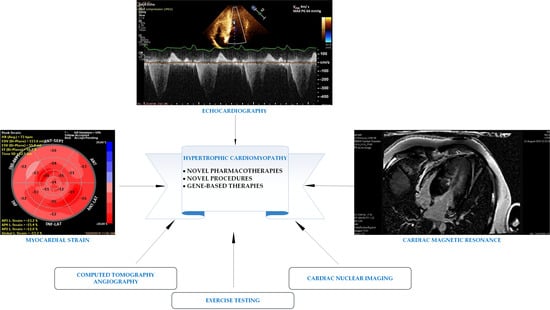
The Advantages of New Multimodality Imaging in Choosing the Optimal Management Strategy for Patients with Hypertrophic Cardiomyopathy
Abstract
:1. Introduction
2. Echocardiography
2.1. Left Ventricular Wall Thickness
2.2. Mitral Valve and Subvalvular Apparatus Morphology and Mitral Hemodynamics
2.3. Left Ventricular Outflow Obstruction
2.4. Left Atrial Enlargement
2.5. Left Ventricular Ejection Fraction
2.6. Diastolic Function
2.7. Apical Aneurysm
3. Myocardial Strain
4. Exercise Testing
5. Computed Tomography Angiography
6. Cardiac Nuclear Imaging
7. Cardiac Magnetic Resonance
8. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Tuohy, C.V.; Kaul, S.; Song, H.K.; Nazer, B.; Heitner, S.B. Hypertrophic cardiomyopathy: The future of treatment. Eur. J. Heart Fail. 2020, 22, 228–240. [Google Scholar] [CrossRef] [PubMed]
- Elliott, P.M.; Anastasakis, A.; Borger, M.A.; Borggrefe, M.; Cecchi, F.; Charron, P.; Hagege, A.A.; Lafont, A.; Limongelli, G.; Mahrholdt, H.; et al. 2014 ESC guidelines on diagnosis and management of hypertrophic cardiomyopathy: The Task Force for the diagnosis and management of hypertrophic cardiomyopathy of the European Society of Cardiology (ESC). Eur. Heart J. 2014, 35, 2733–2779. [Google Scholar] [PubMed]
- Makavos, G.; Κairis, C.; Tselegkidi, M.-E.; Karamitsos, T.; Rigopoulos, A.G.; Noutsias, M.; Ikonomidis, I. Hypertrophic cardiomyopathy: An updated review on diagnosis, prognosis, and treatment. Heart Fail. Rev. 2019, 24, 439–459. [Google Scholar] [CrossRef] [PubMed]
- Maron, B.J. Clinical course and management of hypertrophic cardiomyopathy. N. Engl. J. Med. 2018, 379, 655–668. [Google Scholar] [CrossRef] [PubMed]
- Spudich, J.A. Three perspectives on the molecular basis of hypercontractility caused by hypertrophic cardiomyopathy mutations. Pflug. Arch. 2019, 471, 701–717. [Google Scholar] [CrossRef] [Green Version]
- Maron, B.J.; Gardin, J.M.; Flack, J.M.; Gidding, S.S.; Kurosaki, T.T.; Bild, D.E. Prevalence of hypertrophic cardiomyopathy in a general population of young adults: Echocardiographic analysis of 4111 subjects in the CARDIA study. Circulation 1995, 92, 785–789. [Google Scholar] [CrossRef]
- Ramchand, J.; Fava, A.M.; Chetrit, M.; Desai, M.Y. Advanced imaging for risk stratification of sudden death in hypertrophic cardiomyopathy. Heart 2020, 106, 793–801. [Google Scholar] [CrossRef]
- Rowin, E.J.; Maron, B.J.; Maron, M.S. The hypertrophic cardiomyopathy phenotype viewed through the prism of multimodality imaging: Clinical and etiologic implications. JACC Cardiovasc. Imaging 2019, 13, 2002–2016. [Google Scholar] [CrossRef]
- Zou, Y.; Song, L.; Wang, Z.; Ma, A.; Liu, T.; Gu, H.; Lu, S.; Wu, P.; Zhang, Y.; Shen, L.; et al. Prevalence of idiopathic hypertrophic cardiomyopathy in China: A population-based echocardiographic analysis of 8080 adults. Am. J. Med. 2004, 116, 14–18. [Google Scholar] [CrossRef]
- Teare, D. Asymmetrical hypertrophy of the heart in young adults. Br. Heart J. 1958, 20, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Braunwald, E.; Lambrew, C.T.; Rockoff, S.D.; Ross, J., Jr.; Morrow, A.G. Idiopathic hypertrophic subaortic stenosis: A description of the disease based upon an analysis of 64 patients. Circulation 1964, 29, IV-3–IV-119. [Google Scholar] [CrossRef] [PubMed]
