Heat-Related Deaths in Hot Cities: Estimates of Human Tolerance to High Temperature Thresholds
Abstract
:Introduction
2. Experimental Section
2.1. Study Region

2.2. Data
| Month | ATmax Mean | ATmax SD | ATmax Minimum | ATmax Maximum |
|---|---|---|---|---|
| May | 92 | 9.2 | 66 | 111 |
| June | 103 | 6.3 | 85 | 118 |
| July | 107 | 4.6 | 93 | 118 |
| August | 105 | 5.3 | 87 | 118 |
| September | 99 | 6.4 | 80 | 113 |
| October | 84 | 8.3 | 60 | 104 |

 = average deaths per day in summer of year I; Ni = number of days in year i from May–October.
= average deaths per day in summer of year I; Ni = number of days in year i from May–October.2.3. Statistical Analysis
spline(ATmax-3-day-lag) + β1 × heat wave

3. Results and Discussion
3.1. Results
| Cause of Death a | Number of County Resident Deaths | Percent Resident Deaths of All Deaths c | Threshold ATmax (°F) (Lag Days) d | RR above Threshold e | 95% CI f |
|---|---|---|---|---|---|
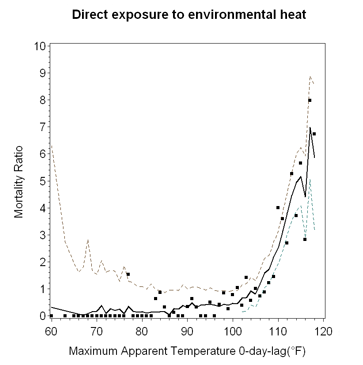
| Direct exposure to environmental heat | 215 | 73.1 | 93 (0) | 1.20 | 1.16, 1.23 |
| Dehydration | 409 | 93.8 | |||
| Possible consequences of heat or dehydration | 1114 | 92.1 | 106 (0) | 1.05 | 1.01, 1.09 |
| Cardiac disease/stroke | 24,717 | 91.2 | 110 (1) | 1.03 | 1.01, 1.05 |
| Chronic renal failure | 762 | 89.8 | |||
| Heart failure | 848 | 92.0 | |||
| Chronic obstructive pulmonary diseases (COPD)/asthma | 5342 | 92.5 | |||
| Other respiratory diseases | 3639 | 89.3 | |||
| All causes b | 90,284 | 91.4 | 107 (1) | 1.01 | 1.00, 1.02 |

| <65 Years | ≥65 Years | |||||
|---|---|---|---|---|---|---|
| Cause of Death a | Threshold ATmax (°F) (Lag Days) c | RR above Threshold d | 95% CI e | Threshold ATmax (°F) (Lag Days) c | RR above Threshold d | 95% CI e |
| Direct exposure to environmental heat | 93 (0) | 1.19 | 1.15, 1.24 | 90 (0) | 1.21 | 1.15, 1.26 |
| Possible consequences of heat ordehydration | 106 (0) | 1.12 | 1.02, 1.23 | |||
| Cardiac disease/stroke | 106 (1) | 1.03 | 1.00, 1.05 | 109 (1) | 1.03 | 1.01, 1.05 |
| Chronic obstructive pulmonary diseases (COPD)/asthma | 110 (0) | 1.05 | 1.00, 1.10 | |||
| All causes b | 104 (1) | 1.01 | 1.00, 1.02 | 107 (1) | 1.01 | 1.00, 1.02 |
| Male < 65 Years | Male ≥ 65 Years | |||||
|---|---|---|---|---|---|---|
| Cause of Death a | Threshold ATmax (°F) (Lag Days) c | RR above Threshold d | 95% CI e | Threshold ATmax (°F) (Lag Days) c | RR above Threshold d | 95% CI e |
| Direct exposure to environmental heat | 92 (0) | 1.19 | 1.15, 1.24 | 90 (0) | 1.21 | 1.14, 1.29 |
| Possible consequences of heat or dehydration | 106 (0) | 1.18 | 1.06, 1.33 | |||
| Other respiratory diseases | 109 (0) | 1.09 | 1.01, 1.16 | |||
| All causes b | 102 (1) | 1.01 | 1.00, 1.02 | |||
