ferry GD. Rising incidence of inflammatory bowel disease among children: a 12-year study. J Pediatr Gastroenterol Nutr. 2010;50:27-31. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 153] [Cited by in F6Publishing: 151] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 3. | Malmborg P, Grahnquist L, Lindholm J, Montgomery S, Hildebrand H. Increasing incidence of paediatric inflammatory bowel disease in northern Stockholm County, 2002-2007. J Pediatr Gastroenterol Nutr. 2013;57:29-34. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 68] [Cited by in F6Publishing: 64] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 4. | El-Matary W, Moroz SP, Bernstein CN. Inflammatory bowel disease in children of Manitoba: 30 years' experience of a tertiary center. J Pediatr Gastroenterol Nutr. 2014;59:763-766. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 38] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 5. | Shivananda S, Lennard-Jones J, Logan R, Fear N, Price A, Carpenter L, van Blankenstein M. Incidence of inflammatory bowel disease across Europe: is there a difference between north and south? Results of the European Collaborative Study on Inflammatory Bowel Disease (EC-IBD). Gut. 1996;39:690-697. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 684] [Cited by in F6Publishing: 643] [Article Influence: 23.0] [Reference Citation Analysis (0)] |
| 6. | Burisch J, Pedersen N, Čuković-Čavka S, Brinar M, Kaimakliotis I, Duricova D, Shonová O, Vind I, Avnstrøm S, Thorsgaard N, Andersen V, Krabbe S, Dahlerup JF, Salupere R, Nielsen KR, Olsen J, Manninen P, Collin P, Tsianos EV, Katsanos KH, Ladefoged K, Lakatos L, Björnsson E, Ragnarsson G, Bailey Y, Odes S, Schwartz D, Martinato M, Lupinacci G, Milla M, De Padova A, D'Incà R, Beltrami M, Kupcinskas L, Kiudelis G, Turcan S, Tighineanu O, Mihu I, Magro F, Barros LF, Goldis A, Lazar D, Belousova E, Nikulina I, Hernandez V, Martinez-Ares D, Almer S, Zhulina Y, Halfvarson J, Arebi N, Sebastian S, Lakatos PL, Langholz E, Munkholm P; EpiCom-group. East-West gradient in the incidence of inflammatory bowel disease in Europe: the ECCO-EpiCom inception cohort. Gut. 2014;63:588-597. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 262] [Cited by in F6Publishing: 263] [Article Influence: 26.3] [Reference Citation Analysis (0)] |
| 7. | Al-Qabandi WA, Buhamrah EK, Hamadi KA, Al-Osaimi SA, Al-Ruwayeh AA, Madda J. Inflammatory bowel disease in children, an evolving problem in Kuwait. Saudi J Gastroenterol. 2011;17:323-327. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 33] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 8. | Ahmaida A, Al-Shaikhi S. Childhood Inflammatory Bowel Disease in Libya: Epidemiological and Clinical features. Libyan J Med. 2009;4:70-74. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Sathiyasekaran M, Bavanandam S, Sankaranarayanan S, Mohan N, Geetha M, Wadhwa N, Kehar M, Biradar V. A questionnaire survey of pediatric inflammatory bowel disease in India. Indian J Gastroenterol. 2014;33:543-549. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 10. | Isa HM, Mohamed AM, Al-Jowder HE, Matrook KA, Althawadi HH. Pediatric Crohn's Disease in Bahrain. Oman Med J. 2018;33:299-308. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | El Mouzan MI, Abdullah AM, Al Habbal MT. Epidemiology of juvenile-onset inflammatory bowel disease in central Saudi Arabia. J Trop Pediatr. 2006;52:69-71. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 36] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 12. | Saadah OI. Ulcerative colitis in children and adolescents from the Western Region of Saudi Arabia. Saudi Med J. 2011;32:943-947. [PubMed] [Cited in This Article: ] |
| 13. | El Mouzan MI, Al Mofarreh MA, Assiri AM, Hamid YH, Al Jebreen AM, Azzam NA. Presenting features of childhood-onset inflammatory bowel disease in the central region of Saudi Arabia. Saudi Med J. 2012;33:423-428. [PubMed] [Cited in This Article: ] |