- Teekakirikul, P.; Zhu, W.; Huang, H.C.; Fung, E. Hypertrophic cardiomyopathy: An overview of genetics and management. Biomolecules 2019, 9, 878. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weissler-Snir, A.; Allan, K.; Cunningham, K.; Connelly, K.A.; Lee, D.S.; Spears, D.A.; Rakowski, H.; Dorian, P. Hypertrophic cardiomyopathy–related sudden cardiac death in young people in Ontario. Circulation 2019, 140, 1706–1716. [Google Scholar] [CrossRef] [PubMed]
- Marian, A.J.; Braunwald, E. Hypertrophic cardiomyopathy: Genetics, pathogenesis, clinical manifestations, diagnosis, and therapy. Circ. Res. 2017, 121, 749–770. [Google Scholar] [CrossRef]
- Cardim, N.; Galderisi, M.; Edvardsen, T.; Plein, S.; Popescu, B.A.; d’Andrea, A.; Bruder, O.; Cosyns, B.; Davin, L.; Donal, E. Role of multimodality cardiac imaging in the management of patients with hypertrophic cardiomyopathy: An expert consensus of the European Association of Cardiovascular Imaging Endorsed by the Saudi Heart Association. Eur. Heart J. Cardiovasc. Imag. 2015, 16, 280. [Google Scholar] [CrossRef]
- Geske, J.B.; Ommen, S.R.; Gersh, B.J. Hypertrophic cardiomyopathy: Clinical update. JACC Heart Fail. 2018, 6, 364–375. [Google Scholar] [CrossRef]
- Maron, B.J.; Rowin, E.J.; Casey, S.A.; Maron, M.S. How hypertrophic cardiomyopathy became a contemporary treatable genetic disease with low mortality: Shaped by 50 years of clinical research and practice. JAMA Cardiol. 2016, 1, 98–105. [Google Scholar] [CrossRef] [Green Version]
- Bois, J.P.; Geske, J.B.; Foley, T.A.; Ommen, S.R.; Pellikka, P.A. Comparison of maximal wall thickness in hypertrophic cardiomyopathy differs between magnetic resonance imaging and transthoracic echocardiography. Am. J. Cardiol. 2017, 119, 643–650. [Google Scholar] [CrossRef]
- Phelan, D.; Sperry, B.W.; Thavendiranathan, P.; Collier, P.; Popović, Z.B.; Lever, H.M.; Smedira, N.G.; Desai, M.Y. Comparison of ventricular septal measurements in hypertrophic cardiomyopathy patients who underwent surgical myectomy using multimodality imaging and implications for diagnosis and management. Am. J. Cardiol. 2017, 119, 1656–1662. [Google Scholar] [CrossRef]
- Maron, M.S.; Maron, B.J.; Harrigan, C.; Buros, J.; Gibson, C.M.; Olivotto, I.; Biller, L.; Lesser, J.R.; Udelson, J.E.; Manning, W.J.; et al. Hypertrophic cardiomyopathy phenotype revisited after 50 years with cardiovascular magnetic resonance. J. Am. Coll. Cardiol. 2009, 54, 220–228. [Google Scholar] [CrossRef] [Green Version]
- Maron, B.J.; Epstein, S.E. Clinical significance and therapeutic implications of the left ventricular outflow tract pressure gradient in hypertrophic cardiomyopathy. Am. J. Cardiol. 1986, 58, 1093–1096. [Google Scholar] [CrossRef]