| Female < 65 Years | Female ≥ 65 Years | |||||
|---|---|---|---|---|---|---|
| Cause-of-Death Category a | Threshold ATmax (°F) (Lag Days) c | RR above Threshold d | 95% CI e | Threshold ATmax (°F) (Lag Days) c | RR above Threshold d | 95% CI e |
| Direct exposure to environmental heat | 97 (0) | 1.19 | 1.08, 1.31 | 90 (0) | 1.20 | 1.12, 1.28 |
| Possible consequences of heat or dehydration | 105 (0) | 1.05 | 1.01, 1.10 | |||
| Cardiac disease/stroke | 106 (1) | 1.05 | 1.01, 1.09 | 108 (1) | 1.03 | 1.01, 1.05 |
| Chronic obstructive pulmonary diseases (COPD)/asthma | 109 (0) | 1.07 | 1.02, 1.13 | |||
| All causes b | 107 (1) | 1.02 | 1.00, 1.04 | 107 (1) | 1.01 | 1.00, 1.02 |
3.2. Discussion
3.2.1. Heat Thresholds and Mortality
3.2.2. Implications of Climate Change for Future Heat Mortality
4. Conclusions
Supplementary Files
Acknowledgements
Author Contributions
Conflicts of Interest
References
- Bell, M.L.; O’Neill, M.S.; Ranjit, N.; Borja-Aburto, V.H.; Cifuentes, L.A.; Gouveia, N.C. Vulnerability to heat-related mortality in Latin America: A case-crossover study in Sao Paulo, Brazil, Santiago, Chile and Mexico City, Mexico. Int. J. Epidemiol. 2008, 37, 796–780. [Google Scholar] [CrossRef]
- Curriero, F.C.; Heiner, K.S.; Samet, J.M.; Zeger, S.L.; Strug, L.; Patz, J.A. Temperature and mortality in 11 cities of the eastern United States. Am. J. Epidemiol. 2002, 155, 80–87. [Google Scholar] [CrossRef]
- D'Ippoliti, D.; Michelozzi, P.; Marino, C.; de’Donato, F.; Menne, B.; Katsouyanni, K.; Kirchmayer, U.; Analitis, A.; Medina-Ramón, M.; Paldy, A.; et al. The impact of heat waves on mortality in 9 European cities: Results from the EuroHEAT project. Environ. Health 2010, 9, 37. [Google Scholar] [CrossRef]
- McMichael, A.J.; Wilkinson, P.; Kovats, R.S.; Pattenden, S.; Hajat, S.; Armstrong, B.; Vajanapoom, N.; Niciu, E.M.; Mahomed, H.; Kingkeow, C.; et al. International study of temperature, heat and urban mortality: The “ISOTHURM” project. Int. J. Epidemiol. 2008, 37, 1121–1131. [Google Scholar] [CrossRef]
- Son, J.Y.; Lee, J.T.; Anderson, G.B.; Bell, M.L. The impact of heat waves on mortality in seven major cities in Korea. Environ. Health. Perspect. 2012, 120, 566–571. [Google Scholar] [CrossRef]
- Tong, S.; Wang, X.Y.; Barnett, G.A. Assessment of heat-related health impacts in Brisbane, Australia: Comparison of different heat wave definitions. PLOS ONE 2010, 5. [Google Scholar] [CrossRef] [Green Version]
- Egondi, T.; Kyobutungi, C.; Kovats, S.; Muindi, K.; Ettarh, R.; Rocklov, J. Time-series analyses of weather and mortality patterns in Nairobi’s informal settlements. Global Health Action. 2012, 5. Available online: http://www.globalhealthaction.net/index.php/gha/article/view/19065 (accessed on 23 January 2014).
