The Spicy Story of Cannabimimetic Indoles
Abstract
:1. Introduction: Pravadoline and the Discovery of Aminoalkylindole Analgesics
2. Aminoalkylindoles and Cannabinoids: Structure—Activity Relationship Studies in Search of a Common Pharmacophore
3. The Quest for Selective CB2 Cannabinoid Receptor Ligands
3.1. CB2-Selective Indole Agonists
3.1.1. JWH-015 and Analogs (1-Propyl-2-methyl-3-(1-naphthoyl) indole)
3.1.2. L768242/GW405833 (1-(2,3-Dichlorobenzoyl)-2-methyl-3-(2-[1-morpholine] ethyl)-5-methoxyindole)
3.1.3. AM1241 ((R-) or (S-) 3-(2-Iodo-5-nitrobenzoyl)-1-(1-methyl-2-piperidinylmethyl)-1H-indole)
3.1.4. BMS Series and A796260 from 1-Alkyl-3-keto Indole Series
3.2. CB2-Selective Indole Antagonists
3.2.1. AM630 6-Iodo-Pravadoline
3.2.2. BML190
3.3. CB2-Selective WIN55212-2 and AAI Ligand Interactions with the CB2 Receptor
4. What Additional Targets Exist for Aminoalkylindoles?
4.1. Non-CB1, Non-CB2 Targets for WIN55212-2
4.2. Putative Alkyl Indole Receptors
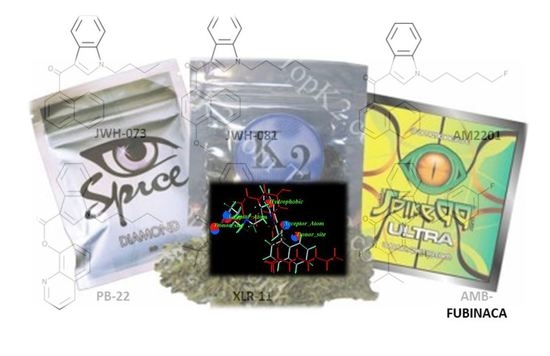
5. The Ultimate Diversion of Cannabimimetic Indoles: Spice/K2
- 2-(3-hydroxycyclohexyl)phenol with substitution at the 5-position of the phenolic ring by alkyl or alkenyl, whether or not substituted on the cyclohexyl ring to any extent.
- 3-(1-naphthoyl)indole or 3-(1-naphthylmethane)indole by substitution at the nitrogen atom of the indole ring, whether or not further substituted on the indole ring to any extent, whether or not substituted on the naphthoyl or naphthyl ring to any extent.
- 3-(1-naphthoyl)pyrrole by substitution at the nitrogen atom of the pyrrole ring, whether or not further substituted in the pyrrole ring to any extent, whether or not substituted on the naphthoyl ring to any extent.
- 1-(1-naphthylmethylene)indene by substitution of the 3-position of the indene ring, whether or not further substituted in the indene ring to any extent, whether or not substituted on the naphthyl ring to any extent.
- 3-phenylacetylindole or 3-benzoylindole by substitution at the nitrogen atom of the indole ring, whether or not further substituted in the indole ring to any extent, whether or not substituted on the phenyl ring to any extent.”
6. Conclusions: Scientists and Entrepreneurs: Who Takes Social Responsibility?
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Howlett, A.C. Inhibition of neuroblastoma adenylate cyclase by cannabinoid and nantradol compounds. Life Sci. 1984, 35, 1803–1810. [Google Scholar] [CrossRef]
- Howlett, A.; Fleming, R.M. Cannabinoid inhibition of adenylate cyclase. Pharmacology of the response in neuroblastoma cell membranes. Mol. Pharmacol. 1984, 26, 532–538. [Google Scholar]
- Milne, G.M., Jr.; Johnson, M.R. Levonantradol: A role for central prostanoid mechanisms? J. Clin. Pharmacol. 1981, 21, 367s–374s. [Google Scholar] [CrossRef]
- Johnson, M.R.; Melvin, L.S.; Althuis, T.H.; Bindra, J.S.; Harbert, C.A.; Milne, G.M.; Weissman, A. Selective and Potent Analgetics Derived from Cannabinoids. J. Clin. Pharmacol. 1981, 21, 271S–282S. [Google Scholar] [CrossRef]
- Jain, A.K.; Ryan, J.R.; McMahon, F.G.; Smith, G. Evaluation of Intramuscular Levonantradol and Placebo in Acute Postoperative Pain. J. Clin. Pharmacol. 1981, 21, 320S–326S. [Google Scholar] [CrossRef]
- Cronin, C.M.; Sallan, S.E.; Gelber, R.; Lucas, V.S.; Laszlo, J. Antiemetic Effect of Intramuscular Levonantradol in Patients Receiving Anticancer Chemotherapy. J. Clin. Pharmacol. 1981, 21, 43S–50S. [Google Scholar] [CrossRef]
- Laszlo, J.; Lucas, V.S.; Hanson, D.C.; Cronin, C.M.; Sallan, S.E. Levonantradol for Chemotherapy-Induced Emesis: Phase I-II Oral Administration. J. Clin. Pharmacol. 1981, 21, 51S–56S. [Google Scholar] [CrossRef]
- Sheidler, V.R.; Ettinger, D.S.; Diasio, R.B.; Enterline, J.P.; Brown, M.D. Double-Blind Multiple-Dose Crossover Study of the Antiemetic Effect of Intramuscular Levonantradol Compared to Prochlorperazine. J. Clin. Pharmacol. 1984, 24, 155–159. [Google Scholar] [CrossRef]
- Stambaugh, J.E.; McAdams, J.; Vreeland, F. Dose Ranging Evaluation of the Antiemetic Efficacy and Toxicity of Intramuscular Levonantradol in Cancer Subjects with Chemotherapy-Induced Emesis. J. Clin. Pharmacol. 1984, 24, 480–485. [Google Scholar] [CrossRef]
- Special Issue: Overview on the Current Status of Therapeutic Opportunities in Cannabinoid Research. J. Clin. Pharmacol. 1981, 21, 1S–494S.
- Howlett, A. Cannabinoid inhibition of adenylate cyclase. Biochemistry of the response in neuroblastoma cell membranes. Mol. Pharmacol. 1985, 27, 429–436. [Google Scholar]
- Howlett, A.; Johnson, M.R.; Melvin, L.S.; Milne, G.M. Nonclassical cannabinoid analgetics inhibit adenylate cyclase: Development of a cannabinoid receptor model. Mol. Pharmacol. 1988, 33, 297–302. [Google Scholar]
- Howlett, A.C.; Qualy, J.M.; Khachatrian, L.L. Involvement of Gi in the inhibition of adenylate cyclase by cannabimimetic drugs. Mol. Pharmacol. 1986, 29, 307–313. [Google Scholar]
- Devane, W.A.; Dysarz, F.A.; Johnson, M.R.; Melvin, L.S.; Howlett, A. Determination and characterization of a cannabinoid receptor in rat brain. Mol. Pharmacol. 1988, 34, 605–613. [Google Scholar]
- Howlett, A.; Bidaut-Russell, M.; Devane, W.A.; Melvin, L.S.; Johnson, M.; Herkenham, M. The cannabinoid receptor: Biochemical, anatomical and behavioral characterization. Trends Neurosci. 1990, 13, 420–423. [Google Scholar] [CrossRef]
- Howlett, A.C.; Johnson, M.R.; Melvin, L.S. Classical and Nonclassical Cannabinoids: Mechanism of Action-Brain Binding. NIDA Res. Monogr. 1990, 96, 100–111. [Google Scholar]
- Haubrich, D.R.; Ward, S.J.; Baizman, E.; Bell, M.R.; Bradford, J.; Ferrari, R.; Miller, M.; Perrone, M.; Pierson, A.K.; Saelens, J.K. Pharmacology of pravadoline: A new analgesic agent. J. Pharmacol. Exp. Ther. 1990, 255, 511–522. [Google Scholar]
- Bell, M.R.; D’Ambra, T.E.; Kumar, V.; Eissenstat, M.A.; Herrmann, J.L.; Wetzel, J.R.; Rosi, D.; Philion, R.E.; Daum, S.J. Antinociceptive (aminoalkyl)indoles. J. Med. Chem. 1991, 34, 1099–1110. [Google Scholar] [CrossRef]
- Ward, S.J.; Mastriani, D.; Casiano, F.; Arnold, R. Pravadoline: Profile in isolated tissue preparations. J. Pharmacol. Exp. Ther. 1990, 255, 1230–1239. [Google Scholar]
- Pacheco, M.; Childers, S.R.; Arnold, R.; Casiano, F.; Ward, S.J. Aminoalkylindoles: Actions on specific G-protein-linked receptors. J. Pharmacol. Exp. Ther. 1991, 257, 170–183. [Google Scholar]
- D’Ambra, T.E.; Estep, K.G.; Bell, M.R.; Eissenstat, M.A.; Josef, K.A.; Ward, S.J.; Haycock, D.A.; Baizman, E.R.; Casiano, F.M.; Beglin, N.C.; et al. Conformationally restrained analogues of pravadoline: Nanomolar potent, enantioselective, (aminoalkyl)indole agonists of the cannabinoid receptor. J. Med. Chem. 1992, 35, 124–135. [Google Scholar] [CrossRef] [PubMed]
- Compton, D.R.; Gold, L.H.; Ward, S.J.; Balster, R.L.; Martin, B.R. Aminoalkylindole analogs: Cannabimimetic activity of a class of compounds structurally distinct from delta 9-tetrahydrocannabinol. J. Pharmacol. Exp. Ther. 1992, 263, 1118–1126. [Google Scholar] [PubMed]
- Ward, S.J.; Baizman, E.; Bell, M.; Childers, S.; D’Ambra, T.; Eissenstat, M.; Estep, K.; Haycock, D.; Howlett, A.; Luttinger, D.; et al. Aminoalkylindoles (AAIs): A new route to the cannabinoid receptor? NIDA Res. Monogr. 1990, 105, 425–426. [Google Scholar] [PubMed]
- Kuster, J.E.; Stevenson, J.I.; Ward, S.J.; D’Ambra, T.E.; Haycock, D.A. Aminoalkylindole binding in rat cerebellum: Selective displacement by natural and synthetic cannabinoids. J. Pharmacol. Exp. Ther. 1993, 264, 1352–1363. [Google Scholar]
- Yamada, K.; Rice, K.C.; Flippen-Anderson, J.L.; Eissenstat, M.A.; Ward, S.J.; Johnson, M.R.; Howlett, A.C. (Aminoalkyl)indole Isothiocyanates as Potential Electrophilic Affinity Ligands for the Brain Cannabinoid Receptor. J. Med. Chem. 1996, 39, 1967–1974. [Google Scholar] [CrossRef] [PubMed]
- Jansen, E.M.; Haycock, D.A.; Ward, S.J.; Seybold, V.S. Distribution of cannabinoid receptors in rat brain determined with aminoalkylindoles. Brain Res. 1992, 575, 93–102. [Google Scholar] [CrossRef]
- Zhang, Q.; Ma, P.; Iszard, M.; Cole, R.B.; Wang, W.; Wang, G. In Vitro Metabolism ofR(+)-[2,3-Dihydro-5-methyl-3-[(morpholinyl)methyl]pyrrolo [1,2,3-de]1,4-benzoxazinyl]-(1-naphthalenyl) methanone mesylate, a Cannabinoid Receptor Agonist. Drug Metab. Dispos. 2002, 30, 1077–1086. [Google Scholar] [CrossRef] [Green Version]
- Collins, J.C.; Gwilt, J.R. The Life Cycle of Sterling Drug, Inc. Bull. Hist. Chem. 2000, 25, 22–27. [Google Scholar]
- Huffman, J.W. Cannabimimetic indoles, pyrroles and indenes. Curr. Med. Chem. 1999, 6, 705–720. [Google Scholar]
- Huffman, J.W.; Padgett, L.W. Recent developments in the medicinal chemistry of cannabimimetic indoles, pyrroles and indenes. Curr. Med. Chem. 2005, 12, 1395–1411. [Google Scholar] [CrossRef]
- Shim, J.Y.; Collantes, E.R.; Welsh, W.J.; Howlett, A.C. Unified pharmacophoric model for cannabinoids and aminoalkylindoles derived from molecular superimpositioin of CB1 cannabinoid receptor agonists CP55244 and WIN55212-2. In Rational Drug Design: Novel Methodology and Practical Applications; Parrill, A.L., Ed.; American Chemical Society: Washington, DC, USA, 1999; pp. 165–184. [Google Scholar]
- Shim, J.-Y.; Collantes, E.R.; Welsh, W.J.; Subramaniam, B.; Howlett, A.C.; Eissenstat, M.A.; Ward, S.J. Three-Dimensional Quantitative Structure–Activity Relationship Study of the Cannabimimetic (Aminoalkyl)indoles Using Comparative Molecular Field Analysis. J. Med. Chem. 1998, 41, 4521–4532. [Google Scholar] [CrossRef]
- Eissenstat, M.A.; Bell, M.R.; D’Ambra, T.E.; Alexander, E.J.; Daum, S.J.; Ackerman, J.H.; Gruett, M.D.; Kumar, V.; Estep, K.G. Aminoalkylindoles: Structure-Activity Relationships of Novel Cannabinoid Mimetics. J. Med. Chem. 1995, 38, 3094–3105. [Google Scholar] [CrossRef]
- D’Ambra, T.E.; Eissenstat, M.A.; Abt, J.; Ackerman, J.H.; Bacon, E.R.; Bell, M.R.; Carabateas, P.M.; Josef, K.A.; Kumar, V.; Weaver, J.D.; et al. C-Attached aminoalkylindoles: Potent cannabinoid mimetics. Bioorg. Med. Chem. Lett. 1996, 6, 17–22. [Google Scholar] [CrossRef]
- Shim, J.-Y.; Welsh, W.J.; Cartier, E.; Edwards, J.L.; Howlett, A. Molecular Interaction of the Antagonist N-(Piperidin-1-yl)-5-(4-chlorophenyl)-1-(2,4-dichlorophenyl)-4-methyl-1H-pyrazole-3-carboxamide with the CB1 Cannabinoid Receptor. J. Med. Chem. 2002, 45, 1447–1459. [Google Scholar] [CrossRef]
- Xiet, X.-Q.; Eissenstat, M.; Makriyannis, A. Common cannabimimetic pharmacophoric requirements between aminoalkyl indoles and classical cannabinoids. Life Sci. 1995, 56, 1963–1970. [Google Scholar] [CrossRef]
- Xie, X.-Q.; Han, X.-W.; Chen, J.-Z.; Eissenstat, M.; Makriyannis, A. High-resolution NMR and computer modeling studies of the cannabimimetic aminoalkylindole prototype WIN-55212-2. J. Med. Chem. 1999, 42, 4021–4027. [Google Scholar] [CrossRef]
- Wiley, J.; Compton, D.R.; Dai, D.; Lainton, J.A.; Phillips, M.; Huffman, J.W.; Martin, B.R. Structure-activity relationships of indole- and pyrrole-derived cannabinoids. J. Pharmacol. Exp. Ther. 1998, 285, 995–1004. [Google Scholar]
- Huffman, J.W.; Dai, D.; Martin, B.R.; Compton, D.R. Design, Synthesis and Pharmacology of Cannabimimetic Indoles. Bioorg. Med. Chem. Lett. 1994, 4, 563–566. [Google Scholar] [CrossRef]
- Huffman, J.W.; Lu, J.; Dai, D.; Kitaygorodskiy, A.; Wiley, J.L.; Martin, B.R. Synthesis and pharmacology of a hybrid cannabinoid. Bioorg. Med. Chem. 2000, 8, 439–447. [Google Scholar] [CrossRef]
- Reggio, P.H.; Basu-Dutt, S.; Barnett-Norris, J.; Castro, M.T.; Hurst, W.P.; Seltzman, H.H.; Roche, M.J.; Gilliam, A.F.; Thomas, B.F.; Stevenson, L.A.; et al. The Bioactive Conformation of Aminoalkylindoles at the Cannabinoid CB1 and CB2 Receptors: Insights Gained from (E)- and (Z)-Naphthylidene Indenes. J. Med. Chem. 1998, 41, 5177–5187. [Google Scholar] [CrossRef]
- Huffman, J.W.; Mabon, R.; Wu, M.-J.; Lu, J.; Hart, R.; Hurst, D.P.; Reggio, P.H.; Wiley, J.L.; Martin, B.R. 3-Indolyl-1-naphthylmethanes: New cannabimimetic indoles provide evidence for aromatic stacking interactions with the CB1 cannabinoid receptor. Bioorg. Med. Chem. 2003, 11, 539–549. [Google Scholar] [CrossRef]
- Song, Z.H.; Bonner, T.I. A lysine residue of the cannabinoid receptor is critical for receptor recognition by several agonists but not WIN55212-2. Mol. Pharmacol. 1996, 49, 891–896. [Google Scholar] [PubMed]
- Tao, Q.; Abood, M. Mutation of a highly conserved aspartate residue in the second transmembrane domain of the cannabinoid receptors, CB1 and CB2, disrupts G-protein coupling. J. Pharmacol. Exp. Ther. 1998, 285, 651–658. [Google Scholar] [PubMed]
- McAllister, S.D.; Tao, Q.; Barnett-Norris, J.; Buehner, K.; Hurst, D.P.; Guarnieri, F.; Reggio, P.H.; Harmon, K.W.N.; Cabral, G.A.; Abood, M.E. A critical role for a tyrosine residue in the cannabinoid receptors for ligand recognition. Biochem. Pharmacol. 2002, 63, 2121–2136. [Google Scholar] [CrossRef]
- Song, Z.H.; Slowey, C.A.; Hurst, D.P.; Reggio, P.H. The difference between the CB(1) and CB(2) cannabinoid receptors at position 5.46 is crucial for the selectivity of WIN55212-2 for CB(2). Mol. Pharmacol. 1999, 56, 834–840. [Google Scholar]
- Shim, J.-Y.; Howlett, A.C. WIN55212-2 Docking to the CB1 Cannabinoid Receptor and Multiple Pathways for Conformational Induction. J. Chem. Inf. Model. 2006, 46, 1286–1300. [Google Scholar] [CrossRef] [PubMed]
- Shim, J.-Y.; Howlett, A.C. Steric Trigger as a Mechanism for CB1 Cannabinoid Receptor Activation. J. Chem. Inf. Comput. Sci. 2004, 44, 1466–1476. [Google Scholar] [CrossRef]
- Shim, J.-Y.; Welsh, W.J.; Howlett, A.C. Homology model of the CB1 cannabinoid receptor: Sites critical for nonclassical cannabinoid agonist interaction. Biopolymers 2003, 71, 169–189. [Google Scholar] [CrossRef]
- Guindon, J.; Hohmann, A.G. Cannabinoid CB2 receptors: A therapeutic target for the treatment of inflammatory and neuropathic pain. Br. J. Pharmacol. 2008, 153, 319–334. [Google Scholar] [CrossRef] [Green Version]
- Beltramo, M. Cannabinoid Type 2 Receptor as a Target for Chronic-Pain. Mini-Rev. Med. Chem. 2009, 9, 11–25. [Google Scholar] [CrossRef]
- Atwood, B.K.; Straiker, A.; Mackie, K. CB2: Therapeutic target-in-waiting. Prog. Neuropsychopharmacol. Biol. Psychiatry 2012, 38, 16–20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huffman, J.W. CB2 receptor ligands. Mini-Rev. Med. Chem. 2005, 5, 641–649. [Google Scholar] [CrossRef] [PubMed]
- Huffman, J.W. The Search for Selective Ligands for the CB2 Receptor. Curr. Pharm. Des. 2000, 6, 1323–1337. [Google Scholar] [CrossRef] [PubMed]
- Huffman, J.W.; Marriott, K.-S.C. Recent Advances in the Development of Selective Ligands for the Cannabinoid CB2 Receptor. Curr. Top. Med. Chem. 2008, 8, 187–204. [Google Scholar] [CrossRef] [PubMed]
- Felder, C.C.; Joyce, K.E.; Briley, E.M.; Mansouri, J.; Mackie, K.; Blond, O.; Lai, Y.; Ma, A.L.; Mitchell, R.L. Comparison of the pharmacology and signal transduction of the human cannabinoid CB1 and CB2 receptors. Mol. Pharmacol. 1995, 48, 443–450. [Google Scholar] [PubMed]
- Showalter, V.M.; Compton, D.R.; Martin, B.R.; Abood, M. Evaluation of binding in a transfected cell line expressing a peripheral cannabinoid receptor (CB2): Identification of cannabinoid receptor subtype selective ligands. J. Pharmacol. Exp. Ther. 1996, 278, 989–999. [Google Scholar]
- Aung, M.M.; Griffin, G.; Huffman, J.W.; Wu, M.-J.; Keel, C.; Yang, B.; Showalter, V.M.; Abood, M.; Martin, B.R. Influence of the N-1 alkyl chain length of cannabimimetic indoles upon CB1 and CB2 receptor binding. Drug Alcohol Depend. 2000, 60, 133–140. [Google Scholar] [CrossRef]
- Huffman, J.W.; Zengin, G.; Wu, M.J.; Lu, J.; Hynd, G.; Bushell, K.; Thompson, A.L.S.; Bushell, S.; Tartal, C.; Hurst, D.P.; et al. Structure-activity relationships for 1-alkyl-3-(1-naphthoyl)indoles at the cannabinoid CB(1) and CB(2) receptors: Steric and electronic effects of naphthoyl substituents. New highly selective CB(2) receptor agonists. Bioorg. Med. Chem. 2005, 13, 89–112. [Google Scholar] [CrossRef]
- Wiley, J.L.; Smith, V.J.; Chen, J.; Martin, B.R.; Huffman, J.W. Synthesis and pharmacology of 1-alkyl-3-(1-naphthoyl)indoles: Steric and electronic effects of 4- and 8-halogenated naphthoyl substituents. Bioorg. Med. Chem. 2012, 20, 2067–2081. [Google Scholar] [CrossRef] [Green Version]
- Gallant, M.; Dufresne, C.; Gareau, Y.; Guay, D.; Leblanc, Y.; Prasit, P.; Rochette, C.; Sawyer, N.; Slipetz, D.M.; Tremblay, N.; et al. New class of potent ligands for the human peripheral cannabinoid receptor. Bioorg. Med. Chem. Lett. 1996, 6, 2263–2268. [Google Scholar] [CrossRef]
- Valenzano, K.J.; Tafesse, L.; Lee, G.; Harrison, J.E.; Boulet, J.M.; Gottshall, S.L.; Mark, L.; Pearson, M.S.; Miller, W.; Shan, S.; et al. Pharmacological and pharmacokinetic characterization of the cannabinoid receptor 2 agonist, GW405833, utilizing rodent models of acute and chronic pain, anxiety, ataxia and catalepsy. Neuropharmacology 2005, 48, 658–672. [Google Scholar] [CrossRef] [PubMed]
- Clayton, N.; Marshall, F.H.; Bountra, C.; O’Shaughnessy, C.T. CB1 and CB2 cannabinoid receptors are implicated in inflammatory pain. Pain 2002, 96, 253–260. [Google Scholar] [CrossRef]
- Beltramo, M.; Bernardini, N.; Bertorelli, R.; Campanella, M.; Nicolussi, E.; Fredduzzi, S.; Reggiani, A. CB2 receptor-mediated antihyperalgesia: Possible direct involvement of neural mechanisms. Eur. J. Neurosci. 2006, 23, 1530–1538. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, M.M.; Deng, H.; Zvonok, A.; Cockayne, D.A.; Kwan, J.; Mata, H.P.; Vanderah, T.W.; Lai, J.; Porreca, F.; Makriyannis, A.; et al. Activation of CB2 cannabinoid receptors by AM1241 inhibits experimental neuropathic pain: Pain inhibition by receptors not present in the CNS. Proc. Natl. Acad. Sci. USA 2003, 100, 10529–10533. [Google Scholar] [CrossRef] [Green Version]
- Bingham, B.; Jones, P.G.; Uveges, A.J.; Kotnis, S.; Lu, P.; Smith, V.A.; Sun, S.-C.; Resnick, L.; Chlenov, M.; He, Y.; et al. Species-specific in vitro pharmacological effects of the cannabinoid receptor 2 (CB2) selective ligand AM1241 and its resolved enantiomers. Br. J. Pharmacol. 2007, 151, 1061–1070. [Google Scholar] [CrossRef] [PubMed]
- Mancini, I.; Brusa, R.; Quadrato, G.; Foglia, C.; Scandroglio, P.; Silverman, L.; Tulshian, D.; Reggiani, A.; Beltramo, M. Constitutive activity of cannabinoid-2 (CB2) receptors plays an essential role in the protean agonism of (+)AM1241 and L768242. Br. J. Pharmacol. 2009, 158, 382–391. [Google Scholar] [CrossRef]
- Quartilho, A.; Mata, H.P.; Ibrahim, M.M.; Vanderah, T.W.; Porreca, F.; Makriyannis, A.; Malan, T.P. Inhibition of Inflammatory Hyperalgesia by Activation of Peripheral CB2Cannabinoid Receptors. Anesthesiology 2003, 99, 955–960. [Google Scholar] [CrossRef]
- Hynes, J.; Leftheris, K.; Wu, H.; Pandit, C.; Chen, P.; Norris, D.J.; Chen, B.-C.; Zhao, R.; Kiener, P.A.; Chen, X.; et al. C-3 Amido-Indole cannabinoid receptor modulators. Bioorg. Med. Chem. Lett. 2002, 12, 2399–2402. [Google Scholar] [CrossRef]
- Dart, M.; Frost, J.; Tietje, K.; Daza, A.; Grayson, G.; Fan, Y.; Mukherjee, S.; Garrison, T.R.; Yao, B.; Meyer, M. 1-Alkyl-3-ketoindoles: Identification and in vitro characterization of a series of potent cannabinoid ligands. In Symposium on the Cannabinoids; International Cannabinoid Research Society: Burlington, VT, USA, 2006. [Google Scholar]
- Pertwee, R.; Griffin, G.; Fernando, S.; Li, X.; Hill, A.; Makriyannis, A. AM630, a competitive cannabinoid receptor antagonist. Life Sci. 1995, 56, 1949–1955. [Google Scholar] [CrossRef]
- Pertwee, R.G.; Fernando, S.R.; Nash, J.E.; Coutts, A.A. Further evidence for the presence of cannabinoid CB1 receptors in guinea-pig small intestine. Br. J. Pharmacol. 1996, 118, 2199–2205. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hosohata, Y.; Quock, R.M.; Hosohata, K.; Makriyannis, A.; Consroe, P.; Roeske, W.R.; Yamamura, H.I. AM630 antagonism of cannabinoid-stimulated [35S] GTP gamma S binding in the mouse brain. Eur. J. Pharmacol. 1997, 321, R1–R3. [Google Scholar] [CrossRef]
- Hosohata, K.; Quock, R.M.; Hosohata, Y.; Burkey, T.H.; Makriyannis, A.; Consroe, P.; Roeske, W.R.; Yamamura, H.I. AM630 is a competitive cannabinoid receptor antagonist in the guinea pig brain. Life Sci. 1997, 61, PL115–PL118. [Google Scholar] [CrossRef]
- Landsman, R.S.; Makriyannis, A.; Deng, H.; Consroe, P.; Roeske, W.R.; Yamamura, H.I. AM630 is an inverse agonist at the human cannabinoid CB1 receptor. Life Sci. 1998, 62, PL109–PL113. [Google Scholar] [CrossRef]
- Ross, R.A.; Brockie, H.C.; Stevenson, L.A.; Murphy, V.L.; Templeton, F.; Makriyannis, A.; Pertwee, R.G. Agonist-inverse agonist characterization at CB1 and CB2 cannabinoid receptors of L759633, L759656 and AM630. Br. J. Pharmacol. 1999, 126, 665–672. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dhopeshwarkar, A.; Mackie, K. Functional Selectivity of CB2 Cannabinoid Receptor Ligands at a Canonical and Noncanonical Pathway. J. Pharmacol. Exp. Ther. 2016, 358, 342–351. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chin, C.N.; Murphy, J.W.; Huffman, J.W.; Kendall, D.A. The third transmembrane helix of the cannabinoid receptor plays a role in the selectivity of aminoalkylindoles for CB2, peripheral cannabinoid receptor. J. Pharmacol. Exp. Ther. 1999, 291, 837–844. [Google Scholar] [PubMed]
- Tao, Q.; McAllister, S.D.; Andreassi, J.; Nowell, K.W.; Cabral, G.A.; Hurst, D.P.; Bachtel, K.; Ekman, M.C.; Reggio, P.H.; Abood, M. Role of a conserved lysine residue in the peripheral cannabinoid receptor (CB2): Evidence for subtype specificity. Mol. Pharmacol. 1999, 55, 605–613. [Google Scholar] [PubMed]
- Rhee, M.-H.; Nevo, I.; Levy, R.; Vogel, Z. Role of the highly conserved Asp-Arg-Tyr motif in signal transduction of the CB2 cannabinoid receptor. FEBS Lett. 2000, 466, 300–304. [Google Scholar] [CrossRef] [Green Version]
- Feng, W.; Song, Z. Effects of D3.49A, R3.50A, and A6.34E mutations on ligand binding and activation of the cannabinoid-2 (CB2) receptor. Biochem. Pharmacol. 2003, 65, 1077–1085. [Google Scholar] [CrossRef]
- Rhee, M.H.; Nevo, I.; Bayewitch, M.L.; Zagoory, O.; Vogel, Z. Functional role of tryptophan residues in the fourth transmembrane domain of the CB(2) cannabinoid receptor. J. Neurochem. 2000, 75, 2485–2491. [Google Scholar] [CrossRef] [Green Version]
- Atwood, B.K.; Wager-Miller, J.; Haskins, C.; Straiker, A.; Mackie, K. Functional Selectivity in CB2 Cannabinoid Receptor Signaling and Regulation: Implications for the Therapeutic Potential of CB2 Ligands. Mol. Pharmacol. 2012, 81, 250–263. [Google Scholar] [CrossRef] [Green Version]
- Stark, S.; Pacheco, M.A.; Childers, S.R. Binding of aminoalkylindoles to noncannabinoid binding sites in NG108-15 cells. Cell. Mol. Neurobiol. 1997, 17, 483–493. [Google Scholar] [CrossRef]
- Ho, B.Y.; Zhao, J. Determination of the cannabinoid receptors in mouse x rat hybridoma NG108-15 cells and rat GH4C1 cells. Neurosci. Lett. 1996, 212, 123–126. [Google Scholar] [CrossRef]
- Devane, W.A.; Spain, J.W.; Coscia, C.J.; Howlett, A.C. An Assessment of the Role of Opioid Receptors in the Response to Cannabimimetic Drugs. J. Neurochem. 1986, 46, 1929–1935. [Google Scholar] [CrossRef]
- Breivogel, C.S.; Griffin, G.; Di Marzo, V.; Martin, B.R. Evidence for a New G Protein-Coupled Cannabinoid Receptor in Mouse Brain. Mol. Pharmacol. 2001, 60, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Monory, K.; Tzavara, E.T.; Lexime, J.; Ledent, C.; Parmentier, M.; Borsodi, A.; Hanoune, J. Novel, Not Adenylyl Cyclase-Coupled Cannabinoid Binding Site in Cerebellum of Mice. Biochem. Biophys. Res. Commun. 2002, 292, 231–235. [Google Scholar] [CrossRef] [PubMed]
- Hájos, N.; Ledent, C.; Freund, T. Novel cannabinoid-sensitive receptor mediates inhibition of glutamatergic synaptic transmission in the hippocampus. Neuroscience 2001, 106, 1–4. [Google Scholar] [CrossRef]
- Németh, B.; Ledent, C.; Freund, T.F.; Hájos, N. CB1 receptor-dependent and -independent inhibition of excitatory postsynaptic currents in the hippocampus by WIN 55212-2. Neuropharmacology 2008, 54, 51–57. [Google Scholar] [CrossRef]
- Accorsi-Mendonça, D.; Almado, C.E.; Dagostin, A.L.; Machado, B.H.; Leão, R.M. Inhibition of spontaneous neurotransmission in the nucleus of solitary tract of the rat by the cannabinoid agonist WIN 55212-2 is not via CB1 or CB2 receptors. Brain Res. 2008, 1200, 1–9. [Google Scholar] [CrossRef]
- Stella, N. Cannabinoid and cannabinoid-like receptors in microglia, astrocytes, and astrocytomas. Glia 2010, 58, 1017–1030. [Google Scholar] [CrossRef] [Green Version]
- Fung, S.; Cherry, A.E.; Xu, C.; Stella, N. Alkylindole-sensitive receptors modulate microglial cell migration and proliferation. Glia 2015, 63, 1797–1808. [Google Scholar] [CrossRef] [Green Version]
- Fung, S.; Xu, C.; Hamel, E.; Wager-Miller, J.B.; Woodruff, G.; Miller, A.; Sanford, C.; Mackie, K.; Stella, N. Novel indole-based compounds that differentiate alkylindole-sensitive receptors from cannabinoid receptors and microtubules: Characterization of their activity on glioma cell migration. Pharmacol. Res. 2017, 115, 233–241. [Google Scholar] [CrossRef] [PubMed]
- Cherry, A.E.; Haas, B.R.; Naydenov, A.V.; Fung, S.; Xu, C.; Swinney, K.; Wagenbach, M.; Freeling, J.; Canton, D.A.; Coy, J.; et al. ST-11: A New Brain-Penetrant Microtubule-Destabilizing Agent with Therapeutic Potential for Glioblastoma Multiforme. Mol. Cancer Ther. 2016, 15, 2018–2029. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morales, P.; Reggio, P.H. An Update on Non-CB(1), Non-CB(2) Cannabinoid Related G-Protein-Coupled Receptors. Cannabis Cannabinoid Res. 2017, 2, 265–273. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adams, R.; Aycock, B.F.; Loewe, S. Tetrahydrocannabinol homologs. XVII. J. Am. Chem. Soc. 1948, 70, 662–664. [Google Scholar] [CrossRef]
- Adams, R.; Loewe, S.; Smith, C.M.; McPhee, W.D. Tetrahydrocannabinol homologs with marihuana activity. XIII. J. Am. Chem. Soc. 1942, 64, 694–698. [Google Scholar] [CrossRef]
- Adams, R.; MacKenzie, S.; Loewe, S. Tetrahydrocannabinol Homologs with Doubly Branched Alkyl Groups in the 3-Position. XVIII1. J. Am. Chem. Soc. 1948, 70, 664–668. [Google Scholar] [CrossRef] [PubMed]
- Appendino, G. The early history of cannabinoid research. Rend. Fis. Acc. Lincei 2020, 31, 919–929. [Google Scholar] [CrossRef]
- Williams, E.G.; Himmelsbach, C.K.; Wikler, A.; Ruble, D.C.; Lloyd, B.J. Studies on Marihuana and Pyrahexyl Compound. Public Health Rep. 1946, 61, 1059. [Google Scholar] [CrossRef] [PubMed]
- Ketchum, J.S. Chemical Warfare Secrets Almost Forgotten: A Personal Story of Medical Testing of Army Volunteers with Incapacitating Chemical Agents during the Cold War (1955–1975); Chembooks: Santa Rosa, CA, USA, 2006. [Google Scholar]
- Carroll, F.I.; Lewin, A.H.; Mascarella, S.W.; Seltzman, H.H.; Reddy, P.A. Designer drugs: A medicinal chemistry perspective (II). Ann. N. Y. Acad. Sci. 2021, 1489, 48–77. [Google Scholar] [CrossRef] [PubMed]
- Dolliver, D.S.; Kuhns, J.B. The Presence of New Psychoactive Substances in a Tor Network Marketplace Environment. J. Psychoact. Drugs 2016, 48, 321–329. [Google Scholar] [CrossRef] [PubMed]
- European Monitoring Centre for Drugs and Drug Addiction. European Drug Report 2021: Trends and Developments 2021; Publications Office of the European Union: Luxembourg, 2021. [Google Scholar]
- Cox, A.O.; Daw, R.C.; Mason, M.D.; Grabenauer, M.; Pande, P.G.; Davis, K.H.; Wiley, J.L.; Stout, P.R.; Thomas, B.F.; Huffman, J.W. Use of SPME-HS-GC-MS for the Analysis of Herbal Products Containing Synthetic Cannabinoids. J. Anal. Toxicol. 2012, 36, 293–302. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ginsburg, B.C.; McMahon, L.R.; Sanchez, J.J.; Javors, M.A. Purity of Synthetic Cannabinoids Sold Online for Recreational Use. J. Anal. Toxicol. 2012, 36, 66–68. [Google Scholar] [CrossRef] [Green Version]
- Münster-Müller, S.; Matzenbach, I.; Knepper, T.; Zimmermann, R.; Pütz, M. Profiling of synthesis-related impurities of the synthetic cannabinoid Cumyl-5F-PINACA in seized samples of e-liquids via multivariate analysis of UHPLC-MS(n) data. Drug Test Anal. 2020, 12, 119–126. [Google Scholar] [CrossRef]
- Moore, K.N.; Garvin, D.; Thomas, B.F.; Grabenauer, M. Identification of Eight Synthetic Cannabinoids, Including 5F-AKB48 in Seized Herbal Products Using DART-TOF-MS and LC-QTOF-MS as Nontargeted Screening Methods. J. Forensic Sci. 2017, 62, 1151–1158. [Google Scholar] [CrossRef]
- Kavanagh, P.; Grigoryev, A.; Savchuk, S.; Mikhura, I.; Formanovsky, A. UR-144 in products sold via the Internet: Identification of related compounds and characterization of pyrolysis products. Drug Test Anal. 2013, 5, 683–692. [Google Scholar] [CrossRef]
- Grabenauer, M.; Krol, W.L.; Wiley, J.L.; Thomas, B.F. Analysis of Synthetic Cannabinoids Using High-Resolution Mass Spectrometry and Mass Defect Filtering: Implications for Nontargeted Screening of Designer Drugs. Anal. Chem. 2012, 84, 5574–5581. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thomas, B.F.; Pollard, G.T.; Grabenauer, M. Analytical surveillance of emerging drugs of abuse and drug formulations. Life Sci. 2013, 92, 512–519. [Google Scholar] [CrossRef] [Green Version]
- Wiley, J.L.; Lefever, T.W.; Marusich, J.A.; Grabenauer, M.; Moore, K.N.; Huffman, J.W.; Thomas, B.F. Evaluation of first generation synthetic cannabinoids on binding at non-cannabinoid receptors and in a battery of in vivo assays in mice. Neuropharmacology 2016, 110, 143–153. [Google Scholar] [CrossRef] [Green Version]
- Wiley, J.L.; Marusich, J.A.; Lefever, T.W.; Grabenauer, M.; Moore, K.N.; Thomas, B. Cannabinoids in disguise: Δ9-Tetrahydrocannabinol-like effects of tetramethylcyclopropyl ketone indoles. Neuropharmacology 2013, 75, 145–154. [Google Scholar] [CrossRef] [Green Version]
- Wiley, J.L.; Marusich, J.A.; Thomas, B.F. Combination Chemistry: Structure–Activity Relationships of Novel Psychoactive Cannabinoids. Curr. Top. Behav. Neurosci. 2017, 32, 231–248. [Google Scholar] [CrossRef]
- Wiley, J.L.; Marusich, J.A.; Huffman, J.W. Moving around the molecule: Relationship between chemical structure and in vivo activity of synthetic cannabinoids. Life Sci. 2014, 97, 55–63. [Google Scholar] [CrossRef] [Green Version]
- Ford, B.M.; Tai, S.; Fantegrossi, W.E.; Prather, P.L. Synthetic Pot: Not Your Grandfather’s Marijuana. Trends Pharmacol. Sci. 2017, 38, 257–276. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Banister, S.D.; Connor, M. The Chemistry and Pharmacology of Synthetic Cannabinoid Receptor Agonists as New Psychoactive Substances: Origins. Handb. Exp. Pharmacol. 2018, 252, 165–190. [Google Scholar] [CrossRef] [PubMed]
- Banister, S.D.; Connor, M. The Chemistry and Pharmacology of Synthetic Cannabinoid Receptor Agonist New Psychoactive Substances: Evolution. Handb. Exp. Pharmacol. 2018, 252, 191–226. [Google Scholar] [CrossRef] [PubMed]
- Thomas, B.F.; Daw, R.C.; Pande, P.G.; Cox, A.O.; Kovach, A.L.; Davis, K.H., Jr.; Grabenauer, M. Analysis of Smoke Condensate From Combustion of Synthetic Cannabinoids in Herbal Products. In Proceedings of the 23rd Annual International Cannabinoid Research Society Symposium on the Cannabinoids, Vancouver, BC, Canada, 21–26 June 2013; pp. 4–24. [Google Scholar]
- Daw, R.; Grabenauer, M.; Pande, P.G.; Cox, A.; Kovach, A.; Davis, K.; Wiley, J.; Stout, P.; Thomas, B. Pyrolysis studies of synthetic cannabinoids in herbal products. Drug Alcohol Depend. 2014, 140, e44. [Google Scholar] [CrossRef]
- Tsujikawa, K.; Yamamuro, T.; Kuwayama, K.; Kanamori, T.; Iwata, Y.T.; Inoue, H. Thermal degradation of a new synthetic cannabinoid QUPIC during analysis by gas chromatography–mass spectrometry. Forensic Toxicol. 2014, 32, 201–207. [Google Scholar] [CrossRef]
- Thomas, B.F.; Lefever, T.W.; Cortes, R.A.; Grabenauer, M.; Kovach, A.; Cox, A.O.; Patel, P.R.; Pollard, G.T.; Marusich, J.A.; Kevin, R.C.; et al. Thermolytic Degradation of Synthetic Cannabinoids: Chemical Exposures and Pharmacological Consequences. J. Pharmacol. Exp. Ther. 2017, 361, 162–171. [Google Scholar] [CrossRef] [Green Version]
- Thomas, B.F.; Wiley, J.L.; Endres, G.W. Synthetic cannabinoids are recurring chemical threats. Cayman Curr. 2015, 26, 1–3. [Google Scholar]
- Gamage, T.F.; Farquhar, C.E.; Lefever, T.W.; Marusich, J.A.; Kevin, R.C.; Mcgregor, I.; Wiley, J.; Thomas, B.F. Molecular and Behavioral Pharmacological Characterization of Abused Synthetic Cannabinoids MMB- and MDMB-FUBINACA, MN-18, NNEI, CUMYL-PICA, and 5-Fluoro-CUMYL-PICA. J. Pharmacol. Exp. Ther. 2018, 365, 437–446. [Google Scholar] [CrossRef]
- Patton, A.L.; Seely, K.A.; Yarbrough, A.L.; Fantegrossi, W.; James, L.P.; McCain, K.R.; Fujiwara, R.; Prather, P.L.; Moran, J.H.; Radominska-Pandya, A. Altered metabolism of synthetic cannabinoid JWH-018 by human cytochrome P450 2C9 and variants. Biochem. Biophys. Res. Commun. 2018, 498, 597–602. [Google Scholar] [CrossRef]
- Kevin, R.C.; Kovach, A.; Lefever, T.W.; Gamage, T.F.; Wiley, J.L.; McGregor, I.S.; Thomas, B.F. Toxic by design? Formation of thermal degradants and cyanide from carboxamide-type synthetic cannabinoids CUMYL-PICA, 5F-CUMYL-PICA, AMB-FUBINACA, MDMB-FUBINACA, NNEI, and MN-18 during exposure to high temperatures. Forensic Toxicol. 2019, 37, 17–26. [Google Scholar] [CrossRef] [PubMed]
- Grigoryev, A.; Kavanagh, P.; Melnik, A.; Savchuk, S.; Simonov, A. Gas and Liquid Chromatography-Mass Spectrometry Detection of the Urinary Metabolites of UR-144 and Its Major Pyrolysis Product. J. Anal. Toxicol. 2013, 37, 265–276. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cooper, Z.D. Adverse Effects of Synthetic Cannabinoids: Management of Acute Toxicity and Withdrawal. Curr. Psychiatry Rep. 2016, 18, 52. [Google Scholar] [CrossRef] [Green Version]
- Pacher, P.; Steffens, S.; Haskó, G.; Schindler, T.H.; Kunos, G. Cardiovascular effects of marijuana and synthetic cannabinoids: The good, the bad, and the ugly. Nat. Rev. Cardiol. 2018, 15, 151–166. [Google Scholar] [CrossRef] [PubMed]
- Grigg, J.; Manning, V.; Arunogiri, S.; Lubman, D.I. Synthetic cannabinoid use disorder: An update for general psychiatrists. Australas. Psychiatry 2019, 27, 279–283. [Google Scholar] [CrossRef]
- Morrow, P.L.; Stables, S.; Kesha, K.; Tse, R.; Kappatos, D.; Pandey, R.; Russell, S.; Linsell, O.; McCarthy, M.J.; Spark, A.; et al. An outbreak of deaths associated with AMB-FUBINACA in Auckland NZ. EClinicalMedicine 2020, 25, 100460. [Google Scholar] [CrossRef]
- Tiemensma, M.; Rutherford, J.D.; Scott, T.; Karch, S. Emergence of Cumyl-PEGACLONE-related fatalities in the Northern Territory of Australia. Forensic Sci. Med. Pathol. 2021, 17, 3–9. [Google Scholar] [CrossRef]
- Ralphs, R.; Williams, L.; Askew, R.; Norton, A. Adding Spice to the Porridge: The development of a synthetic cannabinoid market in an English prison. CrimRxiv 2016. [Google Scholar] [CrossRef]
- Wohlfarth, A.; Scheidweiler, K.B.; Castaneto, M.; Gandhi, A.S.; Desrosiers, N.A.; Klette, K.L.; Martin, T.M.; Huestis, M.A. Urinary prevalence, metabolite detection rates, temporal patterns and evaluation of suitable LC-MS/MS targets to document synthetic cannabinoid intake in US military urine specimens. Clin. Chem. Lab. Med. 2015, 53, 423–434. [Google Scholar] [CrossRef]
- Finlay, D.B.; Manning, J.J.; Ibsen, M.S.; Macdonald, C.E.; Patel, M.; Javitch, J.A.; Banister, S.D.; Glass, M. Do Toxic Synthetic Cannabinoid Receptor Agonists Have Signature in Vitro Activity Profiles? A Case Study of AMB-FUBINACA. ACS Chem. Neurosci. 2019, 10, 4350–4360. [Google Scholar] [CrossRef] [PubMed]
- Sachdev, S.; Banister, S.; Santiago, M.J.; Bladen, C.; Kassiou, M.; Connor, M. Differential activation of G protein-mediated signaling by synthetic cannabinoid receptor agonists. Pharmacol. Res. Perspect. 2020, 8, e00566. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kumar, K.K.; Shalev-Benami, M.; Robertson, M.J.; Hu, H.; Banister, S.; Hollingsworth, S.A.; Latorraca, N.R.; Kato, H.; Hilger, D.; Maeda, S.; et al. Structure of a Signaling Cannabinoid Receptor 1-G Protein Complex. Cell 2019, 176, 448–458.e12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xing, C.; Zhuang, Y.; Xu, T.-H.; Feng, Z.; Zhou, X.E.; Chen, M.; Wang, L.; Meng, X.; Xue, Y.; Wang, J.; et al. Cryo-EM Structure of the Human Cannabinoid Receptor CB2-Gi Signaling Complex. Cell 2020, 180, 645–654.e13. [Google Scholar] [CrossRef]










| Name | N1 | C2 | C3 | CB2 Ki (nM) | CB2/CB1 Selectivity Ratio | Reference |
|---|---|---|---|---|---|---|
| JWH-015 | Propyl | Methyl | 1-naphthoyl | 13.8 | 27 | [57] |
| JWH-046 | Propyl | Methyl | 7-methyl-1-naphthoyl | 16.0 | 21 | [58] |
| JWH-120 | Propyl | H | 4-methyl-1-naphthoyl | 6.1 | 170 | [57] |
| JWH-267 | Pentyl | H | 2-methoxy-1-naphthoyl | 7.2 | 54 | [59] |
| JWH-151 | Propyl | Methyl | 6-methoxy-1-naphthoyl | 30.0 | >300 | [59] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Howlett, A.C.; Thomas, B.F.; Huffman, J.W. The Spicy Story of Cannabimimetic Indoles. Molecules 2021, 26, 6190. https://doi.org/10.3390/molecules26206190
Howlett AC, Thomas BF, Huffman JW. The Spicy Story of Cannabimimetic Indoles. Molecules. 2021; 26(20):6190. https://doi.org/10.3390/molecules26206190
Chicago/Turabian StyleHowlett, Allyn C., Brian F. Thomas, and John W. Huffman. 2021. "The Spicy Story of Cannabimimetic Indoles" Molecules 26, no. 20: 6190. https://doi.org/10.3390/molecules26206190