- Maron, M.S.; Maron, B.J. Clinical impact of contemporary cardiovascular magnetic resonance imaging in hypertrophic cardiomyopathy. Circulation 2015, 132, 292–298. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gersh Bernard, J.; Maron Barry, J.; Bonow Robert, O.; Dearani Joseph, A.; Fifer Michael, A.; Link Mark, S.; Naidu Srihari, S.; Nishimura Rick, A.; Ommen Steve, R.; Rakowski Harry, S.C.E.; et al. ACCF/AHA Guideline for the diagnosis and treatment of hypertrophic cardiomyopathy: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2011, 124, e783–e831. [Google Scholar]
- Klarich, K.W.; Attenhofer Jost, C.H.; Binder, J.; Connolly, H.M.; Scott, C.G.; Freeman, W.K.; Ackerman, M.J.; Nishimura, R.A.; Tajik, A.J.; Ommen, S.R. Risk of death in long-term follow-up of patients with apical hypertrophic cardiomyopathy. Am. J. Cardiol. 2013, 111, 1784–1791. [Google Scholar] [CrossRef]
- Rowin, E.J.; Maron, B.J.; Haas, T.S.; Garberich, R.F.; Wang, W.; Link, M.S.; Maron, M.S. Hypertrophic cardiomyopathy with left ventricular apical aneurysm: Implications for risk stratification and management. J. Am. Coll. Cardiol. 2017, 69, 761–773. [Google Scholar] [CrossRef]
- Olivotto, I.; Hellawell, J.L.; Farzaneh-Far, R.; Blair, C.; Coppini, R.; Myers, J.; Belardinelli, L.; Maron, M.S. Novel approach targeting the complex pathophysiology of hypertrophic cardiomyopathy: The impact of late sodium current inhibition on exercise capacity in subjects with symptomatic hypertrophic cardiomyopathy (LIBERTY-HCM) trial. Circ. Heart Fail. 2016, 9, e002764. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nishimura, R.A.; Seggewiss, H.; Schaff, H.V. Hypertrophic obstructive cardiomyopathy: Surgical myectomy and septal ablation. Circ. Res. 2017, 121, 771–783. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, S.; Tuzcu, E.M.; Desai, M.Y.; Smedira, N.; Lever, H.M.; Lytle, B.W.; Kapadia, S.R. Updated meta-analysis of septal alcohol ablation versus myectomy for hypertrophic cardiomyopathy. J. Am. Coll. Cardiol. 2010, 55, 823–834. [Google Scholar] [CrossRef] [Green Version]
- Wigle, E.D. Cardiomyopathy: The diagnosis of hypertrophic cardiomyopathy. Heart 2001, 86, 709–714. [Google Scholar] [CrossRef] [Green Version]
- Sherrid, M.V.; Wever-Pinzon, O.; Shah, A.; Chaudhry, F.A. Reflections of inflections in hypertrophic cardiomyopathy. J. Am. Coll. Cardiol. 2009, 54, 212–219. [Google Scholar] [CrossRef]
- Veselka, J.; Anavekar, N.S.; Charron, P. Hypertrophic obstructive cardiomyopathy. Lancet 2017, 389, 1253–1267. [Google Scholar] [CrossRef]
- Kramer, C.M.; Appelbaum, E.; Desai, M.Y.; Desvigne-Nickens, P.; DiMarco, J.P.; Friedrich, M.G.; Geller, N.; Heckler, S.; Ho, C.Y.; Jerosch-Herold, M.; et al. Hypertrophic cardiomyopathy registry: The rationale and design of an international, observational study of hypertrophic cardiomyopathy. Am. Heart J. 2015, 170, 223–230. [Google Scholar] [CrossRef] [PubMed]
- Maron, M.S.; Olivotto, I.; Zenovich, A.G.; Link, M.S.; Pandian, N.G.; Kuvin, J.T.; Nistri, S.; Cecchi, F.; Udelson, J.E.; Maron, B.J. Hypertrophic cardiomyopathy is predominantly a disease of left ventricular outflow tract obstructio. Circulation 2006, 114, 2232–2239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nistri, S.; Olivotto, I.; Maron, M.S.; Ferrantini, C.; Coppini, R.; Grifoni, C.; Baldini, K.; Sgalambro, A.; Cecchi, F.; Maron, B.J. β Blockers for prevention of exercise-induced left ventricular outflow tract obstruction in patients with hypertrophic cardiomyopathy. Am. J. Cardiol. 2012, 110, 715–719. [Google Scholar] [CrossRef] [PubMed]
