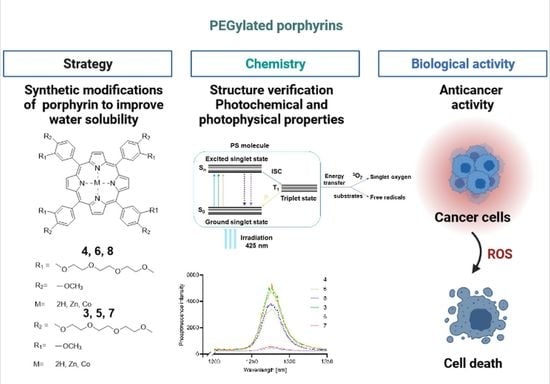
Novel Short PEG Chain-Substituted Porphyrins: Synthesis, Photochemistry, and In Vitro Photodynamic Activity against Cancer Cells
Abstract
:1. Introduction
2. Results and Discussion
2.1. Synthesis
2.2. NMR Spectroscopy
2.3. Mass Spectrometry with Fragmentation
2.4. UV-Vis Spectroscopy and Simulation
2.5. Singlet Oxygen Generation
2.6. Biological Activity
3. Materials and Methods
3.1. Molecular Modeling
3.2. PEGylated Aldehyde Synthesis—General Procedure
3.3. PEGylated Porphyrin Synthesis—General Procedure
3.4. Metallated PEGylated Porphyrins—General Procedure
3.5. Singlet Oxygen Measurement
3.6. Chromatographic Analysis of Purity
3.7. Cytotoxic Activity of the Tested Compounds
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gunaydin, G.; Gedik, M.E.; Ayan, S. Photodynamic Therapy for the Treatment and Diagnosis of Cancer—A Review of the Current Clinical Status. Front. Chem. 2021, 9, 608. [Google Scholar] [CrossRef] [PubMed]
- Morton, C.; Szeimies, R.-M.; Basset-Séguin, N.; Calzavara-Pinton, P.; Gilaberte, Y.; Hædersdal, M.; Hofbauer, G.; Hunger, R.; Karrer, S.; Piaserico, S.; et al. European Dermatology Forum Guidelines on Topical Photodynamic Therapy 2019 Part 2: Emerging Indications—Field Cancerization, Photorejuvenation and Inflammatory/Infective Dermatoses. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 17–29. [Google Scholar] [CrossRef]
- Overholt, B.F.; Lightdale, C.J.; Wang, K.K.; Canto, M.I.; Burdick, S.; Haggitt, R.C.; Bronner, M.P.; Taylor, S.L.; Grace, M.G.A.; Depot, M. Photodynamic Therapy with Porfimer Sodium for Ablation of High-Grade Dysplasia in Barrett’s Esophagus: International, Partially Blinded, Randomized Phase III Trial. Gastrointest. Endosc. 2005, 62, 488–498. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.; Yang, T.; Shi, P.; Shen, J.; Feng, Q.; Su, J. Benefits and Safety of Photodynamic Therapy in Patients with Hilar Cholangiocarcinoma: A Meta-Analysis. Photodiagn. Photodyn. Ther. 2022, 37, 102712. [Google Scholar] [CrossRef] [PubMed]
- Lambert, A.; Nees, L.; Nuyts, S.; Clement, P.; Meulemans, J.; Delaere, P.; Vander Poorten, V. Photodynamic Therapy as an Alternative Therapeutic Tool in Functionally Inoperable Oral and Oropharyngeal Carcinoma: A Single Tertiary Center Retrospective Cohort Analysis. Front. Oncol. 2021, 11, 626394. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, N.; Usuda, J.; Maehara, S. Photodynamic Therapy for Central-Type Early-Stage Lung Cancer. Gen. Thorac. Cardiovasc. Surg. 2020, 68, 679–683. [Google Scholar] [CrossRef]
- Usuda, J.; Kato, H.; Okunaka, T.; Furukawa, K.; Tsutsui, H.; Yamada, K.; Suga, Y.; Honda, H.; Nagatsuka, Y.; Ohira, T.; et al. Photodynamic Therapy (PDT) for Lung Cancers. J. Thorac. Oncol. 2006, 1, 489–493. [Google Scholar] [CrossRef]
- Kulkarni, G.S.; Lilge, L.; Nesbitt, M.; Dumoulin-White, R.J.; Mandel, A.; Jewett, M.A.S. A Phase 1b Clinical Study of Intravesical Photodynamic Therapy in Patients with Bacillus Calmette-Guérin–Unresponsive Non–Muscle-Invasive Bladder Cancer. Eur. Urol. Open Sci. 2022, 41, 105–111. [Google Scholar] [CrossRef]