- Anderson, G.B.; Bell, M.L. Heat waves in the United States: Mortality risk during heat waves and effect modification by heat wave characteristics in 43 U.S. communities. Environ. Health Persp. 2011, 119, 210–218. [Google Scholar] [CrossRef]
- Hajat, S.; Kosatsky, T. Heat-related mortality: A review and exploration of heterogeneity. J. Epidemiol. Commun. H. 2010, 64, 753–760. [Google Scholar] [CrossRef]
- Peretz, C.; Biggeri, A.; Alpert, P.; Baccini, M. The Effect of Heat Stress on Daily Mortality in Tel Aviv, Israel. In National Security and Human Health Implications of Climate Change; Fernando, H.J., Klaic, Z.B., McCulley, J.L., Eds.; Springer: New York, NY, USA, 2012; pp. 241–251. [Google Scholar]
- Balogun, A.A.; Balogun, I.A.; Adeyewa, Z.D. Comparisons of urban and rural heat stress conditions in a hot-humid tropical city. Glob. Health Action 2010, 3, 5614. [Google Scholar] [CrossRef]
- Contribution of Working Group I to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change; Solomon, S.; Qin, D.; Manning, M.; Chen, Z.; Marquis, M.; Averyt, K.B.; Tignor, M.; Miller, H.L. (Eds.) Cambridge University Press: Cambridge, UK, 2007.
- Grimmond, S.B. Urbanization and global environmental change: Local effects of urban warming. The Geogr. J. 2007, 173, 83–88. [Google Scholar] [CrossRef]
- Osborn, L. Hottest Cities in the World. Current Results: Research News & Science Facts. Available online: http://www.currentresults.com/Weather-Extremes/hottest-cities-in-the-world.php (accessed on 16 December 2013).
- World Health Organization. Civil Registration: Why Counting Births and Deaths is Important. Fact Sheet No. 324. April 2013. Available online: http://www.who.int/mediacentre/factsheets/fs324/en/ (accessed on 16 December 2013).
- Haque, A.S.; Shamim, K.; Siddiqui, N.H.; Irfan, M.; Khan, J.A. Death certificate completion skills of hospital physicians in a developing country. BMC Health Serv. Res. 2013, 13. [Google Scholar] [CrossRef]
- Rao, C.; Bradshaw, D.; Mathers, C.D. Improving death registrations and statistics in developing countries: Lessons from sub-Saharan Africa. S. Afr. J. Demogr. 2004, 9, 81–99. [Google Scholar]
- National Oceanic and Atmospheric Administration. Comparative Climatic Data for the United States through 2012. Available online: http://www1.ncdc.noaa.gov/pub/data/ccd-data/CCD-2012.pdf (accessed on 8 January 2014).
- Grossman-Clarke, S.; Zehnder, J.A.; Loridan, T.; Grimmond, S.B. Contribution of land use changes to near-surface air temperatures during recent summer extreme heat events in the Phoenix metropolitan area. J. Clim. 2010, 49, 1649–1664. [Google Scholar]
- Chow, W.T.L.; Brennan, D.; Brazel, A.J. Urban heat island research in Phoenix, Arizona: Theoretical contributions and policy applications. Bull. Amer. Meteor. Soc. 2012, 93, 517–530. [Google Scholar] [CrossRef]
- Brazel, A.; Selover, N.; Vose, R.; Heisler, G. The tale of two climates—Baltimore and Phoenix urban LTER sites. Clim. Res. 2000, 15, 123–135. [Google Scholar] [CrossRef]
- Ruddell, D.; Hoffman, D; Ahmad, O.; Brazel, A. Historical threshold temperatures for Phoenix (Urban) and Gila Bend (Desert), Central Arizona, USA. Clim. Res. 2013, 55, 201–215. [Google Scholar] [CrossRef]
- Georgescu, M.; Moustaoui, M.; Mahalov, A.; Dudhia, J. Summer-time climate impacts of projected megapolitan expansion in Arizona. Nat. Clim. Chang. 2012, 3, 37–41. [Google Scholar] [CrossRef]
- Ruddell, D.M.; Harlan, S.L.; Grossman-Clarke, S.; Buyantuyev, A. Risk and Exposure to Extreme Heat in Microclimates of Phoenix, AZ. In Geospatial Techniques in Urban Hazard and Disaster Analysis; Showalter, P., Lu, Y., Eds.; Springer: New York, NY, USA, 2010; pp. 179–202. [Google Scholar]
- Zhang, K.; Oswald, E.M.; Brown, D.G.; Brines, S.J.; Gronlund, C.J.; White-Newsome, J.L.; Rood, R.B.; O’Neill, M.S. Geospatial exploration of spatial variation of summertime temperatures in the Detroit metropolitan region. Environ. Res. 2011, 111, 1046–1053. [Google Scholar] [CrossRef]
- Braga, A.L.F.; Zanobetti, A.; Schwartz, J. The time course of weather-related deaths. Epidemiology 2001, 12, 662–667. [Google Scholar] [CrossRef]
- Steadman, R.G. The assessment of sultriness. Part I: A temperature-humidity index based on human physiology and clothing science. J. Appl. Meteor. 1979, 18, 861–873. [Google Scholar] [CrossRef]
- Basu, R. High ambient temperature and mortality: A review of epidemiologic studies from 2001–2008. Environ. Health 2009, 8, 1–13. [Google Scholar] [CrossRef]
- Kalkstein, L.S.; Valimont, K.M. An evaluation of summer discomfort in the United States using a relative climatological index. Bull. Amer. Meteor. Soc. 1986, 67, 842–848. [Google Scholar] [CrossRef]
- Steadman, R.G. The assessment of sultriness. Part II: Effects of wind, extra radiation and barometric pressure on apparent temperature. J. Appl. Meteor. 1979, 18, 874–885. [Google Scholar] [CrossRef]
- Barnett, A.G. Temperature and cardiovascular deaths in the U.S. elderly: Changes over time. Epidemiology 2007, 18, 369–372. [Google Scholar] [CrossRef]
- Basu, R.; Dominici, F.; Samet, J.M. Temperature and mortality among the elderly in the United States: A comparison of epidemiologic methods. Epidemiology 2005, 16, 58–66. [Google Scholar] [CrossRef]
- Braga, A.L.F.; Zanobetti, A.; Schwartz, J. The effect of weather on respiratory and cardiovascular deaths in 12 U.S. cities. Environ. Health Perspect. 2002, 110, 859–863. [Google Scholar]
- Vaneckova, P.; Beggs, P.J.; de Dear, R.J.; McCracken, K.W. Effect of temperature on mortality during the six warmer months in Sydney, Australia between 1993 and 2004. Environ. Res. 2008, 108, 361–369. [Google Scholar] [CrossRef]
- Basu, R.; Feng, W.; Ostro, B.D. Characterizing temperature and mortality in nine California counties, 1999–2003. Epidemiology 2008, 19, 138–145. [Google Scholar] [CrossRef]
- Medina-Ramón, M.; Zanobetti, A.; Cavanaugh, D.P.; Schwartz, J. Extreme temperatures and mortality: Assessing effect modification by personal characteristics and specific cause of death in a multi-city case-only analysis. Environ. Health Perspect. 2006, 114, 1331–1336. [Google Scholar] [CrossRef]
- Meehl, G.A.; Tebaldi, C. More intense, more frequent, and longer lasting heat waves in the 21st century. Science 2004, 305, 994–997. [Google Scholar] [CrossRef]
- Yip, F.Y.; Flanders, W.; Wolkin, A; Engelthaler, D.; Humble, W.; Neri, A.; Lewis, L.; Backer, L.; Rubin, C. The impact of excess heat events in Maricopa County, Arizona: 2000–2005. Int. J. Biometeorol. 2008, 52, 765–772. [Google Scholar] [CrossRef]
- Maricopa County Department of Public Health. Annual Heat Reports 2007–2011. Available online: http://www.maricopa.gov/publichealth/Services/EPI/Reports/heat.aspx (accessed on 17 October 2013).
- Golden, J.; Hart, D.; Brazel, A.; Luber, G.; Phelan, P. A biometeorology study of climate and heat-related morbidity in Phoenix from 2001 to 2006. Int. J. Biometeorol. 2008, 52, 471–480. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention (CDC). Heat-related deaths—United States, 1999–2003. In Morb. Mortal Wkly. Rep.; 2006; 55, pp. 796–798. [Google Scholar]
- National Oceanic and Atmospheric Administration (NOAA). Heat Wave: A Major Summer Killer. U.S. Department of Commerce. Available online: http://www.nws.noaa.gov/om/brochures/heatwave.pdf (accessed on 17 October 2013).
- Petitti, D.B.; Harlan, S.L.; Chowell-Puente, G.; Ruddell, D. Occupation and environmental heat-associated deaths in Maricopa County, Arizona: A case-control study. PLOS ONE 2013, 8, e62596. [Google Scholar] [CrossRef]
- Sanchez, C. Tricks of the Shade: Heat-related Coping Strategies of Urban Homeless Persons in Phoenix, Arizona. Master Thesis, Arizona State University, Tempe, AZ, USA, 2011. [Google Scholar]
- Harlan, S.L.; Brazel, A.; Prashad, L.; Stefanov, W.L.; Larsen, L. Neighborhood microclimates and vulnerability to heat stress. Soc. Sci. Med. 2006, 63, 2847–2863. [Google Scholar] [CrossRef]
- Maricopa County Department of Public Health. Annual Heat Reports 2012. Available online: http://www.maricopa.gov/publichealth/Services/EPI/pdf/heat/2012annualreport.pdf (accessed on 17 October 2013).
- Basu, R.; Ostro, B.D. A multicounty analysis identifying the populations vulnerable to mortality associated with high ambient temperature in California. Am. J. Epidemiol. 2008, 168, 632–637. [Google Scholar] [CrossRef]
- Choi, G.; Choi, J.; Kwon, H. The impact of high apparent temperature on the increase of summertime disease-related mortality in Seoul: 1991–2000. J. Prev. Med. Public Health 2005, 38, 283–290. [Google Scholar]
- Díaz, J.; Jordán, A.; Garcia, R.; López, C.; Alberdi, J.C.; Hernández, E.; Otero, A. Heat waves in Madrid 1986–1997: Effects on the health of the elderly. Int. Arch. Environ. Occup. Health 2002, 75, 163–170. [Google Scholar] [CrossRef]
- Rainham, D.G.C.; Smoyer-Tomic, K.E. The role of air pollution in the relationship between a heat stress index and human mortality in Toronto. Environ. Res. 2003, 93, 9–19. [Google Scholar] [CrossRef]
- Grogan, H.; Hopkins, P.M. Heat stroke: Implications for critical care and anaesthesia. Br. J. Anaesth. 2002, 88, 700–707. [Google Scholar] [CrossRef]
- Muggeo, V.M.R. Modeling temperature effects on mortality: Multiple segmented relationships with common break points. Biostatistics 2008, 9, 613–620. [Google Scholar] [CrossRef]
- Harlan, S.L.; Declet-Barreto, J.H.; Stefanov, W.L.; Petitti, D.B. Neighborhood effects on heat deaths: Social and environmental predictors of vulnerability in Maricopa County, Arizona. Environ. Health Persp. 2013, 121, 197–204. [Google Scholar] [CrossRef]
- Guo, Y.; Barnett, A.G.; Tong, S. Spatiotemporal model or time series model for assessing city-wide temperature effects on mortality? Environ. Res. 2013, 120, 55–62. [Google Scholar] [CrossRef]
- Mearns, L.O.; Arritt, R.; Biner, S.; Bukovsky, M.S.; McGinnis, S.; Sain, S.; Caya, D.; Correia, J., Jr.; Flory, D.; Gutowski, W.; et al. The North American Regional Climate Change Assessment Program: Overview of Phase I results. BAMS 2012, 93, 1337–1362. [Google Scholar] [CrossRef]
- North American Regional Climate Change Assessment Program (NARCCAP). Available online: http://www.narccap.ucar.edu/about/index.html (accessed on 18 December 2013).
- Clarke, S.G.; Clarke, T.R.; Harlan, S.L. Extreme summer heat in Phoenix, Arizona (USA) under global climate change (2140–2070). Under review.
- Georgescu, M.; Moustaoui, M.; Mahalov, M.; Dudhia, J. An alternative explanation of the semiarid urban area “oasis effect”. J. Geophys. Res. Atmos. 2011, 116, p. D24113. Available online: http://dx.doi.org/10.1029/2011JD016720 (accessed on 23 January 2014).
- Davis, R.E.; Knappenberger, P.C.; Novicoff, W.M.; Michaels, P.J. Decadal changes in human heat-related mortality in the eastern United States. Clim. Res. 2002, 22, 175–184. [Google Scholar] [CrossRef]
- Barreca, A.; Clay, K.; Deschenes, O.; Greenstone, M.; Shapiro, J.S. Adapting to Climate Change: The Remarkable Decline in the U.S. Temperature-mortality Relationship over the 20th Century. Working Paper 18692. National Bureau of Economic Research, 2013. Available online: http://www.nber.org/papers/w18692 (accessed on 17 October 13).
- Bouchama, A.; Dehbi, M.; Mohamed, G.; Matthies, F.; Shoukri, M.; Menne, B. Prognostic factors in heat-wave related deaths: A meta-analysis. Arch. Intern. Med. 2007, 167, 2170–2176. [Google Scholar] [CrossRef]
- U.S. Bureau of the Census. 2011 American Community Housing Survey Metropolitan Areas. Table CO3AOM. Available online: http://www.census.gov/housing/ahs/data/2011ma.html (accessed on 17 October 2013).
- Hayden, M.H.; Brenkart-Smith, H.; Wilhelmi, O.V. Differential adaptive capacity to extreme heat: A Phoenix, Arizona case study. Weather Clim. Soc. 2011, 3, 269–280. [Google Scholar] [CrossRef]
- Overpeck, J.; Udall, B. Dry times ahead. Science 2010, 328, 1642–1643. [Google Scholar] [CrossRef]
- Sherwood, S.C.; Huber, M. An adaptability limit to climate change due to heat stress. P. Natl. Acad. Sci. USA 2010, 107, 9483–9484. [Google Scholar]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Harlan, S.L.; Chowell, G.; Yang, S.; Petitti, D.B.; Morales Butler, E.J.; Ruddell, B.L.; Ruddell, D.M. Heat-Related Deaths in Hot Cities: Estimates of Human Tolerance to High Temperature Thresholds. Int. J. Environ. Res. Public Health 2014, 11, 3304-3326. https://doi.org/10.3390/ijerph110303304
Harlan SL, Chowell G, Yang S, Petitti DB, Morales Butler EJ, Ruddell BL, Ruddell DM. Heat-Related Deaths in Hot Cities: Estimates of Human Tolerance to High Temperature Thresholds. International Journal of Environmental Research and Public Health. 2014; 11(3):3304-3326. https://doi.org/10.3390/ijerph110303304
Chicago/Turabian StyleHarlan, Sharon L., Gerardo Chowell, Shuo Yang, Diana B. Petitti, Emmanuel J. Morales Butler, Benjamin L. Ruddell, and Darren M. Ruddell. 2014. "Heat-Related Deaths in Hot Cities: Estimates of Human Tolerance to High Temperature Thresholds" International Journal of Environmental Research and Public Health 11, no. 3: 3304-3326. https://doi.org/10.3390/ijerph110303304