- Maron, M.S.; Olivotto, I.; Betocchi, S.; Casey, S.A.; Lesser, J.R.; Losi, M.A.; Cecchi, F.; Maron, B.J. Effect of left ventricular outflow tract obstruction on clinical outcome in hypertrophic cardiomyopathy. N. Engl. J. Med. 2003, 348, 295–303. [Google Scholar] [CrossRef] [PubMed]
- Gimeno, J.R.; Tomé-Esteban, M.; Lofiego, C.; Hurtado, J.; Pantazis, A.; Mist, B.; Lambiase, P.; McKenna, W.J.; Elliott, P.M. Exercise-induced ventricular arrhythmias and risk of sudden cardiac death in patients with hypertrophic cardiomyopathy. Eur. Heart J. 2009, 30, 2599–2605. [Google Scholar] [CrossRef] [Green Version]
- Lu, D.-Y.; Hailesealassie, B.; Ventoulis, I.; Liu, H.; Liang, H.-Y.; Nowbar, A.; Pozios, I.; Canepa, M.; Cresswell, K.; Luo, H.C. Impact of peak provoked left ventricular outflow tract gradients on clinical outcomes in hypertrophic cardiomyopathy. Int. J. Cardiol. 2017, 243, 290–295. [Google Scholar] [CrossRef]
- Dimitrow, P.P.; Bober, M.; Michałowska, J.; Sorysz, D. Left ventricular outflow tract gradient provoked by upright position or exercise in treated patients with hypertrophic cardiomyopathy without obstruction at rest. Echocardiography 2009, 26, 513–520. [Google Scholar] [CrossRef]
- Guttmann, O.P.; Rahman, M.S.; O’Mahony, C.; Anastasakis, A.; Elliott, P.M. Atrial fibrillation and thromboembolism in patients with hypertrophic cardiomyopathy: Systematic review. Heart 2014, 100, 465–472. [Google Scholar] [CrossRef]
- O’Mahony, C.; Jichi, F.; Pavlou, M.; Monserrat, L.; Anastasakis, A.; Rapezzi, C.; Biagini, E.; Gimeno, J.R.; Limongelli, G.; McKenna, W.J. A novel clinical risk prediction model for sudden cardiac death in hypertrophic cardiomyopathy (HCM risk-SCD). Eur. Heart J. 2014, 35, 2010–2020. [Google Scholar] [CrossRef]
- Spirito, P.; Autore, C.; Rapezzi, C.; Bernabò, P.; Badagliacca, R.; Maron, M.S.; Bongioanni, S.; Coccolo, F.; Estes, N.A.M.; Barillà, C.S. Syncope and risk of sudden death in hypertrophic cardiomyopathy. Circulation 2009, 119, 1703–1710. [Google Scholar] [CrossRef] [Green Version]
- Yang, W.I.; Shim, C.Y.; Kim, Y.J.; Kim, S.A.; Rhee, S.J.; Choi, E.Y.; Choi, D.; Jang, Y.; Chung, N.; Cho, S.Y. Left atrial volume index: A predictor of adverse outcome in patients with hypertrophic cardiomyopathy. J. Am. Soc. Echocardiogr. 2009, 22, 1338–1343. [Google Scholar] [CrossRef]
- Debonnaire, P.; Thijssen, J.; Leong, D.P.; Joyce, E.; Katsanos, S.; Hoogslag, G.E.; Schalij, M.J.; Atsma, D.E.; Bax, J.J.; Delgado, V. Global longitudinal strain and left atrial volume index improve prediction of appropriate implantable cardioverter defibrillator therapy in hypertrophic cardiomyopathy patients. Int. J. Cardiovasc. Imaging 2014, 30, 549–558. [Google Scholar] [CrossRef] [PubMed]
- Tower-Rader, A.; Kramer, C.M.; Neubauer, S.; Nagueh, S.F.; Desai, M.Y. Multimodality imaging in hypertrophic cardiomyopathy for risk stratification. Circ. Cardiovasc. Imaging 2020, 13, e009026. [Google Scholar] [CrossRef]