- Del Regno, L.; Catapano, S.; Di Stefani, A.; Cappilli, S.; Peris, K. A Review of Existing Therapies for Actinic Keratosis: Current Status and Future Directions. Am. J. Clin. Dermatol. 2022, 23, 339–352. [Google Scholar] [CrossRef]
- Van Dijk, E.H.C.; van Rijssen, T.J.; Subhi, Y.; Boon, C.J.F. Photodynamic Therapy for Chorioretinal Diseases: A Practical Approach. Ophthalmol. Ther. 2020, 9, 329–342. [Google Scholar] [CrossRef] [Green Version]
- Correia, J.H.; Rodrigues, J.A.; Pimenta, S.; Dong, T.; Yang, Z. Photodynamic Therapy Review: Principles, Photosensitizers, Applications, and Future Directions. Pharmaceutics 2021, 13, 1332. [Google Scholar] [CrossRef] [PubMed]
- Mallidi, S.; Anbil, S.; Bulin, A.-L.; Obaid, G.; Ichikawa, M.; Hasan, T. Beyond the Barriers of Light Penetration: Strategies, Perspectives and Possibilities for Photodynamic Therapy. Theranostics 2016, 6, 2458–2487. [Google Scholar] [CrossRef]
- Kessel, D.; Obaid, G.; Rizvi, I. Critical PDT Theory II: Current Concepts and Indications. Photodiagn. Photodyn. Ther. 2022, 39, 102923. [Google Scholar] [CrossRef] [PubMed]
- Kessel, D. Critical PDT Theory III: Events at the Molecular and Cellular Level. Int. J. Mol. Sci. 2022, 23, 6195. [Google Scholar] [CrossRef]
- Wang, C.; Zhao, P.; Jiang, D.; Yang, G.; Xue, Y.; Tang, Z.; Zhang, M.; Wang, H.; Jiang, X.; Wu, Y.; et al. In Situ Catalytic Reaction for Solving the Aggregation of Hydrophobic Photosensitizers in Tumor. ACS Appl. Mater. Interfaces 2020, 12, 5624–5632. [Google Scholar] [CrossRef]
- Casas, A.; Di Venosa, G.; Hasan, T.; Batlle, A. Mechanisms of Resistance to Photodynamic Therapy. Curr. Med. Chem. 2011, 18, 2486–2515. [Google Scholar] [CrossRef]
- Spring, B.Q.; Rizvi, I.; Xu, N.; Hasan, T. The Role of Photodynamic Therapy in Overcoming Cancer Drug Resistance. Photochem. Photobiol. Sci. Off. J. Eur. Photochem. Assoc. Eur. Soc. Photobiol. 2015, 14, 1476–1491. [Google Scholar] [CrossRef] [PubMed]
- Escudero, A.; Carrillo-Carrión, C.; Castillejos, M.C.; Romero-Ben, E.; Rosales-Barrios, C.; Khiar, N. Photodynamic Therapy: Photosensitizers and Nanostructures. Mater. Chem. Front. 2021, 5, 3788–3812. [Google Scholar] [CrossRef]
- Matsson, P.; Doak, B.C.; Over, B.; Kihlberg, J. Cell Permeability beyond the Rule of 5. Adv. Drug Deliv. Rev. 2016, 101, 42–61. [Google Scholar] [CrossRef]
- Feng, G.; Wang, C.; Chen, C.; Pan, Y.; Wu, M.; Wang, Y.; Liu, J.; Liu, B. Modulating Cell Specificity and Subcellular Localization by Molecular Charges and Lipophilicity. Chem. Mater. 2020, 32, 10383–10393. [Google Scholar] [CrossRef]
- Luciano, M.; Brückner, C. Modifications of Porphyrins and Hydroporphyrins for Their Solubilization in Aqueous Media. Molecules 2017, 22, 980. [Google Scholar] [CrossRef] [PubMed]
- Xie, J.; Wang, Y.; Choi, W.; Jangili, P.; Ge, Y.; Xu, Y.; Kang, J.; Liu, L.; Zhang, B.; Xie, Z.; et al. Overcoming Barriers in Photodynamic Therapy Harnessing Nano-Formulation Strategies. Chem. Soc. Rev. 2021, 50, 9152–9201. [Google Scholar] [CrossRef]