| 14. | Saadah OI. Childhood onset of Crohn disease: experience from a university teaching hospital in Saudi Arabia. Ann Saudi Med. 2012;32:596-602. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | El Mouzan MI, Saadah O, Al-Saleem K, Al Edreesi M, Hasosah M, Alanazi A, Al Mofarreh M, Asery A, Al Qourain A, Nouli K, Al Hussaini A, Telmesani A, AlReheili K, Alghamdi S, Alrobiaa N, Alzaben A, Mehmadi A, Al Hebbi H, Al Sarkhy A, Al Mehaidib A, Al Saleem B, Assiri A, Wali S. Incidence of pediatric inflammatory bowel disease in Saudi Arabia: a multicenter national study. Inflamm Bowel Dis. 2014;20:1085-1090. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 35] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 16. | AlSaleem K, El Mouzan MI, Saadah OI, AlSaleem B, Al-Hussaini A, Hassosa M, Ali AM, Banemai MO, Halaby H, El Edreesi M. Characteristics of pediatric ulcerative colitis in Saudi Arabia: a multicenter national study. Ann Saudi Med. 2015;35:19-22. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 17. | Al-Hussaini A, El Mouzan M, Hasosah M, Al-Mehaidib A, ALSaleem K, Saadah OI, Al-Edreesi M. Clinical Pattern of Early-Onset Inflammatory Bowel Disease in Saudi Arabia: A Multicenter National Study. Inflamm Bowel Dis. 2016;22:1961-1970. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 18. | Levine A, Koletzko S, Turner D, Escher JC, Cucchiara S, de Ridder L, Kolho KL, Veres G, Russell RK, Paerregaard A, Buderus S, Greer ML, Dias JA, Veereman-Wauters G, Lionetti P, Sladek M, Martin de Carpi J, Staiano A, Ruemmele FM, Wilson DC; European Society of Pediatric Gastroenterology, Hepatology, and Nutrition. ESPGHAN revised porto criteria for the diagnosis of inflammatory bowel disease in children and adolescents. J Pediatr Gastroenterol Nutr. 2014;58:795-806. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 822] [Cited by in F6Publishing: 811] [Article Influence: 81.1] [Reference Citation Analysis (0)] |
| 19. | The Central Department of Statistics Information. Population and housing census 2004 and 2010. Available from: http://cdsi.gov.sa/english. [Cited in This Article: ] |
| 20. | Roma ES, Panayiotou J, Pachoula J, Constantinidou C, Polyzos A, Zellos A, Lagona E, Mantzaris GJ, Syriopoulou VP. Inflammatory bowel disease in children: the role of a positive family history. Eur J Gastroenterol Hepatol. 2010;22:710-715. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 21. | el-Hazmi MA, al-Swailem AR, Warsy AS, al-Swailem AM, Sulaimani R, al-Meshari AA. Consanguinity among the Saudi Arabian population. J Med Genet. 1995;32:623-626. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 247] [Cited by in F6Publishing: 253] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 22. | El-Mouzan MI, Al-Salloum AA, Al-Herbish AS, Qurachi MM, Al-Omar AA. Regional variations in the prevalence of consanguinity in Saudi Arabia. Saudi Med J. 2007;28:1881-1884. [PubMed] [Cited in This Article: ] |
| 23. | El Mouzan M, Al-Mofarreh M, Assiri A, Hamid Y, Saeed A. Consanguinity and inflammatory bowel diseases: is there a relation? J Pediatr Gastroenterol Nutr. 2013;56:182-185. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 24. | Wang YR, Loftus EV, Cangemi JR, Picco MF. Racial/Ethnic and regional differences in the prevalence of inflammatory bowel disease in the United States. Digestion. 2013;88:20-25. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 25. | Damas OM, Jahann DA, Reznik R, McCauley JL, Tamariz L, Deshpande AR, Abreu MT, Sussman DA. Phenotypic manifestations of inflammatory bowel disease differ between Hispanics and non-Hispanic whites: results of a large cohort study. Am J Gastroenterol. 2013;108:231-239. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 53] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 26. | Rinawi F, Assa A, Bashir H, Peleg S, Shamir R. Clinical and Phenotypic Differences in Inflammatory Bowel Disease Among Arab and Jewish Children in Israel. Dig Dis Sci. 2017;62:2095-2101. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 27. | Walker DG, Williams HR, Kane SP, Mawdsley JE, Arnold J, McNeil I, Thomas HJ, Teare JP, Hart AL, Pitcher MC, Walters JR, Marshall SE, Orchard TR. Differences in inflammatory bowel disease phenotype between South Asians and Northern Europeans living in North West London, UK. Am J Gastroenterol. 2011;106:1281-1289. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 42] [Article Influence: 3.2] [Reference Citation Analysis (0)] |