Published online Jun 28, 2016. doi: 10.3748/wjg.v22.i24.5609
Peer-review started: March 13, 2016
First decision: March 31, 2016
Revised: April 12, 2016
Accepted: May 21, 2016
Article in press: May 23, 2016
Published online: June 28, 2016
AIM: To assess the use of dezocine combined with propofol for the anesthetization of patients undergoing indolent colonoscopy.
METHODS: A cross-sectional survey of patients undergoing indolent colonoscopy in the Xinjiang People’s Hospital was conducted from April 1 to April 30, 2015. The survey collected patient general information and anesthesia data, including overall medical experience and pain management. Thirty minutes after colonoscopy surgery, samples of venous blood were collected and the biochemical indicators of gastrointestinal function were analyzed.
RESULTS: There were 98 female and 62 male respondents. Indolent colonoscopy was found to be more suitable for mid to older-aged patients. The necessary conditions for the diagnosis of digestive diseases were required in 65 of the 73 inpatients. Adverse reactions to the intraoperative process included two cases of body movement and two cases of respiratory depression. Gastrin and vasoactive intestinal peptide levels were slightly increased. However, somatostatin and endothelin levels were slightly decreased.
CONCLUSION: This study revealed that dezocine combined with propofol can be successfully used for the anesthetization of indolent colonoscopy patients without pain and should be widely used.
Core tip: A cross-sectional survey of patients undergoing indolent colonoscopy was carried out to study the clinical effect of anesthetization by dezocine combined with propofol. Thirty minutes after colonoscopy surgery, samples of venous blood were collected and the biochemical indicators of gastrointestinal function were analyzed. Indolent colonoscopy was found to be more suitable for mid to older-aged patients. Gastrin and vasoactive intestinal peptide levels were slightly increased. However, somatostatin and endothelin levels were slightly decreased. This study revealed that dezocine combined with propofol can be successfully used for the anesthetization of indolent colonoscopy patients without pain and should be widely used.
- Citation: Xu BB, Zhao XL, Xu GP. Clinical study of anesthetization by dezocine combined with propofol for indolent colonoscopy. World J Gastroenterol 2016; 22(24): 5609-5615
- URL: https://www.wjgnet.com/1007-9327/full/v22/i24/5609.htm
- DOI: https://dx.doi.org/10.3748/wjg.v22.i24.5609
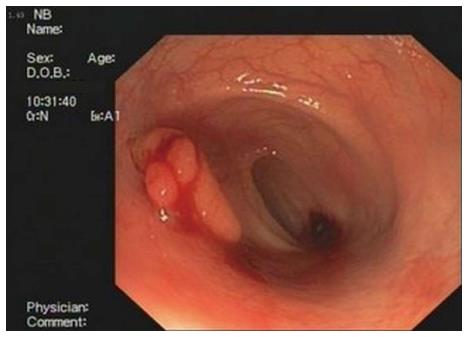
Colonoscopy is an endoscopic examination of the large intestine and the distal part of the small intestine. It provides a diagnosis and therapeutic opportunity for colorectal lesions[1-4]. At present, colonoscopy remains the gold standard investigation for inspecting colorectal lesions such as adenomas, cancer or inflammation. In many situations, it remains preferable to other imaging examinations such as computed tomography (CT) colonography or barium enema due to the capacity to intervene and sample or remove the pathology encountered.
Unlike sigmoidoscopy which can get to the distal portion (about 600 mm) of the colon, colonoscopy provides an investigation of the full colon (1200-1500 mm)[5,6]. The pain is not caused by the scope of the insertion but rather by the inflation of the colon to allow the inspection. The scope itself is essentially a long, flexible tube about a centimeter in diameter, i.e., around the diameter of the little finger, which is less than the diameter of an average stool[7-9].