- Toepfer, C.N.; Wakimoto, H.; Garfinkel, A.C.; McDonough, B.; Liao, D.; Jiang, J.; Tai, A.C.; Gorham, J.M.; Lunde, I.G.; Lun, M. Hypertrophic cardiomyopathy mutations in MYBPC3 dysregulate myosin. Sci. Transl. Med. 2019, 11. [Google Scholar] [CrossRef] [PubMed]
- Penicka, M.; Gregor, P.; Kerekes, R.; Marek, D.; Curila, K.; Krupicka, J. Candesartan use in Hypertrophic And Non-obstructive Cardiomyopathy Estate (CHANCE) Study Investigators. The effects of candesartan on left ventricular hypertrophy and function in nonobstructive hypertrophic cardiomyopathy: A pilot, randomized study. J. Mol. Diagn. 2009, 11, 35–41. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Araujo, A.Q.; Arteaga, E.; Ianni, B.M.; Buck, P.C.; Rabello, R.; Mady, C. Effect of Losartan on left ventricular diastolic function in patients with nonobstructive hypertrophic cardiomyopathy. Am. J. Cardiol. 2005, 96, 1563–1567. [Google Scholar] [CrossRef] [PubMed]
- Biagini, E.; Spirito, P.; Rocchi, G.; Ferlito, M.; Rosmini, S.; Lai, F.; Lorenzini, M.; Terzi, F.; Bacchi-Reggiani, L.; Boriani, G.; et al. Prognostic implications of the Doppler restrictive filling pattern in hypertrophic cardiomyopathy. Am. J. Cardiol. 2009, 104, 1727–1731. [Google Scholar] [CrossRef]
- Lu, D.-Y.; Haileselassie, B.; Ventoulis, I.; Liu, H.-Y.; Liang, H.-Y.; Pozios, I.; Canepa, M.; Phillip, S.; Abraham, M.R.; Abraham, T. E/e′ ratio and outcome prediction in hypertrophic cardiomyopathy: The influence of outflow tract obstruction. Eur. Heart J. Cardiovasc. Imaging 2018, 19, 101–107. [Google Scholar] [CrossRef]
- Maron, M.S.; Finley, J.J.; Bos, J.M.; Hauser, T.H.; Manning, W.J.; Haas, T.S.; Lesser, J.R.; Udelson, J.E.; Ackerman, M.J.; Maron, B.J. Prevalence, clinical significance, and natural history of left ventricular apical aneurysms in hypertrophic cardiomyopathy. Circulation 2008, 118, 1541–1549. [Google Scholar] [CrossRef] [Green Version]
- Suzuki, J.; Shimamoto, R.; Nishikawa, J.; Yamazaki, T.; Tsuji, T.; Nakamura, F.; Shin, W.S.; Nakajima, T.; Toyo-Oka, T.; Ohotomo, K. Morphological onset and early diagnosis in apical hypertrophic cardiomyopathy: A long-term analysis with nuclear magnetic resonance imaging. J. Am. Coll. Cardiol. 1999, 33, 146–151. [Google Scholar] [CrossRef] [Green Version]
- Nijenkamp, L.L.A.M.; Bollen, I.A.E.; van Velzen, H.G.; Regan, J.A.; van Slegtenhorst, M.; Niessen, H.W.M.; Schinkel, A.F.L.; Krüger, M.; Poggesi, C.; Ho, C.Y. Sex differences at the time of myectomy in hypertrophic cardiomyopathy. Circ. Heart Fail. 2018, 11, e004133. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Y.; Wang, L.P.; Yang, Y.K.; Tian, T.; Yang, K.Q.; Sun, X.; Jiang, Y.; Liu, Y.X.; Zhou, X.L.; Li, J. Clinical profile and prognosis of left ventricular apical aneurysm in hypertrophic cardiomyopathy. Am. J. Med. Sci. 2016, 351, 101–110. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.P.; Park, K.; Kim, H.K.; Kim, Y.J.; Sohn, D.W. Apically displaced papillary muscles mimicking apical hypertrophic cardiomyopathy. Eur. Heart J. Cardiovasc. Imaging 2013, 14, 128–134. [Google Scholar] [CrossRef] [PubMed]
- To, A.C.Y.; Dhillon, A.; Desai, M.Y. Cardiac magnetic resonance in hypertrophic cardiomyopathy. JACC Cardiovasc. Imaging 2011, 4, 1123–1137. [Google Scholar] [CrossRef] [Green Version]
- Ichida, M.; Nishimura, Y.; Kario, K. Clinical significance of left ventricular apical aneurysms in hypertrophic cardiomyopathy patients: The role of diagnostic electrocardiography. J. Cardiol. 2014, 64, 265–272. [Google Scholar] [CrossRef] [Green Version]
- Serri, K.; Reant, P.; Lafitte, M.; Berhouet, M.; Le Bouffos, V.; Roudaut, R.; Lafitte, S. Global and regional myocardial function quantification by two-dimensional strain: Application in hypertrophic cardiomyopathy. J. Am. Coll. Cardiol. 2006, 47, 1175–1181. [Google Scholar] [CrossRef] [Green Version]
- Kansal, M.M.; Lester, S.J.; Surapaneni, P.; Sengupta, P.P.; Appleton, C.P.; Ommen, S.R.; Ressler, S.W.; Hurst, R.T. Usefulness of two-dimensional and speckle tracking echocardiography in “gray zone” left ventricular hypertrophy to differentiate professional football player’s heart from hypertrophic cardiomyopathy. Am. J. Cardiol. 2011, 108, 1322–1326. [Google Scholar] [CrossRef]
- Collier, P.; Phelan, D.; Klein, A. A test in context: Myocardial strain measured by speckle-tracking echocardiography. J. Am. Coll. Cardiol. 2017, 69, 1043–1056. [Google Scholar] [CrossRef]
- Yang, H.; Carasso, S.; Woo, A.; Jamorski, M.; Nikonova, A.; Wigle, E.D.; Rakowski, H. Hypertrophy pattern and regional myocardial mechanics are related in septal and apical hypertrophic cardiomyopathy. J. Am. Soc. Echocardiogr. 2010, 23, 1081–1089. [Google Scholar] [CrossRef]
- Urbano-Moral, J.A.; Rowin, E.J.; Maron, M.S.; Crean, A.; Pandian, N.G. Investigation of global and regional myocardial mechanics with 3-dimensional speckle tracking echocardiography and relations to hypertrophy and fibrosis in hypertrophic cardiomyopathy. Circ. Cardiovasc. Imaging 2014, 7, 11–19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paraskevaidis, I.A.; Farmakis, D.; Papadopoulos, C.; Ikonomidis, I.; Parissis, J.; Rigopoulos, A.; Iliodromitis, E.K.; Kremastinos, D.T. Two-dimensional strain analysis in patients with hypertrophic cardiomyopathy and normal systolic function: A 12-month follow-up study. Am. Heart J. 2009, 158, 444–450. [Google Scholar] [CrossRef] [PubMed]
- Tower-Rader, A.; Mohananey, D.; To, A.; Lever, H.M.; Popovic, Z.B.; Desai, M.Y. Prognostic value of global longitudinal strain in hypertrophic cardiomyopathy: A systematic review of existing literature. JACC Cardiovasc. Imaging 2019, 12, 1930–1942. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Pozios, I.; Haileselassie, B.; Nowbar, A.; Sorensen, L.L.; Phillip, S.; Lu, D.-Y.; Ventoulis, I.; Luo, H.; Abraham, M.R. Role of global longitudinal strain in predicting outcomes in hypertrophic cardiomyopathy. Am. J. Cardiol. 2017, 120, 670–675. [Google Scholar] [CrossRef]
- Weng, Z.; Yao, J.; Chan, R.H.; He, J.; Yang, X.; Zhou, Y.; He, Y. Prognostic value of LGE-CMR in HCM: A meta-analysis. JACC Cardiovasc. Imaging 2016, 9, 1392–1402. [Google Scholar] [CrossRef]
- Schnell, F.; Donal, E.; Bernard-Brunet, A.; Reynaud, A.; Wilson, M.G.; Thebault, C.; Ridard, C.; Mabo, P.; Carré, F. Strain analysis during exercise in patients with left ventricular hypertrophy: Impact of etiology. J. Am. Soc. Echocardiogr. 2013, 26, 1163–1169. [Google Scholar] [CrossRef]
- Popović, Z.B.; Kwon, D.H.; Mishra, M.; Buakhamsri, A.; Greenberg, N.L.; Thamilarasan, M.; Flamm, S.D.; Thomas, J.D.; Lever, H.M.; Desai, M.Y. Association between regional ventricular function and myocardial fibrosis in hypertrophic cardiomyopathy assessed by speckle tracking echocardiography and delayed hyperenhancement magnetic resonance imaging. J. Am. Soc. Echocardiogr. 2008, 21, 1299–1305. [Google Scholar] [CrossRef]
- Rowin, E.J.; Maron, B.J.; Olivotto, I.; Maron, M.S. Role of exercise testing in hypertrophic cardiomyopathy. JACC Cardiovasc. Imaging 2017, 10, 1374–1386. [Google Scholar] [CrossRef]
- Desai, M.Y.; Bhonsale, A.; Patel, P.; Naji, P.; Smedira, N.G.; Thamilarasan, M.; Lytle, B.W.; Lever, H.M. Exercise echocardiography in asymptomatic HCM: Exercise capacity and not LV outflow tract gradient predicts long-term outcomes. JACC Cardiovasc. Imaging 2014, 7, 26–36. [Google Scholar] [CrossRef] [Green Version]
- Coats, C.J.; Rantell, K.; Bartnik, A.; Patel, A.; Mist, B.; McKenna, W.J.; Elliott, P.M. Cardiopulmonary exercise testing and prognosis in hypertrophic cardiomyopathy. Circ. Heart Fail. 2015, 8, 1022–1031. [Google Scholar] [CrossRef]
- Finocchiaro, G.; Haddad, F.; Knowles, J.W.; Caleshu, C.; Pavlovic, A.; Homburger, J.; Shmargad, Y.; Sinagra, G.; Magavern, E.; Wong, M. Cardiopulmonary responses and prognosis in hypertrophic cardiomyopathy: A potential role for comprehensive noninvasive hemodynamic assessment. JACC Heart Fail. 2015, 3, 408–418. [Google Scholar] [CrossRef] [PubMed]
- Sorajja, P.; Allison, T.; Hayes, C.; Nishimura, R.A.; Lam, C.S.P.; Ommen, S.R. Prognostic utility of metabolic exercise testing in minimally symptomatic patients with obstructive hypertrophic cardiomyopathy. Am. J. Cardiol. 2012, 109, 1494–1498. [Google Scholar] [CrossRef] [PubMed]
- Masri, A.; Pierson, L.M.; Smedira, N.G.; Agarwal, S.; Lytle, B.W.; Naji, P.; Thamilarasan, M.; Lever, H.M.; Cho, L.S.; Desai, M.Y. Predictors of long-term outcomes in patients with hypertrophic cardiomyopathy undergoing cardiopulmonary stress testing and echocardiography. Am. Heart J. 2015, 169, 684–692. [Google Scholar] [CrossRef] [PubMed]
- Magrì, D.; Re, F.; Limongelli, G.; Agostoni, P.; Zachara, E.; Correale, M.; Mastromarino, V.; Santolamazza, C.; Casenghi, M.; Pacileo, G. Heart failure progression in hypertrophic cardiomyopathy—Possible insights from cardiopulmonary exercise testing. Circ. J. 2016, 80, 2204–2211. [Google Scholar] [CrossRef] [Green Version]
- Magrì, D.; Limongelli, G.; Re, F.; Agostoni, P.; Zachara, E.; Correale, M.; Mastromarino, V.; Santolamazza, C.; Casenghi, M.; Pacileo, G. Cardiopulmonary exercise test and sudden cardiac death risk in hypertrophic cardiomyopathy. Heart 2016, 102, 602–609. [Google Scholar] [CrossRef]
- Maron, B.J.; Ommen, S.R.; Semsarian, C.; Spirito, P.; Olivotto, I.; Maron, M.S. Hypertrophic cardiomyopathy: Present and future, with translation into contemporary cardiovascular medicine. J. Am. Coll. Cardiol. 2014, 64, 83–99. [Google Scholar] [CrossRef] [Green Version]
- Raphael, C.E.; Cooper, R.; Parker, K.H.; Collinson, J.; Vassiliou, V.; Pennell, D.J.; de Silva, R.; Hsu, L.Y.; Greve, A.M.; Nijjer, S. Mechanisms of myocardial ischaemia in hypertrophic cardiomyopathy: Insights from wave intensity analysis and magnetic resonance. J. Am. Coll. Cardiol. 2016, 68, 1651–1660. [Google Scholar] [CrossRef] [Green Version]
- Yanagiuchi, T.; Tada, N.; Haga, Y.; Suzuki, S.; Sakurai, M.; Taguri, M.; Ootomo, T. Utility of preprocedural multidetector computed tomography in alcohol septal ablation for hypertrophic obstructive cardiomyopathy. Cardiovasc. Interv. Ther. 2019, 34, 364–372. [Google Scholar] [CrossRef]
- Olivotto, I.; Cecchi, F.; Gistri, R.; Lorenzoni, R.; Chiriatti, G.; Girolami, F.; Torricelli, F.; Camici, P.G. Relevance of coronary microvascular flow impairment to long-term remodelling and systolic dysfunction in hypertrophic cardiomyopathy. J. Am. Coll. Cardiol. 2006, 47, 1043–1048. [Google Scholar] [CrossRef] [Green Version]
- Freitas, P.; Ferreira, A.M.; Arteaga-Fernández, E.; de Oliveira Antunes, M.; Mesquita, J.; Abecasis, J.; Marques, H.; Saraiva, C.; Matos, D.N.; Rodrigues, R.; et al. The amount of late gadolinium enhancement outperforms current guideline-recommended criteria in the identification of patients with hypertrophic cardiomyopathy at risk of sudden cardiac death. J. Cardiovasc. Magn. R. 2019, 21, 50. [Google Scholar] [CrossRef] [Green Version]
- Conte, M.R.; Bongioanni, S.; Chiribiri, A.; Leuzzi, S.; Lardone, E.; Di Donna, P.; Pizzuti, A.; Luceri, S.; Cesarani, F.; Mabritto, B. Late gadolinium enhancement on cardiac magnetic resonance and phenotypic expression in hypertrophic cardiomyopathy. Am. Heart J. 2011, 161, 1073–1077. [Google Scholar] [CrossRef] [PubMed]
- Bruder, O.; Wagner, A.; Jensen, C.J.; Schneider, S.; Ong, P.; Kispert, E.M.; Nassenstein, K.; Schlosser, T.; Sabin, G.V.; Sechtem, U. Myocardial scar visualized by cardiovascular magnetic resonance imaging predicts major adverse events in patients with hypertrophic cardiomyopathy. J. Am. Coll. Cardiol. 2010, 56, 875–887. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Green, J.J.; Berger, J.S.; Kramer, C.M.; Salerno, M. Prognostic value of late gadolinium enhancement in clinical outcomes for hypertrophic cardiomyopathy. JACC Cardiovasc. Imaging 2012, 5, 370–377. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mentias, A.; Raeisi-Giglou, P.; Smedira, N.G.; Feng, K.; Sato, K.; Wazni, O.; Kanj, M.; Flamm, S.D.; Thamilarasan, M.; Popovic, Z.B. Late gadolinium enhancement in patients with hypertrophic cardiomyopathy and preserved systolic function. J. Am. Coll. Cardiol. 2018, 72, 857–870. [Google Scholar] [CrossRef]
- Avanesov, M.; Münch, J.; Weinrich, J.; Well, L.; Säring, D.; Stehning, C.; Tahir, E.; Bohnen, S.; Radunski, U.K.; Muellerleile, K. Prediction of the estimated 5-year risk of sudden cardiac death and syncope or non-sustained ventricular tachycardia in patients with hypertrophic cardiomyopathy using late gadolinium enhancement and extracellular volume CMR. Eur. Radiol. 2017, 27, 5136–5145. [Google Scholar] [CrossRef]
- Sado, D.M.; White, S.K.; Piechnik, S.K.; