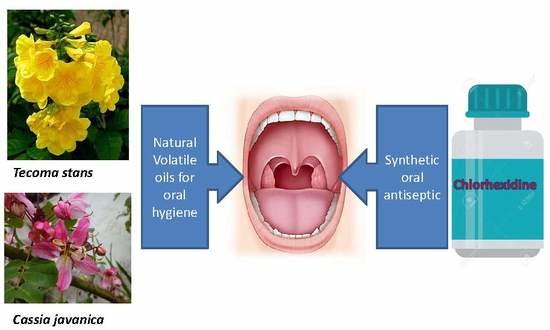
Anti-Oral Pathogens of Tecoma stans (L.) and Cassia javanica (L.) Flower Volatile Oils in Comparison with Chlorhexidine in Accordance with Their Folk Medicinal Uses
Abstract
:1. Introduction
2. Materials and Methods
2.1. Plant Collection and Method of Extraction
2.2. Gas Chromatography-Mass Spectroscopy (GC-MS) Analysis
2.3. Identifications of the Cassia javanica and Tecoma stans Constituents
2.4. Microorganisms
2.5. Determination of the Minimal Inhibitory Concentration (MIC) Using XTT Assay
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kleinberg, I. A mixed-bacteria ecological approach to understanding the role of the oral bacteria in dental caries causation: An alternative to Streptococcus mutans and the specific-plaque hypothesis. Crit. Rev. Oral Biol. Med. 2002, 13, 108–125. [Google Scholar] [CrossRef] [PubMed]
- Koo, H.; Gomes, B.; Rosalen, P.L.; Ambrosano, G.M.B.; Park, Y.K.; Cury, J.A. In vitro antimicrobial activity of propolis and Arnica montana against oral pathogens. Arch. Oral Biol. 2000, 45, 141–148. [Google Scholar] [CrossRef]
- Meyer, D.H.; Fives-Taylor, P.M. Oral pathogens: From dental plaque to cardiac disease. Curr. Opin. Microbiol. 1998, 1, 88–95. [Google Scholar] [CrossRef]
- Abe, S.; Ishihara, K.; Adachi, M.; Sasaki, H.; Tanaka, K.; Okuda, K. Professional oral care reduces influenza infection in elderly. Arch. Gerontol. Geriatr. 2006, 43, 157–164. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ichinose-Tsuno, A.; Aoki, A.; Takeuchi, Y.; Kirikae, T.; Shimbo, T.; Yoshino, F.; Maruoka, Y.; Itoh, T.; Ishikawa, I.; Izumi, Y. Antimicrobial photodynamic therapy suppresses dental plaque formation in healthy adults: A randomized controlled clinical trial. BMC Oral Health 2014, 14, 152. [Google Scholar] [CrossRef] [PubMed]
- Sbordone, L.; Bortolaia, C. Oral microbial biofilms and plaque-related diseases: Microbial communities and their role in the shift from oral health to disease. Clin. Oral Investig. 2003, 7, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Miller, W.D. Microorganisms of the Human Mouth; The SS White Dental Mfg: Philadelphia, PA, USA, 1890. [Google Scholar]
- Imfeld, T.N. Identification of low caries risk dietary components. Monogr. Oral Sci. 1983, 11, 1–198. [Google Scholar]
- Akhtar, J.; Siddique, K.M.; Bi, S.; Mujeeb, M. A review on phytochemical and pharmacological investigations of miswak (Salvadora persica Linn.). J. Pharm. Bioallied Sci. 2011, 3, 113. [Google Scholar]
- Alali, F.; Al-Lafi, T. GC-MS analysis and bioactivity testing of the volatile oil from the leaves of the toothbrush tree Salvadora persica L. Nat. Prod. Res. 2003, 17, 189–194. [Google Scholar] [CrossRef]
- Halawany, H.S. A review on miswak (Salvadora persica) and its effect on various aspects of oral health. Saudi Dent. J. 2012, 24, 63–69. [Google Scholar] [CrossRef]