- Ekladious, I.; Colson, Y.L.; Grinstaff, M.W. Polymer–Drug Conjugate Therapeutics: Advances, Insights and Prospects. Nat. Rev. Drug Discov. 2019, 18, 273–294. [Google Scholar] [CrossRef]
- Banerjee, S.S.; Aher, N.; Patil, R.; Khandare, J. Poly(Ethylene Glycol)-Prodrug Conjugates: Concept, Design, and Applications. J. Drug Deliv. 2012, 2012, 103973. [Google Scholar] [CrossRef]
- Kuang, G.; Zhang, Q.; He, S.; Liu, Y. Curcumin-Loaded PEGylated Mesoporous Silica Nanoparticles for Effective Photodynamic Therapy. RSC Adv. 2020, 10, 24624–24630. [Google Scholar] [CrossRef]
- Fadeel, D.A.; Kamel, R.; Fadel, M. PEGylated Lipid Nanocarrier for Enhancing Photodynamic Therapy of Skin Carcinoma Using Curcumin: In-Vitro/in-Vivo Studies and Histopathological Examination. Sci. Rep. 2020, 10, 10435. [Google Scholar] [CrossRef]
- Master, A.M.; Rodriguez, M.E.; Kenney, M.E.; Oleinick, N.L.; Gupta, A.S. Delivery of the Photosensitizer Pc 4 in PEG-PCL Micelles for in Vitro PDT Studies. J. Pharm. Sci. 2010, 99, 2386–2398. [Google Scholar] [CrossRef]
- Zmerli, I.; Ibrahim, N.; Cressey, P.; Denis, S.; Makky, A. Design and Synthesis of New PEGylated Polydopamine-Based Nanoconstructs Bearing ROS-Responsive Linkers and a Photosensitizer for Bimodal Photothermal and Photodynamic Therapies against Cancer. Mol. Pharm. 2021, 18, 3623–3637. [Google Scholar] [CrossRef]
- Sapra, P.; Zhao, H.; Mehlig, M.; Malaby, J.; Kraft, P.; Longley, C.; Greenberger, L.M.; Horak, I.D. Novel Delivery of SN38 Markedly Inhibits Tumor Growth in Xenografts, Including a Camptothecin-11–Refractory Model. Clin. Cancer Res. 2008, 14, 1888–1896. [Google Scholar] [CrossRef]
- Zhao, H.; Rubio, B.; Sapra, P.; Wu, D.; Reddy, P.; Sai, P.; Martinez, A.; Gao, Y.; Lozanguiez, Y.; Longley, C.; et al. Novel Prodrugs of SN38 Using Multiarm Poly(Ethylene Glycol) Linkers. Bioconjug. Chem. 2008, 19, 849–859. [Google Scholar] [CrossRef] [PubMed]
- Simpson, C.A.; Agrawal, A.C.; Balinski, A.; Harkness, K.M.; Cliffel, D.E. Short-Chain PEG Mixed Monolayer Protected Gold Clusters Increase Clearance and Red Blood Cell Counts. ACS Nano 2011, 5, 3577–3584. [Google Scholar] [CrossRef] [PubMed]
- Harris, J.M.; Chess, R.B. Effect of Pegylation on Pharmaceuticals. Nat. Rev. Drug Discov. 2003, 2, 214–221. [Google Scholar] [CrossRef] [PubMed]
- Rudmann, D.G.; Alston, J.T.; Hanson, J.C.; Heidel, S. High Molecular Weight Polyethylene Glycol Cellular Distribution and PEG-Associated Cytoplasmic Vacuolation Is Molecular Weight Dependent and Does Not Require Conjugation to Proteins. Toxicol. Pathol. 2013, 41, 970–983. [Google Scholar] [CrossRef] [PubMed]
- Yadav, D.; Dewangan, H.K. PEGYLATION: An Important Approach for Novel Drug Delivery System. J. Biomater. Sci. Polym. Ed. 2021, 32, 266–280. [Google Scholar] [CrossRef]
- Wierzchowski, M.; Łażewski, D.; Tardowski, T.; Grochocka, M.; Czajkowski, R.; Sobiak, S.; Sobotta, L. Nanomolar Photodynamic Activity of Porphyrins Bearing 1,4,7-Trioxanonyl and 2-Methyl-5-Nitroimidazole Moieties against Cancer Cells. J. Photochem. Photobiol. B 2020, 202, 111703. [Google Scholar] [CrossRef]
- Sobotta, L.; Wierzchowski, M.; Mierzwicki, M.; Gdaniec, Z.; Mielcarek, J.; Persoons, L.; Goslinski, T.; Balzarini, J. Photochemical Studies and Nanomolar Photodynamic Activities of Phthalocyanines Functionalized with 1,4,7-Trioxanonyl Moieties at Their Non-Peripheral Positions. J. Inorg. Biochem. 2016, 155, 76–81. [Google Scholar] [CrossRef] [PubMed]
- Hamblin, M.R. Photodynamic Therapy for Cancer: What’s Past Is Prologue. Photochem. Photobiol. 2020, 96, 506–516. [Google Scholar] [CrossRef]
- Pavlíčková, V.; Rimpelová, S.; Jurášek, M.; Záruba, K.; Fähnrich, J.; Křížová, I.; Bejček, J.; Rottnerová, Z.; Spiwok, V.; Drašar, P.; et al. PEGylated Purpurin 18 with Improved Solubility: Potent Compounds for Photodynamic Therapy of Cancer. Molecules 2019, 24, 4477. [Google Scholar] [CrossRef]
- Nawalany, K.; Rusin, A.; Kępczyński, M.; Mikhailov, A.; Kramer-Marek, G.; Śnietura, M.; Połtowicz, J.; Krawczyk, Z.; Nowakowska, M. Comparison of Photodynamic Efficacy of Tetraarylporphyrin Pegylated or Encapsulated in Liposomes: In Vitro Studies. J. Photochem. Photobiol. B 2009, 97, 8–17. [Google Scholar] [CrossRef]
- Ruan, Z.; Zhao, Y.; Yuan, P.; Liu, L.; Wang, Y.; Yan, L. PEG Conjugated BODIPY-Br2 as Macro-Photosensitizer for Efficient Imaging-Guided Photodynamic Therapy. J. Mater. Chem. B 2018, 6, 753–762. [Google Scholar] [CrossRef]
- Hou, W.; Xia, F.; Alves, C.S.; Qian, X.; Yang, Y.; Cui, D. MMP2-Targeting and Redox-Responsive PEGylated Chlorin E6 Nanoparticles for Cancer Near-Infrared Imaging and Photodynamic Therapy. ACS Appl. Mater. Interfaces 2016, 8, 1447–1457. [Google Scholar] [CrossRef] [PubMed]
- Mandal, S.; Mandal, S.; Ghosh, S.K.; Sar, P.; Ghosh, A.; Saha, R.; Saha, B. A Review on the Advancement of Ether Synthesis from Organic Solvent to Water. RSC Adv. 2016, 6, 69605–69614. [Google Scholar] [CrossRef]
- Adler, A.D.; Longo, F.R.; Finarelli, J.D.; Goldmacher, J.; Assour, J.; Korsakoff, L. A Simplified Synthesis for Meso-Tetraphenylporphine. J. Org. Chem. 1967, 32, 476. [Google Scholar] [CrossRef]
- Lindsey, J.S.; Schreiman, I.C.; Hsu, H.C.; Kearney, P.C.; Marguerettaz, A.M. Rothemund and Adler-Longo Reactions Revisited: Synthesis of Tetraphenylporphyrins under Equilibrium Conditions. J. Org. Chem. 1987, 52, 827–836. [Google Scholar] [CrossRef]
- Suckau, D.; Resemann, A.; Schuerenberg, M.; Hufnagel, P.; Franzen, J.; Holle, A. A Novel MALDI LIFT-TOF/TOF Mass Spectrometer for Proteomics. Anal. Bioanal. Chem. 2003, 376, 952–965. [Google Scholar] [CrossRef]
- Mauger, F.; Tabet, J.-C.; Gut, I.G. A Revisit of High Collision Energy Effects on Collision-Induced Dissociation Spectra Using Matrix-Assisted Laser Desorption/Ionization Tandem Time-of-Flight Mass Spectrometry (MALDI-LIFT-TOF/TOF): Application to the Sequencing of RNA/DNA Chimeras. Rapid Commun. Mass Spectrom. 2014, 28, 1433–1443. [Google Scholar] [CrossRef]
- Town, J.S.; Jones, G.R.; Hancox, E.; Shegiwal, A.; Haddleton, D.M. Tandem Mass Spectrometry for Polymeric Structure Analysis: A Comparison of Two Common MALDI–ToF/ToF Techniques. Macromol. Rapid Commun. 2019, 40, 1900088. [Google Scholar] [CrossRef]
- Gouterman, M.; Wagnière, G.H.; Snyder, L.C. Spectra of Porphyrins: Part II. Four Orbital Model. J. Mol. Spectrosc. 1963, 11, 108–127. [Google Scholar] [CrossRef]
- Ricci, M.; Lofrumento, C.; Becucci, M.; Castellucci, E.M. The Raman and SERS Spectra of Indigo and Indigo-Ag2 Complex: DFT Calculation and Comparison with Experiment. Spectrochim. Acta A Mol. Biomol. Spectrosc. 2018, 188, 141–148. [Google Scholar] [CrossRef]
- Wierzchowski, M.; Sobotta, L.; Łażewski, D.; Kasprzycki, P.; Fita, P.; Goslinski, T. Spectroscopic and Quantum Chemical Study of Phthalocyanines with 1,4,7-Trioxanonyl Moieties. J. Mol. Struct. 2020, 1203, 127371. [Google Scholar] [CrossRef]
- Anbarasanan, P.M.; Kumar, S.P.; Vasudevan, K.; Moorthy Babu, S.; Aroulmoji, V. DFT and TD-DFT Calculations of Some Metal Free Phthalonitrile Derivatives for Enhancement of the Dye Sensitized Solar Cells. Acta Phys. Pol. A 2011, 119, 395–404. [Google Scholar] [CrossRef]
- Holland, J.P.; Green, J.C. Evaluation of Exchange-Correlation Functionals for Time-Dependent Density Functional Theory Calculations on Metal Complexes. J. Comput. Chem. 2010, 31, 1008–1014. [Google Scholar] [CrossRef] [PubMed]
- Elijošiutė, E.; Jankūnaitė, D.; Eicher-Lorka, O. TD-DFT Study of the Electronic Absorption Spectra of Iron(III) Monoisothiocyanate. Polyhedron 2015, 90, 41–46. [Google Scholar] [CrossRef]
- Lopes, J.M.S.; Sharma, K.; Sampaio, R.N.; Batista, A.A.; Ito, A.S.; Machado, A.E.H.; Araújo, P.T.; Barbosa Neto, N.M. Novel Insights on the Vibronic Transitions in Free Base Meso-Tetrapyridyl Porphyrin. Spectrochim. Acta A Mol. Biomol. Spectrosc. 2019, 209, 274–279. [Google Scholar] [CrossRef]
- Song, Y.; Schubert, A.; Maret, E.; Burdick, R.K.; Dunietz, B.D.; Geva, E.; Ogilvie, J.P. Vibronic Structure of Photosynthetic Pigments Probed by Polarized Two-Dimensional Electronic Spectroscopy and Ab Initio Calculations. Chem. Sci. 2019, 10, 8143–8153. [Google Scholar] [CrossRef]
- Algorri, J.F.; Ochoa, M.; Roldán-Varona, P.; Rodríguez-Cobo, L.; López-Higuera, J.M. Light Technology for Efficient and Effective Photodynamic Therapy: A Critical Review. Cancers 2021, 13, 3484. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Hao, Y.; Chen, S.; Xu, M. Photodynamic Therapy of Cancers With Internal Light Sources: Chemiluminescence, Bioluminescence, and Cerenkov Radiation. Front. Chem. 2020, 8, 770. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Lin, L. Internal Light Source for Deep Photodynamic Therapy. Light Sci. Appl. 2022, 11, 85. [Google Scholar] [CrossRef] [PubMed]
- Laptev, R.; Nisnevitch, M.; Siboni, G.; Malik, Z.; Firer, M.A. Intracellular Chemiluminescence Activates Targeted Photodynamic Destruction of Leukaemic Cells. Br. J. Cancer 2006, 95, 189–196. [Google Scholar] [CrossRef]
- Maytin, E.V.; Kaw, U.; Ilyas, M.; Mack, J.A.; Hu, B. Blue Light versus Red Light for Photodynamic Therapy of Basal Cell Carcinoma in Patients with Gorlin Syndrome: A Bilaterally Controlled Comparison Study. Photodiagn. Photodyn. Ther. 2018, 22, 7–13. [Google Scholar] [CrossRef]
- Akasov, R.A.; Sholina, N.V.; Khochenkov, D.A.; Alova, A.V.; Gorelkin, P.V.; Erofeev, A.S.; Generalova, A.N.; Khaydukov, E.V. Photodynamic Therapy of Melanoma by Blue-Light Photoactivation of Flavin Mononucleotide. Sci. Rep. 2019, 9, 9679. [Google Scholar] [CrossRef]
- Xie, L.; Ji, X.; Zhang, Q.; Wei, Y. Curcumin Combined with Photodynamic Therapy, Promising Therapies for the Treatment of Cancer. Biomed. Pharmacother. 2022, 146, 112567. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, P.M.; Lopes, T.Z.; Tedesco, A.C.; Rahal, P.; Calmon, M.F. Effect of Berberine Associated with Photodynamic Therapy in Cell Lines. Photodiagn. Photodyn. Ther. 2020, 32, 102045. [Google Scholar] [CrossRef] [PubMed]
- Mugas, M.L.; Calvo, G.; Marioni, J.; Céspedes, M.; Martinez, F.; Sáenz, D.; Di Venosa, G.; Cabrera, J.L.; Montoya, S.N.; Casas, A. Photodynamic Therapy of Tumour Cells Mediated by the Natural Anthraquinone Parietin and Blue Light. J. Photochem. Photobiol. B 2021, 214, 112089. [Google Scholar] [CrossRef]
- Wang, K.; Liu, L.; Qi, G.; Chao, X.; Ma, W.; Yu, Z.; Pan, Q.; Mao, Z.; Liu, B. Light-Driven Cascade Mitochondria-to-Nucleus Photosensitization in Cancer Cell Ablation. Adv. Sci. 2021, 8, 2004379. [Google Scholar] [CrossRef] [PubMed]
- Desgranges, S.; Juzenas, P.; Vasovic, V.; Gederaas, O.A.; Lindgren, M.; Warloe, T.; Peng, Q.; Contino-Pépin, C. Amphiphilic Protoporphyrin IX Derivatives as New Photosensitizing Agents for the Improvement of Photodynamic Therapy. Biomedicines 2022, 10, 423. [Google Scholar] [CrossRef]
- Čunderlíková, B.; Vasovič, V.; Sieber, F.; Furre, T.; Borgen, E.; Nesland, J.M.; Peng, Q. Hexaminolevulinate-Mediated Photodynamic Purging of Marrow Grafts with Murine Breast Carcinoma. Bone Marrow Transplant. 2011, 46, 1118–1127. [Google Scholar] [CrossRef]
- Moghassemi, S.; Dadashzadeh, A.; de Azevedo, R.B.; Amorim, C.A. Secure Transplantation by Tissue Purging Using Photodynamic Therapy to Eradicate Malignant Cells. J. Photochem. Photobiol. B 2022, 234, 112546. [Google Scholar] [CrossRef]
- Daneshmand, S.; Schuckman, A.K.; Bochner, B.H.; Cookson, M.S.; Downs, T.M.; Gomella, L.G.; Grossman, H.B.; Kamat, A.M.; Konety, B.R.; Lee, C.T.; et al. Hexaminolevulinate Blue-Light Cystoscopy in Non-Muscle-Invasive Bladder Cancer: Review of the Clinical Evidence and Consensus Statement on Appropriate Use in the USA. Nat. Rev. Urol. 2014, 11, 589–596. [Google Scholar] [CrossRef]
- Caputo, E.; Maiorana, L.; Vasta, V.; Pezzino, F.M.; Sunkara, S.; Wynne, K.; Elia, G.; Marincola, F.M.; McCubrey, J.A.; Libra, M.; et al. Characterization of Human Melanoma Cell Lines and Melanocytes by Proteome Analysis. Cell Cycle 2011, 10, 2924–2936. [Google Scholar] [CrossRef]
- Huang, Y.-Y.; Vecchio, D.; Avci, P.; Yin, R.; Garcia-Diaz, M.; Hamblin, M.R. Melanoma Resistance to Photodynamic Therapy: New Insights. Biol. Chem. 2013, 394, 239–250. [Google Scholar] [CrossRef] [PubMed]
- Tudor, D.; Nenu, I.; Filip, G.A.; Olteanu, D.; Cenariu, M.; Tabaran, F.; Ion, R.M.; Gligor, L.; Baldea, I. Combined Regimen of Photodynamic Therapy Mediated by Gallium Phthalocyanine Chloride and Metformin Enhances Anti-Melanoma Efficacy. PLoS ONE 2017, 12, e0173241. [Google Scholar] [CrossRef]
- Hossain, M.R.; Ansary, T.M.; Komine, M.; Ohtsuki, M. Diversified Stimuli-Induced Inflammatory Pathways Cause Skin Pigmentation. Int. J. Mol. Sci. 2021, 22, 3970. [Google Scholar] [CrossRef] [PubMed]
- Arslanbaeva, L.; Tosi, G.; Ravazzolo, M.; Simonato, M.; Tucci, F.A.; Pece, S.; Cogo, P.; Santoro, M.M. UBIAD1 and CoQ10 Protect Melanoma Cells from Lipid Peroxidation-Mediated Cell Death. Redox Biol. 2022, 51, 102272. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.; Zhou, T.; Bai, R.; Xie, Y. Chemical Approaches for the Enhancement of Porphyrin Skeleton-Based Photodynamic Therapy. J. Enzyme Inhib. Med. Chem. 2020, 35, 1080–1099. [Google Scholar] [CrossRef]
- Králová, J.; Bříza, T.; Moserová, I.; Dolenský, B.; Vašek, P.; Poučková, P.; Kejík, Z.; Kaplánek, R.; Martásek, P.; Dvořák, M.; et al. Glycol Porphyrin Derivatives as Potent Photodynamic Inducers of Apoptosis in Tumor Cells. J. Med. Chem. 2008, 51, 5964–5973. [Google Scholar] [CrossRef]
- Frisch, M.J.; Trucks, G.W.; Schlegel, H.B.; Scuseria, G.E.; Robb, M.A.; Cheeseman, J.R.; Scalmani, G.; Barone, V.; Mennucci, B.; Petersson, G.A.; et al. Gaussian~09 Revision E.01.; Gaussian, Inc.: Wallingford, CT, USA, 2009. [Google Scholar]
- Chemcraft—Graphical Program for Visualization of Quantum Chemistry Computations. Available online: https://www.chemcraftprog.com/ (accessed on 6 July 2022).
- Epelde-Elezcano, N.; Martínez-Martínez, V.; Peña-Cabrera, E.; Gómez-Durán, C.F.A.; Arbeloa, I.L.; Lacombe, S. Modulation of Singlet Oxygen Generation in Halogenated BODIPY Dyes by Substitution at Their: Meso Position: Towards a Solvent-Independent Standard in the Vis Region. RSC Adv. 2016, 6, 41991–41998. [Google Scholar] [CrossRef]
- Khurana, R.; Kakatkar, A.S.; Chatterjee, S.; Barooah, N.; Kunwar, A.; Bhasikuttan, A.C.; Mohanty, J. Supramolecular Nanorods of (N-Methylpyridyl) Porphyrin with Captisol: Effective Photosensitizer for Anti-Bacterial and Anti-Tumor Activities. Front. Chem. 2019, 7, 452. [Google Scholar] [CrossRef]
- Kucinska, M.; Plewinski, A.; Szczolko, W.; Kaczmarek, M.; Goslinski, T.; Murias, M. Modeling the Photodynamic Effect in 2D versus 3D Cell Culture under Normoxic and Hypoxic Conditions. Free Radic. Biol. Med. 2021, 162, 309–326. [Google Scholar] [CrossRef]











| Experimental Band Maximum (nm) | Simmulated Band Maximum (nm) | Transition Number | λ (nm) | EE 1 (eV) | OS 2 (f) | Orbital Transition Composition 3 (% of Contribution) | Type | Band 4 |
|---|---|---|---|---|---|---|---|---|
| 597 | 592 | 1 | 591.757 | 2.095 | 0.106 | HOMO → LUMO (73), HOMO-1 → LUMO+1 (24) | π-π* | Q |
| 564 | 557 | 2 | 557.636 | 2.223 | 0.157 | HOMO → LUMO+1 (73), HOMO-1 → LUMO (25) | π-π* | Q |
| 426 | 428 | 3 | 430.757 | 2.878 | 1.023 | HOMO-1 → LUMO+1 (43), HOMO-2 → LUMO (21) | π-π* | B |
| 426 | 428 | 4 | 426.167 | 2.909 | 1.061 | HOMO-1 → LUMO (37), HOMO-2 → LUMO (26) | π-π* | B |
| Experimental Band Maximum (nm) | Simmulated Band Maximum (nm) | Transition Number | λ (nm) | EE 1 (eV) | OS 2 (f) | Orbital Transition Composition 3 (% of Contribution) | Type | Band 4 |
|---|---|---|---|---|---|---|---|---|
| 597 | 597 | 1 | 596.454 | 2.079 | 0.150 | HOMO → LUMO (76), HOMO-1 → LUMO+1 (22) | π-π* | Q |
| 564 | 564 | 2 | 563.773 | 2.199 | 0.227 | HOMO → LUMO+1 (77), HOMO-1 → LUMO (22) | π-π* | Q |
| 426 | 426 | 3 | 428.806 | 2.891 | 1.177 | HOMO-1 → LUMO+1 (48) | π-π* | B |
| 426 | 426 | 4 | 423.431 | 2.928 | 1.273 | HOMO-1 → LUMO (48) | π-π* | B |
| Experimental Band Maximum (nm) | Simmulated Band Maximum (nm) | Transition Number | λ (nm) | EE 1 (eV) | OS 2 (f) | Orbital Transition Composition 3 (% of Contribution) | Type | Band 4 |
|---|---|---|---|---|---|---|---|---|
| 561 | 563 | 1 | 563.030 | 2.202 | 0.139 | HOMO → LUMO (71), HOMO-1 → LUMO+1 (24] | π-π* | Q |
| 561 | 563 | 2 | 563.030 | 2.202 | 0.139 | HOMO → LUMO+1 (71), HOMO-1 → LUMO (24) | π-π* | Q |
| 431 | 420 | 3 | 419.747 | 2.954 | 1.429 | HOMO-1 → LUMO+1 (38) HOMO-1 → LUMO (26) | π-π* | B |
| 431 | 420 | 4 | 419.747 | 2.954 | 1.429 | HOMO-1 → LUMO (38), HOMO-1 → LUMO+1 (26) | π-π* | B |
| 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|
| ΦΔ | 0.54 | 0.53 | 0.43 | 0.4 | 0.06 | 0.05 |
| Compound | IC50 [nM] | |||||
|---|---|---|---|---|---|---|
| 5637 | LNCaP | A375 | ||||
| 0 J/cm2 | 10 J/cm2 | 0 J/cm2 | 10 J/cm2 | 0 J/cm2 | 10 J/cm2 | |
| 3 | >250 | 8.01 ± 2.12 | >250 | 49.71 ± 11.55 | >1000 | 754.69 ± 145.56 |
| 4 | >250 | 32.13 ± 3.86 | >1000 | 44.91 ± 1.98 | >1000 | 250.59 ± 64.51 |
| 5 | >1000 | 79.71 ± 7.08 | >1000 | 106.00 ± 26.27 | >1000 | 578.01 ± 25.44 |
| 6 | >250 | 15.56 ± 3.50 | >250 | 48.63 ± 13.21 | >1000 | 284.56 ± 83.21 |
| 7 | >1000 | 149.92 ± 42.12 | >1000 | 557.75 ± 104.99 | >1000 | >1000 |
| 8 | >1000 | 247.94 ± 45.45 | >1000 | 333.53 ± 116.33 | >1000 | >1000 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lazewski, D.; Kucinska, M.; Potapskiy, E.; Kuzminska, J.; Tezyk, A.; Popenda, L.; Jurga, S.; Teubert, A.; Gdaniec, Z.; Kujawski, J.; et al. Novel Short PEG Chain-Substituted Porphyrins: Synthesis, Photochemistry, and In Vitro Photodynamic Activity against Cancer Cells. Int. J. Mol. Sci. 2022, 23, 10029. https://doi.org/10.3390/ijms231710029
Lazewski D, Kucinska M, Potapskiy E, Kuzminska J, Tezyk A, Popenda L, Jurga S, Teubert A, Gdaniec Z, Kujawski J, et al. Novel Short PEG Chain-Substituted Porphyrins: Synthesis, Photochemistry, and In Vitro Photodynamic Activity against Cancer Cells. International Journal of Molecular Sciences. 2022; 23(17):10029. https://doi.org/10.3390/ijms231710029
Chicago/Turabian StyleLazewski, Dawid, Malgorzata Kucinska, Edward Potapskiy, Joanna Kuzminska, Artur Tezyk, Lukasz Popenda, Stefan Jurga, Anna Teubert, Zofia Gdaniec, Jacek Kujawski, and et al. 2022. "Novel Short PEG Chain-Substituted Porphyrins: Synthesis, Photochemistry, and In Vitro Photodynamic Activity against Cancer Cells" International Journal of Molecular Sciences 23, no. 17: 10029. https://doi.org/10.3390/ijms231710029