Increasingly, doctors like to operate on totally anesthetized patients because it allows for a calmer examination without perceived pain or discomfort. Compared with general anesthesia, twilight sedation is safer and it also allows the patient to follow simple commands and even to watch the operation on a monitor. Therefore, twilight sedation is generally best and the operator should not rush, even although the examination may cause discomfort. Tens of millions of people need colonoscopies annually and yet many of them refuse because of concerns about the procedure[9]. Propofol is a short-acting, intravenously administered hypnotic/amnestic agent. It is usually used in the induction and maintenance of general anesthesia, sedation for mechanically ventilated adults and procedural sedation. Propofol is also used in veterinary medicine[9-11].
Recently, propofol has replaced sodium thiopental for the induction of anesthesia in many hospitals because anabiosis is faster and “clearer” using propofol. Propofol is not a pain medication so it may be combined with opioids such as fentanyl to alleviate pain. Whether this is always necessary is unclear.
Propofol has been known as “milk of amnesia” (a play on milk of magnesia) because the intravenous preparation has a milk-like appearance. It is on the World Health Organization Model List of Essential Medicines. More than 50 countries have approved it for use and generic versions are available[11-15]. Some patients may develop propofol infusion syndrome (PRIS), a rare syndrome that affects patients who undergo long-term treatment with high doses of propofol (> 4 mg/kg per hour for more than 24 h). It can result in cardiac failure, kidney failure, metabolic acidosis and rhabdomyolysis and is often fatal. High blood potassium, high blood triglycerides and liver enlargement, possibly caused by either direct mitochondrial respiratory chain inhibition or impaired mitochondrial fatty acid metabolism, are also key features. Children are more likely to develop PRIS and critically ill patients who receive glucocorticoids and catecholamines are at high risk. The main treatment is supportive therapy[9,16,17]. Early recognition of the syndrome and discontinuation of the propofol infusion reduces morbidity and mortality.
Dezocine is an opioid analgesic which was first synthesized in 1970. It is a mixed agonist/antagonist of opioid receptors and has the effects of analgesic action and euphoria. However, it is a silent antagonist of the κ-opioid receptor and thus has no side effects such as hallucinations or dysphoria[18]. Dezocine was patented by the American Home Products Corp. in 1978. Clinical trials ran from 1979 to 1985 before its approval by the United States Food and Drug Administration in 1986. The use of dezocine was discontinued in the United States in 2011 but it is commonly used after surgery in China.
This study analyzed the clinical manifestations after the administration of dezocine combined with propofol in the anesthetization of indolent colonoscopy patients to assess its effects on gastrointestinal function. The incidence of adverse reactions and improvement of patient tolerance were also studied.
A cross-sectional survey was used to collect epidemiological evidence. The use of regularly collected data provides large cross-sectional studies at little or no expense[19-21], which is an important advantage over other styles of epidemiological studies. A natural progression has been suggested from cheap cross-sectional studies of regularly collected data that can put forward hypotheses. However case-control studies test more specific hypotheses, cohort studies and trials cost much more and take much longer but provide stronger evidence. A cross-sectional survey is conducted to examine a specific group to determine whether alcohol consumption is correlated with cirrhosis being investigated. If alcohol is related to cirrhosis, this would support the hypothesis that alcohol may induce cirrhosis.
After obtaining institutional review board approval and informed consent from the participants or their guardians, 160 consecutive eligible patients previously diagnosed with indolent colonoscopy were enrolled in the study (Figure 1). All the patients had an ASA physical status of I or II and were aged between 1 and 68 years old.
All the experiments were performed under the supervision of the Patients’ Experimental Ethics Committee of the Beijing Army General Hospital (Beijing, China). The cross-sectional survey, conducted from April 1 to April 30, 2015, recruited patients undergoing indolent colonoscopy in the Xinjiang People’s Hospital. Patients with severe organ damage and drug allergies were excluded. This department does not operate on patients aged over 70 or under 1 year, or with a body mass index over 28 or under 18.
General epidemiological data and a history of neurological anesthetic drugs, including intravenous injection or oral drugs, were recorded.
After identification of the patients, intravenous access to the appropriate area was established. All patients received 5 mg of anisodamine, avoiding microvascular spasm. Baseline hemodynamic data were recorded on arrival in the operating room after placement of routine monitors.
Anesthesia was induced with an intravenous injection of 5 mg of dezocine. Ten minutes later, 1.5-2.0 mg/kg of propofol was administered intravenously to induce anesthesia. The dose of propofol was adjusted to maintain the heart rate and blood pressure within 20% of the pre-induction values. No opioids were given intraoperatively. All patients received standardized colonoscopy by a practicing physician.
The intraoperative index included the time the patient took to lose consciousness (from the induction of anesthesia until the eyelash conditioned reflex disappeared) and the total dosage of propofol.
The postoperative index included the length of time from the end of the colonoscopy surgery to the patient waking up and the patient’s pain score in the observation room 30 min after surgery. Adverse reactions were investigated during two phases: the incidence of body movements and respiratory depression in the intraoperative phase and the incidence of vomiting and dizziness or headache in the postoperative phase.
Samples of venous blood were collected thirty minutes after the colonoscopy surgery. The biochemical indicators gastrin, vasoactive intestinal peptide, somatostatin and endothelin were tested using the radioimmunoassay (RIA) method. The RIA kits were purchased from the Chinese People’s Liberation Army General Hospital, RIA Technology Development Center Institute (East Immunity Institute of Technology).
All data are represented as the means x ± SD (x ± s) of three or more independent experiments. Data with a positively skewed distribution were logarithmically transformed into a normal distribution. If the data were homogenous, analysis of variance, the Student-Newman-Keuls test and Pearson’s correlation were used. If the data were not homogenous, the Kruskal-Wallis test, Games-Howell test and Spearman’s correlation analysis were used. All the analyses were carried out using SPSS17.0 software (SPSS Inc., Chicago, IL, United States). Values below 0.05 were considered to be statistically significant.
From April 1 to April 30, 2015, 160 patients who had undergone dezocine combined with propofol in the anesthetization of indolent colonoscopy took part in the cross-sectional survey. Table 1 summarizes the patients’ characteristics. There were 98 females and 62 males; therefore, there were more than 1.6 times as many females as males. They ranged from 1 to 68 years of age, with a median of 43, an average of 48 and a mode of 52 years. These figures indicate that indolent colonoscopy was more common among mid to older-aged patients.
| Items | Value |
| Gender | |
| Male | 62 |
| Female | 98 |
| Age (yr) | |
| Median age | 43 |
| Maximum age | 68 |
| Minimum age | 1.3 |
| Average age | 48 |
| Modal age | 52 |
| Source | |
| Outpatients | 87 |
| Inpatients | 73 |
| Feedback from all patients | |
| Good medical experience | 92 |
| Normal medical experience | 58 |
| Bad medical experience | 9 |
There were 87 outpatients and 73 inpatients. For the purpose of health screening, more people chose indolent colonoscopy, especially the older patients. The necessary conditions for a diagnosis of digestive disease were required in 65 of the 73 inpatients (89.04%).
The patients’ feedback about their overall medical experience indicated that 92 had a good medical experience, 58 had an average experience, but 9 had a bad experience and 1 had a very bad experience, which was concentrated in the younger age group. Only one child had no statistical significance.
According to the American Society of Anesthesiologists (ASA) grading, 89 patients were classified as P1, 62 as P2, and 9 as P3, but no patient was classified as P4, 5 or 6. All diagnoses met the standard clinical symptoms of the ASA.
The ASA physical status class risk stratification system is dependent on comorbid conditions that are a threat to life or limit activity, thus helping to predicting preoperative risks. They are as follows: (1) P1 - normal healthy patient; (2) P2 - patient with mild systemic disease; (3) P3 - patient with severe systemic disease; (4) P4 - patient with severe systemic disease that is a constant threat to life; (5) P5 - moribund patient who is not expected to survive without the operation; and (6) P6 - declared brain-dead patient whose organs are being removed for donor purposes. All the patients were assessed by the anesthetist before surgery and not by self-reporting.
Among the 160 anesthetized patients, two episodes of postoperative emesis were recorded which occurred after propofol anesthesia. No patient required additional medication for pain in the post-anesthesia care or normal unit. The anesthesia experience perceived by the parents of the children was more appropriate for dezocine combined with propofol. However, three patients reported dizziness 30 min after the operation.
Intraoperative adverse reactions included two cases of body movement and two cases of respiratory depression. The assessment and pain management methods were based on the World Health Organization classification. One hundred and thirty-two patients reported a pain level under 3. No patients reported a higher level of pain; however, 12 patients reported feeling exhausted and fatigued. These results are shown in Table 2.
| Value | |
| Anesthesiologists’ (ASA) Grading | |
| P 1 | 89 |
| P 2 | 62 |
| P 3 | 9 |
| P 4, 5 or 6 | 0 |
| Adverse reactions | |
| Body movement | 2 |
| Respiratory depression | 2 |
| Vomiting | 2 |
| Dizziness | 3 |
| Exhaustion and fatigue | 12 |
| Pain management | |
| Level 0-3 | 132 |
| Level 4-6 | 28 |
| Above level 7-10 | 0 |
The mean duration of surgery was 52 ± 24 min, the induction time was 10 ± 4 min and the duration of maintenance was 60 ± 23 min.
Thirty minutes after the colonoscopy surgery, samples of venous blood were collected and four meaningful biochemical indicators of gastrointestinal function were assessed, as shown in Table 3. The results showed that gastrin and vasoactive intestinal peptide levels were slightly increased, whereas somatostatin and endothelin levels were slightly decreased.
| Detection value | Reference value | Comparison | |
| Gastrin (μg/mL) | 88.94 ± 18.77 | 63.12 ± 28.71 | Up |
| Vasoactive intestinal peptide (pg/mL) | 58.33 ± 4.22 | 35.25 ± 3.12 | Up |
| Somatostatin (pg/mL) | 79.42 ± 4.26 | 108.25 ± 5.12 | Down |
| Endothelin (pg/mL) | 36.77 ± 9.12 | 48.91 ± 10.1 | Down |
Gastrin can increase gastric mucosal blood flow and protect the gastric mucosa. Vasoactive intestinal peptide can cause the relaxation of the pyloric sphincter. The decrease in somatostatin and endothelin levels helped to inhibit the relaxation of the smooth gastric muscles.
General anesthesia refers to a medically induced coma with the lack of protective reflexes caused by one or more general anesthetic agents[1,12,21]. Various kinds of medications may be administered, with the aim of amnesia, analgesia, ensuring unconsciousness, relaxing the skeletal muscles and loss of control of the autonomic nervous system reflexes[9]. The optimal combination of these agents for any given patient and operation is usually chosen by the anesthesiologist or another provider, such as an anesthesiology assistant or nurse anesthetist, in consultation with the patient and the doctor conducting the operation.
Colonoscopy is the standard procedure for the diagnosis, screening, treatment and follow-up of many colorectal diseases[22,23]. Although some patients can tolerate the colonoscopy procedure without sedation or analgesics, the use of drugs in some patients is associated with stress. There are difficulties in determining an optimal dose for sedation and monitoring patients adequately during the procedure[24-27]. Many patients require intravenous benzodiazepines and opiates, which are associated with amnesic, anxiolytic and sedative properties. Combined administration of benzodiazepines and opioids has several undesirable effects, including a delay of several minutes from the time of injection before the drugs exert their effects, amnesia and the risk of respiratory depression[7,28,29].
Hospitals increasingly prefer to use fospropofol for colonoscopy. Fospropofol (trade name Lusedra) is an intravenous sedative-hypnotic agent. It is currently used for the sedation of adult patients undergoing diagnostic or therapeutic operations such as endoscopy. Some water-soluble prodrugs of propofol have been developed, of which fospropofol is known as the most fit for clinical development to date. Fospropofol is often administered combined with an opioid such as fentanyl. As a prodrug of propofol, it is metabolized into propofol by alkaline phosphatases. Theoretically, one millimole (mmol) of propofol may be generated for each mmol of fospropofol sodium administered; 1.86 mg of fospropofol sodium is the molar equivalent of 1 mg propofol[30-33].
Dezocine can be administered intravenously or intramuscularly. Dezocine is an effective painkiller compared with meperidine (pethidine) and a more effective analgesic than pentazocine but may cause greater respiratory depression. It is an effective drug for the treatment of pain but side effects such as dizziness restrict its clinical use and it also causes opioid withdrawal syndrome in patients already using other opioids[34].
A study conducted by the Department of Anesthesia, Xishan People’s Hospital of Wuxi City in Jiangsu province explored the clinical effect of dezocine combined with propofol in the anesthetization of 60 patients undergoing indolent enteroscopy between July 2012 and June 2014. The patients were randomly divided into a research group that received dezocine combined with propofol and a control group that received fentanyl combined with propofol[33-36]. The total dosage of propofol in the research group was less than that in the control group (P < 0.05), the awakening time in the research group was shorter than in the control group (P < 0.05) and the number of adverse effects during and after surgery was lower in the research group than in the control group (P < 0.05). Dezocine combined with propofol applied in the anesthetization of indolent enteroscopy can have a remarkable effect, improve operational safety and decrease the occurrence of adverse reactions. Our results were consistent with those of this study.
According to the results of a study by the Department of Anesthesiology at the First Hospital of Quanzhou, age was an important influence on the pharmacodynamics of propofol in patients receiving propofol combined with dezocine while undergoing colonoscopy[37]. However, the results from the Department of Gastroenterology at the Second People’s Hospital of Fujian province showed that endoscopic mucosal resection under painless colonoscopy shortened the recovery time, increased the success rate and improved the satisfaction rate of older patients who received propofol and fentanyl. Endoscopic mucosal resection under painless colonoscopy is an easy, safe and effective therapy for colorectal polyps.
Thirty minutes after colonoscopy surgery, samples of venous blood were collected and the biochemical indicators gastrin, vasoactive intestinal peptide, somatostatin and endothelin were tested. There was an increase in the plasma contents of gastrin and vasoactive intestinal peptide (P < 0.05) and a decrease in somatostatin and endothelin (P < 0.05) compared with the standard reference values[38-40].
Anesthesia with dezocine combined with propofol evidently increases gastric mucosal blood flow, suggesting that it has a regulative effect on gastrointestinal function. The use of dezocine combined with propofol might change plasma brain-gut peptides levels and may be useful.
Increasingly, doctors like to operate on totally anesthetized patients because it allows for a calmer examination without perceived pain or discomfort. Twilight sedation is safer than general anesthesia and allows the patient to follow simple commands and even to watch the operation on a monitor. Therefore, twilight sedation is generally best and the operator should not rush, even although the examination may cause discomfort. Tens of millions of adults need colonoscopies annually and yet many refuse because of concerns about the procedure.
This study assessed the use of dezocine combined with propofol for the anesthetization of patients undergoing indolent colonoscopy for the assessment of gastrointestinal function. A cross-sectional survey of patients undergoing indolent colonoscopy in the Xinjiang People’s Hospital was conducted from April 1 to April 30, 2015. The survey collected general information and anesthesia data, including overall medical experience and pain management.
Indolent colonoscopy was found to be more suitable for mid to older-aged patients. Somatostatin and endothelin levels were slightly decreased and patients had a good medical experience.
Gastrin and vasoactive intestinal peptide levels were slightly increased. However, somatostatin and endothelin levels were slightly decreased. This clinical study of dezocine combined with propofol indicates that it is a successful method for the anesthetization of indolent colonoscopy patients without pain and should therefore be widely used.
In this study, the authors assessed the use of dezocine combined with propofol for the anesthetization of patients undergoing indolent colonoscopy for the assessment of gastrointestinal function. The study collected general information and anesthesia data, including overall medical experience and pain management. This clinical study of dezocine combined with propofol indicates that it is a successful method for the anesthetization of indolent colonoscopy patients without pain and should therefore be widely used.
P- Reviewer: Arville B, Shimizu Y S- Editor: Gong ZM L- Editor: Roemmele A E- Editor: Ma S
| 1. | Triantafillidis JK, Merikas E, Nikolakis D, Papalois AE. Sedation in gastrointestinal endoscopy: current issues. World J Gastroenterol. 2013;19:463-481. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 135] [Cited by in F6Publishing: 143] [Article Influence: 13.0] [Reference Citation Analysis (3)] |
| 2. | Gasparović S, Rustemović N, Opacić M, Premuzić M, Korusić A, Bozikov J, Bates T. Clinical analysis of propofol deep sedation for 1,104 patients undergoing gastrointestinal endoscopic procedures: a three year prospective study. World J Gastroenterol. 2006;12:327-330. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 34] [Cited by in F6Publishing: 40] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 3. | IJspeert JE, Bevan R, Senore C, Kaminski MF, Kuipers EJ, Mroz A, Bessa X, Cassoni P, Hassan C, Repici A. Detection rate of serrated polyps and serrated polyposis syndrome in colorectal cancer screening cohorts: a European overview. Gut. 2016; Epub ahead of print. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 84] [Cited by in F6Publishing: 86] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 4. | Repici A, Pagano N, Hassan C, Carlino A, Rando G, Strangio G, Romeo F, Zullo A, Ferrara E, Vitetta E. Balanced propofol sedation administered by nonanesthesiologists: The first Italian experience. World J Gastroenterol. 2011;17:3818-3823. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 20] [Cited by in F6Publishing: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 5. | Davila RE, Rajan E, Adler DG, Egan J, Hirota WK, Leighton JA, Qureshi W, Zuckerman MJ, Fanelli R, Wheeler-Harbaugh J. ASGE Guideline: the role of endoscopy in the patient with lower-GI bleeding. Gastrointest Endosc. 2005;62:656-660. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 99] [Cited by in F6Publishing: 107] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 6. | Metwally M, Agresti N, Hale WB, Ciofoaia V, O’Connor R, Wallace MB, Fine J, Wang Y, Gross SA. Conscious or unconscious: the impact of sedation choice on colon adenoma detection. World J Gastroenterol. 2011;17:3912-3915. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 29] [Cited by in F6Publishing: 34] [Article Influence: 2.6] [Reference Citation Analysis (1)] |
| 7. | Zauber AG, Winawer SJ, O’Brien MJ, Lansdorp-Vogelaar I, van Ballegooijen M, Hankey BF, Shi W, Bond JH, Schapiro M, Panish JF. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med. 2012;366:687-696. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1952] [Cited by in F6Publishing: 2084] [Article Influence: 173.7] [Reference Citation Analysis (1)] |
| 8. | Hamdani U, Naeem R, Haider F, Bansal P, Komar M, Diehl DL, Kirchner HL. Risk factors for colonoscopic perforation: a population-based study of 80118 cases. World J Gastroenterol. 2013;19:3596-3601. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 52] [Cited by in F6Publishing: 49] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 9. | Eisen GM, Dominitz JA, Faigel DO, Goldstein JL, Kalloo AN, Petersen JL, Raddawi HM, Ryan ME, Vargo JJ, Young HS. Endoscopic therapy of anorectal disorders. Gastrointest Endosc. 2001;53:867-870. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Allen M, Leslie K, Hebbard G, Jones I, Mettho T, Maruff P. A randomized controlled trial of light versus deep propofol sedation for elective outpatient colonoscopy: recall, procedural conditions, and recovery. Can J Anaesth. 2015;62:1169-1178. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 32] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 11. | Peytremann-Bridevaux I, Arditi C, Froehlich F, O’Malley J, Fairclough P, Le Moine O, Dubois RW, Gonvers JJ, Schusselé Filliettaz S, Vader JP. Appropriateness of colonoscopy in Europe (EPAGE II). Iron-deficiency anemia and hematochezia. Endoscopy. 2009;41:227-233. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 12. | Uezono S, Goto T, Terui K, Ichinose F, Ishguro Y, Nakata Y, Morita S. Emergence agitation after sevoflurane versus propofol in pediatric patients. Anesth Analg. 2000;91:563-566. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 163] [Cited by in F6Publishing: 136] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 13. | Savides TJ, Jensen DM. Therapeutic endoscopy for nonvariceal gastrointestinal bleeding. Gastroenterol Clin North Am. 2000;29:465-487, vii. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 70] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 14. | Iwasaki J, Sano Y, Fu KI, Machida A, Okuno T, Kuwamura H, Yoshino T, Mera K, Kato S, Ohtsu A. Depressed-type (0-IIc) colorectal neoplasm in patients with family history of first-degree relatives with colorectal cancer: A cross-sectional study. World J Gastroenterol. 2006;12:3082-3087. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 1] [Cited by in F6Publishing: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 15. | Lin YL, Chiang JK, Lin SM, Tseng CE. Helicobacter pylori infection concomitant with metabolic syndrome further increase risk of colorectal adenomas. World J Gastroenterol. 2010;16:3841-3846. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 26] [Cited by in F6Publishing: 27] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 16. | Spinzi G, Fante MD, Masci E, Buffoli F, Colombo E, Fiori G, Ravelli P, Ceretti E, Minoli G. Lack of colonic neoplastic lesions in patients under 50 yr of age with hematochezia: a multicenter prospective study. Am J Gastroenterol. 2007;102:2011-2015. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 17] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 17. | Horiuchi A, Nakayama Y, Kajiyama M, Kato N, Kamijima T, Ichise Y, Tanaka N. Safety and effectiveness of propofol sedation during and after outpatient colonoscopy. World J Gastroenterol. 2012;18:3420-3425. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 25] [Cited by in F6Publishing: 28] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 18. | Bae T, Ha Y, Kim C, Lee J, Ha K, Shin S, Lee Y, Kang Y. Distribution of the colonoscopic adenoma detection rate according to age: is recommending colonoscopy screening for koreans over the age of 50 safe? Ann Coloproctol. 2015;31:46-51. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 19. | Ahn E, Son KY, Shin DW, Han MK, Lee H, An AR, Kim EH, Cho B. Perceived risk as a barrier to appropriate diagnosis of irritable bowel syndrome. World J Gastroenterol. 2014;20:18360-18366. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 4] [Cited by in F6Publishing: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Bjerregaard NC, Tøttrup A, Sørensen HT, Laurberg S. Diagnostic value of self-reported symptoms in Danish outpatients referred with symptoms consistent with colorectal cancer. Colorectal Dis. 2007;9:443-451. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 21. | Aydogmus MT, Türk HS, Oba S, Gokalp O. A comparison of different proportions of a ketamine-propofol mixture administered in a single injection for patients undergoing colonoscopy. Arch Med Sci. 2015;11:570-576. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 22. | Xie WQ, Li YY, Zie WJ, Yan JJ, Jiang CC, Kang ZM. Effect of patient’s age on propofol’s pharmacodynamics while combining with low dose fentanyly in colonoscopy. Linchuang Mazuixue Zazhi. 2014;30:462-465. [Cited in This Article: ] |
| 23. | Pasha SF, Shergill A, Acosta RD, Chandrasekhara V, Chathadi KV, Early D, Evans JA, Fisher D, Fonkalsrud L, Hwang JH. The role of endoscopy in the patient with lower GI bleeding. Gastrointest Endosc. 2014;79:875-885. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 145] [Cited by in F6Publishing: 127] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 24. | Heuss LT, Sugandha SP, Beglinger C. Carbon dioxide accumulation during analgosedated colonoscopy: comparison of propofol and midazolam. World J Gastroenterol. 2012;18:5389-5396. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 8] [Cited by in F6Publishing: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 25. | Tong GX, Chai J, Cheng J, Xia Y, Feng R, Zhang L, Wang DB. Diagnostic value of rectal bleeding in predicting colorectal cancer: a systematic review. Asian Pac J Cancer Prev. 2014;15:1015-1021. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 26. | Sun XB. Clinical study of dezocien combined with propofol in the anesthetization of indolent enteroscope. Zhongguo Dangdai Yixue. 2015;22:124-126. [Cited in This Article: ] |
| 27. | Choe EK, Kim D, Kim HJ, Park KJ. Association of visceral obesity and early colorectal neoplasia. World J Gastroenterol. 2013;19:8349-8356. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 23] [Cited by in F6Publishing: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 28. | Lozano-Maya M, Ponferrada-Díaz A, González-Asanza C, Nogales-Rincón O, Senent-Sánchez C, Pérez-de-Ayala V, Jiménez-Aleixandre P, Cos-Arregui E, Menchén-Fernández-Pacheco P. Usefulness of colonoscopy in ischemic colitis. Rev Esp Enferm Dig. 2010;102:478-483. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 29. | Gan T, Yang JL, Wu JC, Wang YP, Yang L. When and why a colonoscopist should discontinue colonoscopy by himself? World J Gastroenterol. 2015;21:7834-7841. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 30. | Leggett B, Whitehall V. Role of the serrated pathway in colorectal cancer pathogenesis. Gastroenterology. 2010;138:2088-2100. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 677] [Cited by in F6Publishing: 678] [Article Influence: 48.4] [Reference Citation Analysis (1)] |
| 31. | Fanti L, Gemma M, Agostoni M, Rossi G, Ruggeri L, Azzolini ML, Dabizzi E, Beretta L, Testoni PA. Target Controlled Infusion for non-anaesthesiologist propofol sedation during gastrointestinal endoscopy: The first double blind randomized controlled trial. Dig Liver Dis. 2015;47:566-571. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 32. | Klare P, Huth R, Haller B, Huth M, Weber A, Schlag C, Reindl W, Schmid RM, von Delius S. Patient position and hypoxemia during propofol sedation for colonoscopy: a randomized trial. Endoscopy. 2015;47:1159-1166. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 33. | Nikpour S, Ali Asgari A. Colonoscopic evaluation of minimal rectal bleeding in average-risk patients for colorectal cancer. World J Gastroenterol. 2008;14:6536-6540. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 22] [Cited by in F6Publishing: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 34. | Jass JR. Classification of colorectal cancer based on correlation of clinical, morphological and molecular features. Histopathology. 2007;50:113-130. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 955] [Cited by in F6Publishing: 952] [Article Influence: 56.0] [Reference Citation Analysis (0)] |
| 35. | Baykal Tutal Z, Gulec H, Derelı N, Babayıgıt M, Kurtay A, Inceoz H, Horasanlı E. Propofol-ketamine combination: a choice with less complications and better hemodynamic stability compared to propofol? On a prospective study in a group of colonoscopy patients. Ir J Med Sci. 2015; Epub ahead of print. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 36. | Weng HF, Hu JF, Yang JY, Wang QY, Wan LT. Analysis of complications of painless gastrointestinal endoscopy in the diagnosis and treatment. Chendou Yixueyuan Xuebao. 2015;10:324-326. [Cited in This Article: ] |
| 37. | Sun DY, Huang YX, Gao W, Chu ZH, Wang QL. Effects of electroacupuncture on plasma leels of brain-gut peptides in dogs. Jiefangjun Yixue Zazhi. 2002;27:997-998. [Cited in This Article: ] |
| 38. | Goudra B, Singh PM, Gouda G, Borle A, Carlin A, Yadwad A. Propofol and non-propofol based sedation for outpatient colonoscopy-prospective comparison of depth of sedation using an EEG based SEDLine monitor. J Clin Monit Comput. 2015; Epub ahead of print. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 39. | Kim YW, Choi H, Kim GJ, Ryu SJ, Park SM, Kim JS, Ji JS, Kim BW, Lee BI, Choi MG. [Role of Colonoscopy in Patients with Hematochezia]. Korean J Gastroenterol. 2016;67:87-91. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 40. | Rees CJ, Ngu WS. Temporal trends and variability of colonoscopy performance in gastroenterology practice. Endoscopy. 2016;48:213-214. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |