Introduction
Heterotopic ossification (HO) is the growth of bone in soft tissue, outside its usual and normal anatomical locations. It is commonly seen following major trauma and burns. A handful of cases of HO have been described in the setting of free tissue transfer, with the majority occurring in osseous flaps, and only one previous case in a radial artery free flap (RAFF).
Wood and colleagues performed a 10-year retrospective analysis of osseous free flaps and found that 21 per cent of incidentally imaged fibula free flaps (FFF) had evidence of HO, predominantly around the vascular pedicle. In their study, there were no cases in the osteocutaneous RAFF and scapular flaps.1 They posited that HO may be a unique property of the FFF. Contrary to this, there has been one reported case of HO in a fasciocutaneous RAFF, however this was in the substance of the flap rather than surrounding the vascular pedicle.2
A further case of HO in a RAFF is presented. To our knowledge, this is the first described case of HO surrounding the vascular pedicle of this flap, rather than in the substance.
Case
We present a 38-year-old man who underwent reconstruction of a recurrent anterior palatal fistula with a RAFF. His history was of bilateral cleft lip and palate, for which he underwent primary lip and palate repair, alveolar bone grafting, septoplasty, and previous upper lip revision. His medical history was significant only for obstructive sleep apnoea treated with Continuous positive airway pressure (CPAP) and mild asthma treated with salbutamol.
The patient presented to our service for management of his recurrent anterior palatal fistula, which was causing oro-nasal regurgitation and hypernasal speech. On examination, he had a slit-like anterior palatal fistula (Pittsburgh IV–V).3 He was partially edentulous due to untreated dental caries.
Repair of his fistula with a superiorly based facial artery myomucosal (FAMM) flap was attempted, however, a recurrent symptomatic anterior hard palate fistula remained (Figure 1a).
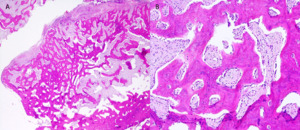
A RAFF was chosen for his salvage reconstruction. A 2 cm wide fascia-only RAFF was inset with an overlying full thickness skin graft (FTSG). The pedicle was tunnelled submucosally around the posterior maxillary alveolus and an anastomosis carried out to the left facial artery and vein via a short submandibular incision. His postoperative course was complicated by haemorrhage from the region of the flap pedicle where it ran posterior to the maxillary alveolus two weeks postoperatively, requiring return to theatre to cauterise the bleeding. He underwent early debulking of the flap at nine weeks postoperatively, at which time a large segment of the pedicle was noted to be ossified. Clinically, he had a moderate degree of trismus and localised left-sided pain on mouth opening. The ossified tissue tented the submucosal tunnel that extended to the buccal region and so was resected. On histopathological examination this tissue was found to be metaplastic, immature woven bone, consistent with heterotopic ossification of the flap pedicle (Figure 2). At follow-up three months postoperatively, he had no evidence of recurrence of his fistula and no new issues related to his RAFF (Figure 1b). His trismus and pain were resolved, and on examination there was no evidence of recurrent HO.
Discussion
The development of HO is an under-reported complication of reconstructive microsurgery. While mostly asymptomatic, HO can present as a head and neck mass or lead to pain and trismus. Symptoms from HO prompted excision in 10–20 per cent of reported cases.1,4
The incidence of HO has been reported as 4–27 per cent in FFF,5,6 with isolated cases in other free flaps also described.2,4 This likely underestimates the true incidence as postoperative imaging is not routinely performed after all free tissue transfers.
This case invites further consideration of the pathophysiology of HO, as the circumstances deviate from those in other reported cases of HO in free flaps. The pathophysiology of HO is currently poorly understood. The prevailing theory involves overactivation of the bone morphogenetic protein (BMP) cascade resulting in endochondral ossification via stimulation of mesenchymal stem cell differentiation to osteoblasts.7 Bone morphogenetic protein is osteoinductive and is crucial in the initiation of bone formation.8 In a free flap pedicle, the widely accepted pathophysiological theory is that this process is enhanced because of the periosteum included with the flap pedicle during subperiosteal dissection of most FFF. Tarsitano and colleagues highlighted this in their study demonstrating that dissection of periosteum from the FFF vascular pedicle can mitigate the risk of HO.9 While this may explain HO in FFF, it does not account for cases in flaps without periosteum. Alternatively, fracture repair theory, mechanical stress and blood flow theory have been proposed in the literature as causes of HO.10 However, none of these theories fit with our case due to the absence of healing bone and significant mechanical stress, and no marked discrepancy in perfusion between donor and host tissue. In the only other reported case of HO in a RAFF,2 bone formation was seen in the body of the flap as opposed to the pedicle, attributed by the authors to the dissection of periosteum off the radial styloid and subsequent transfer into host tissue.
Common to all cases of HO is the initiation of an inflammatory response due to trauma or surgery.7 This may be the only clear link between the presented case and manifestations of HO in alternate clinical settings. It is speculated that the prolonged inflammatory response around the pedicle propagated by the procedure to arrest haemorrhage may have contributed to HO formation in this case.
Conclusion
To our knowledge this is the first described case of HO of the pedicle of a RAFF, and the first description of HO after cleft palate reconstruction. This case is inconsistent with the current leading theories of HO development in free flaps without periosteum. We speculate that further inflammatory stimulus related to an emergent operation to arrest postoperative haemorrhage may have contributed to this unusual complication.
Patient consent
Patients/guardians have given informed consent to the publication of images and/or data.
Disclosure
The authors have no financial or commercial conflicts of interest to disclose.
Funding declaration
The authors received no financial support for the research, authorship, and/or publication of this article.
Revised: 2021 May 18 AEST