- Hayacibara, M.F.; Koo, H.; Rosalen, P.L.; Duarte, S.; Franco, E.M.; Bowen, W.H.; Ikegaki, M.; Cury, J.A. In vitro and in vivo effects of isolated fractions of Brazilian propolis on caries development. J. Ethnopharmacol. 2005, 101, 110–115. [Google Scholar] [CrossRef] [PubMed]
- Chung, J.Y.; Choo, J.H.; Lee, M.H.; Hwang, J.K. Anticariogenic activity of macelignan isolated from Myristica fragrans (nutmeg) against Streptococcus mutans. Phytomedicine 2006, 13, 261–266. [Google Scholar] [CrossRef] [PubMed]
- Tichy, J.; Novak, J. Extraction, assay, and analysis of antimicrobials from plants with activity against dental pathogens (Streptococcus sp.). J. Altern. Complement. Med. 1998, 4, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Smullen, J.; Koutsou, G.A.; Foster, H.A.; Zumbé, A.; Storey, D.M. The antibacterial activity of plant extracts containing polyphenols against Streptococcus mutans. Caries Res. 2007, 41, 342–349. [Google Scholar] [CrossRef] [PubMed]
- Badria, F.A.; Zidan, O.A. Natural products for dental caries prevention. J. Med. Food 2004, 7, 381–384. [Google Scholar] [CrossRef] [PubMed]
- Flötra, L.; Gjermo, P.E.R.; Rölla, G.; Waerhaug, J. Side effects of chlorhexidine mouth washes. Eur. J. Oral Sci. 1971, 79, 119–125. [Google Scholar] [CrossRef]
- Pemberton, M.N.; Gibson, J. Chlorhexidine and hypersensitivity reactions in dentistry. Br. Dent. J. 2012, 213, 547. [Google Scholar] [CrossRef] [PubMed]
- Murugesan, K.; Sahadevan, R. Optimization of nonedible oil extraction from Cassia javanica seeds. Energy Sources Part A Recover. Util. Environ. Eff. 2017, 39, 1140–1146. [Google Scholar] [CrossRef]
- Sharma, A.; Ahmad, S.; Harikumar, S.L. Pharmacognosy, phytochemistry & pharmacology of Cassia javanica Linn.: A Review. Int. J. Pharma Res. Rev. 2014, 3, 101–105. [Google Scholar]
- Tiwari, R.D.; Singh, J. Anthraquinone rhamnosides from Cassia javanica root bark. Phytochemistry 1979, 18, 906. [Google Scholar] [CrossRef]
- Tiwari, R.D.; Yadava, O.P. The flavonoids of Cassia javanica flowers. Phytochemistry 1971, 10, 2256–2263. [Google Scholar] [CrossRef]
- Bhuvaneswari, R.; Gobalakrishnan, R. Antimicrobial potential and structural elucidation of bioactive compounds from flower extract of Cassia javanica L. Indian J. Nat. Prod. Resour. (IJNPR) 2015, 5, 34–39. [Google Scholar]
- Cheng, H.-Y.; Yang, C.-M.; Lin, T.-C.; Shieh, D.-E.; Lin, C.-C. ent-Epiafzelechin-(4α→8)-epiafzelechin extracted from Cassia javanica inhibits herpes simplex virus type 2 replication. J. Med. Microbiol. 2006, 55, 201–206. [Google Scholar] [CrossRef] [PubMed]
- Mehta, J.P.; Parmar, P.H.; Vadia, S.H.; Patel, M.K.; Tripathi, C.B. In-vitro antioxidant and in-vivo anti-inflammatory activities of aerial parts of Cassia species. Arab. J. Chem. 2017, 10, S1654–S1662. [Google Scholar] [CrossRef] [Green Version]
- Sundaramoorthy, S.; Gunasekaran, S.; Arunachalam, S.; Sathiavelu, M. A phytopharmacological review on cassia species. J. Pharm. Sci. Res. 2016, 8, 260. [Google Scholar]
- El-Gendy, M.M.A. In vitro, evaluation of medicinal activity of Egyptian honey from different floral sources as anticancer and antimycotic infective agents. J. Microb. Biochem. Technol. 2010, 2, 1000035. [Google Scholar] [CrossRef]
- Cunningham, P.L. Tecoma stans a potential invasive alien in Namibia. Dinteria 2008, 33–39. [Google Scholar]
- Ittagi, S.; Merugumolu, V.K.; Siddamsetty, R.S. Cardioprotective effect of hydroalcoholic extract of Tecoma stans flowers against isoproterenol induced myocardial infarction in rats. Asian Pac. J. Trop. Dis. 2014, 4, S378–S384. [Google Scholar] [CrossRef]
- Anburaj, G.; Marimuthu, M.; Rajasudha, V.; Manikandan, R. Phytochemical screening and GC-MS analysis of ethanolic extract of Tecoma stans (Family: Bignoniaceae) Yellow Bell Flowers. J. Pharm. Phytochem. 2016, 5, 172. [Google Scholar]
- Bianco, A.; Massa, M.; Oguakwa, J.U.; Passacantilli, P. 5-deoxystansioside, an iridoid glucoside from Tecoma stans. Phytochemistry 1981, 20, 1871–1872. [Google Scholar] [CrossRef]
- Aguilar-Santamaría, L.; Ramírez, G.; Nicasio, P.; Alegría-Reyes, C.; Herrera-Arellano, A. Antidiabetic activities of Tecoma stans (L.) Juss. ex Kunth. J. Ethnopharmacol. 2009, 124, 284–288. [Google Scholar]
- Kameshwaran, S.; Senthilkumar, R.; Thenmozhi, S.; Dhanalakshmi, M. Wound healing potential of ethanolic extract of tecoma stans flowers in rats. Pharmacologia 2014, 5, 215–221. [Google Scholar] [CrossRef]
- Rajamurugan, R.; Thirunavukkarasu, C.; Sakthivel, V.; Sivashanmugam, M.; Raghavan, C.M. Phytochemical screening, antioxidant and antimicrobial activities of ethanolic extract of Tecoma stans flowers. Int. J. Pharma Bio Sci. 2013, 4, P124–P130. [Google Scholar]
- Kameshwaran, S.; Suresh, V.; Arunachalam, G.; Frank, P.R.; Manikandan, V. Evaluation of antinociceptive and anti-inflammatory potential of flower extract Tecoma stans. Indian J. Pharm. 2012, 44, 543. [Google Scholar] [CrossRef] [PubMed]
- Raju, S.; Kavimani, S.; Reddy, K.S.; Kumar, G.V. Floral extract of Tecoma stans: A potent inhibitor of gentamicin-induced nephrotoxicity in vivo. Asian Pac. J. Trop. Med. 2011, 4, 680–685. [Google Scholar] [CrossRef]
- Tunney, M.M.; Ramage, G.; Field, T.R.; Moriarty, T.F.; Storey, D.G. Rapid colorimetric assay for antimicrobial susceptibility testing of Pseudomonas aeruginosa. Antimicrob. Agents Chemother. 2004, 48, 1879–1881. [Google Scholar] [CrossRef] [PubMed]
- Ganesan, S. Traditional Oral Care Medicinal Plants Survey of Tamil Nadu; CSIR: New Delhi, India, 2008; pp. 166–172. [Google Scholar]
- Bever, B.O. Oral hypoglycaemic plants in West Africa. J. Ethnopharmacol. 1980, 2, 119–127. [Google Scholar] [CrossRef]
- Sobeh, M.; Braun, M.S.; Krstin, S.; Youssef, F.S.; Ashour, M.L.; Wink, M. Chemical profiling of the essential oils of Syzygium aqueum, Syzygium samarangense and Eugenia uniflora and their discrimination using chemometric analysis. Chem. Biodivers. 2016, 13, 1537–1550. [Google Scholar] [CrossRef] [PubMed]
- Nadaf, M.; Nasrabadi, M.; Halimi, M. GC-MS analysis of n-hexane extract from aerial parts of Salvia nemorosa. Middle-East. J. Sci Res. 2012, 11, 1127–1130. [Google Scholar]
- Mostafa, N.M. β-Amyrin rich Bombax ceiba leaf extract with potential neuroprotective activity against scopolamine-induced memory impairment in rats. Rec. Nat. Prod. 2018, 12, 480. [Google Scholar] [CrossRef]
- Mohamed, S.H.; Mohamed, M.S.M.; Khalil, M.S.; Azmy, M.; Mabrouk, M.I. Combination of essential oil and ciprofloxacin to inhibit/eradicate biofilms in multidrug-resistant Klebsiella pneumoniae. J. Appl. Microbiol. 2018, 125, 84–95. [Google Scholar] [CrossRef] [PubMed]
- Hudaib, M.; Bellardi, M.G.; Rubies-Autonell, C.; Fiori, J.; Cavrini, V. Chromatographic (GC-MS, HPLC) and virological evaluations of Salvia sclarea infected by BBWV-I. Farmaco 2001, 56, 219–227. [Google Scholar] [CrossRef]
- Hudaib, M.M.; Aburjai, T.A. Composition of the essential oil from Artemisia herba-alba grown in Jordan. J. Essent. Oil Res. 2006, 18, 301–304. [Google Scholar] [CrossRef]
- Hanamanthagouda, M.S.; Kakkalameli, S.B.; Naik, P.M.; Nagella, P.; Seetharamareddy, H.R.; Murthy, H.N. Essential oils of Lavandula bipinnata and their antimicrobial activities. Food Chem. 2010, 118, 836–839. [Google Scholar] [CrossRef]
- Hamdan, D.I.; Mohamed, M.E.; Abdulla, R.H.; Mohamed, S.M.; El-Shazly, A.M. Anti-inflammatory, insecticidal and antimicrobial activities and chemical composition of the essential oils of different plant organs from navel orange (Citrus sinensis (L.) Osbeck var. Malesy) grown in Egypt. J. Med. Plants Res. 2013, 7, 1204–1215. [Google Scholar]
- Hamdan, D.I.; Abdulla, R.H.; Mohamed, M.E.; El-Shazly, A.M. Chemical composition and biological activity of essential oils of Cleopatra mandarin (Citrus reshni) cultivated in Egypt. J. Pharm. Phyther. 2013, 5, 83–90. [Google Scholar]
- Do, N.; Fontes, J.E.; Ferraz, R.P.C.; Britto, A.C.S.; Carvalho, A.A.; Moraes, M.O.; Pessoa, C.; Costa, E.V.; Bezerra, D.P. Antitumor effect of the essential oil from leaves of Guatteria pogonopus (Annonaceae). Chem. Biodivers. 2013, 10, 722–729. [Google Scholar]
- Rodrigues, M.E.; Henriques, M.; Silva, S. Disinfectants to fight oral candida biofilms. In Fungal Biofilms and Related Infections; Springer: Cham, Switzerland, 2016; pp. 83–93. [Google Scholar]
- Mohammed, H.A.; Al-Omar, M.S.; Aly, M.S.A.; Hegazy, M.M. Essential oil constituents and biological activities of the halophytic plants, Suaeda vermiculata Forssk and Salsola cyclophylla Bakera growing in Saudi Arabia. J. Essent. Oil Bear. Plants 2019, 1–12. [Google Scholar] [CrossRef]
- Reyes-Jurado, F.; Navarro-Cruz, A.R.; Ochoa-Velasco, C.E.; Palou, E.; López-Malo, A.; Ávila-Sosa, R. Essential oils in vapor phase as alternative antimicrobials: A review. Crit. Rev. Food Sci. Nutr. 2019, 15, 1–10. [Google Scholar] [CrossRef]
- Imfeld, T. Chlorhexidine-containing chewing gum. Schweizer Monatsschrift fur Zahnmedizin 2006, 116, 476. [Google Scholar]
- Saxena, S.; Meshram, V.; Kapoor, N. Muscodor tigerii sp. nov.-Volatile antibiotic producing endophytic fungus from the Northeastern Himalayas. Ann. Microbiol. 2015, 65, 47–57. [Google Scholar] [CrossRef]
- Park, S.-N.; Lim, Y.K.; Freire, M.O.; Cho, E.; Jin, D.; Kook, J.-K. Antimicrobial effect of linalool and α-terpineol against periodontopathic and cariogenic bacteria. Anaerobe 2012, 18, 369–372. [Google Scholar] [CrossRef] [PubMed]
- Loesche, W.J. Role of Streptococcus mutans in human dental decay. Microbiol. Rev. 1986, 50, 353. [Google Scholar] [PubMed]
- Bersan, S.M.; Galvão, L.C.; Goes, V.F.; Sartoratto, A.; Figueira, G.M.; Rehder, V.L.; Alencar, S.M.; Duarte, R.M.; Rosalen, P.L.; Duarte, M.C. Action of essential oils from Brazilian native and exotic medicinal species on oral biofilms. BMC Complement. Altern. Med. 2014, 14, 451. [Google Scholar] [CrossRef] [PubMed]

| No | Compound Name | RT | RIexp | RIrep | %RTecoma stans | %RCassia javanica |
|---|---|---|---|---|---|---|
| 1 | Decane | 9.161 | 989 | 891 | 6.06 | 0.89 |
| 2 | 3-Carene | 9.870 | 1012 | 1012 | 1.21 | 0.36 |
| 3 | m-Cymene | 10.160 | 1021 | 1021 | 0.62 | - |
| 4 | (Z)-β-Ocimene | 10.890 | 1044 | 1043 | 0.93 | - |
| 5 | Heptyl acetate | 10.980 | 1047 | 1047 | 0.92 | - |
| 6 | (Z)-β-Ocimene | 11.075 | 1050 | 1050 | 0.99 | 0.35 |
| 7 | 2-Methyldecane | 11.190 | 1053 | 1051 | 2.57 | 1.10 |
| 8 | γ-Terpinene | 11.395 | 1060 | 1059 | 0.96 | 0.45 |
| 9 | 2,9-Dimethyldecane | 12.350 | 1090 | 1086 | 15.87 | 11.46 |
| 10 | Nonanal | 12.875 | 1106 | 1107 | 1.62 | - |
| 11 | Myrcenol | 13.180 | 1116 | 1116 | 1.98 | - |
| 12 | Fenchol | 13.205 | 1117 | 1117 | - | 0.98 |
| 13 | trans-Pinene hydrate | 13.420 | 1124 | 1123 | 1.33 | 0.80 |
| 14 | neo-Isopulegol | 14.025 | 1143 | 1143 | 1.37 | - |
| 15 | trans-Verbenol | 14.070 | 1144 | 1144 | 1.41 | 1.73 |
| 16 | Z-Tagetone | 14.190 | 1148 | 1147 | 1.64 | 1.33 |
| 17 | Citronellal | 14.325 | 1152 | 1153 | 5.09 | 3.79 |
| 18 | β-Pinene oxide | 14.525 | 1159 | 1158 | 2.26 | 1.28 |
| 19 | Artemisyl acetate | 15.035 | 1175 | 1174 | - | 0.90 |
| 20 | Terpinen-4-ol | 15.176 | 1179 | 1177 | - | 0.50 |
| 21 | p-Cymen-8-ol | 15.455 | 1188 | 1188 | 23.73 | - |
| 22 | α-Terpineol | 15.490 | 1189 | 1189 | - | 29.32 |
| 23 | cis-Dihydrocarvone | 15.845 | 1200 | 1198 | 3.60 | 3.11 |
| 24 | Pulegone | 16.600 | 1226 | 1227 | 0.75 | - |
| 25 | Citronellol | 16.634 | 1228 | 1228 | - | 0.59 |
| 26 | Cumin aldehyde | 16.985 | 1240 | 1239 | 0.69 | - |
| 27 | Neral | 17.045 | 1242 | 1242 | 0.67 | - |
| 28 | Carvone | 17.180 | 1247 | 1248 | 0.88 | 0.55 |
| 29 | Piperitone | 17.320 | 1252 | 1253 | 2.77 | 2.42 |
| 30 | Methyl citronellate | 17.510 | 1258 | 1258 | 1.59 | 1.39 |
| 31 | Linalyl acetate | 17.580 | 1261 | 1261 | 2.95 | 2.58 |
| 32 | Geranial | 17.795 | 1268 | 1268 | - | 0.27 |
| 33 | Limonen-10-ol | 18.375 | 1288 | 1289 | 0.55 | 0.60 |
| 34 | Palmitic acid | 34.465 | 1951 | 1953 | 1.32 | - |
| 35 | 4-Hexadecyl hexanoate | 42.185 | 2367 | 2362 | 0.57 | |
| 36 | Pentacosane | 44.860 | 2533 | 2521 | 1.78 | |
| 37 | 1,2-Benzenedicarboxylic acid, mono(2-ethylhexyl) ester | 44.895 | 2535 | 2521 | - | 6.71 |
| 38 | Heptacosane | 46.980 | 2669 | 2666 | 6.44 | 6.80 |
| 39 | Octacosane | 48.450 | 2764 | 2738 | - | 1.34 |
| 40 | Squalene | 49.850 | 2854 | 2831 | 4.76 | 10.51 |
| 41 | Stigmastan-3,5-diene | 52.560 | 3028 | 3040 | 0.67 | 7.33 |
| Total percentage | 100 | 100 | ||||
| Monoterpene hydrocarbons | 29.12 | 14.61 | ||||
| Monoterpene alcohols | 30.37 | 34.02 | ||||
| Esters | 5.46 | 12.15 | ||||
| Aldehydes | 8.07 | 4.06 | ||||
| Ketones | 9.64 | 7.41 | ||||
| Long chain hydrocarbons | 13.65 | 25.98 | ||||
| Pathogen | Cassia javanica | Tecoma stans | Chlorhexidine | ||||||
|---|---|---|---|---|---|---|---|---|---|
| MIC50 | MIC90 | MIC | MIC50 | MIC90 | MIC | MIC50 | MIC90 | MIC | |
| Porphyromonas gingivalis | 30.13 ± 1.48 | 79.03 ± 0.78 | 100 | 96.50 ± 2.2 | nd | nd | 5.51 ± 0.17 | 16.25 ± 0.57 | 25 |
| Streptococcus mutans | 3.89 ± 0.07 | 9.57 ± 0.21 | 12.5 | 4.77 ± 0.02 | 18.49 ± 0.39 | 25 | 0.31 ± 0.01 | 0.99 ± 0.11 | 1.56 |
| Lactobacillus acidophilus | 5.93 ± 0.22 | 21.2 ± 0.23 | 25 | 17.39 ± 0.33 | 47.6 ± 1.8 | 100 | 0.36 ± 0.01 | 1.5 ± 0.03 | 3.13 |
| Candida albicans | 9.43 ± 0.41 | 17.5 ± 0.23 | 25 | nd | nd | nd | 1.16 ± 0.03 | 4.47 ± 0.18 | 6.25 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mohammed, H.A.; Abdel-Aziz, M.M.; Hegazy, M.M. Anti-Oral Pathogens of Tecoma stans (L.) and Cassia javanica (L.) Flower Volatile Oils in Comparison with Chlorhexidine in Accordance with Their Folk Medicinal Uses. Medicina 2019, 55, 301. https://doi.org/10.3390/medicina55060301
Mohammed HA, Abdel-Aziz MM, Hegazy MM. Anti-Oral Pathogens of Tecoma stans (L.) and Cassia javanica (L.) Flower Volatile Oils in Comparison with Chlorhexidine in Accordance with Their Folk Medicinal Uses. Medicina. 2019; 55(6):301. https://doi.org/10.3390/medicina55060301
Chicago/Turabian StyleMohammed, Hamdoon A., Marwa M. Abdel-Aziz, and Mostafa M. Hegazy. 2019. "Anti-Oral Pathogens of Tecoma stans (L.) and Cassia javanica (L.) Flower Volatile Oils in Comparison with Chlorhexidine in Accordance with Their Folk Medicinal Uses" Medicina 55, no. 6: 301. https://doi.org/10.3390/medicina55060301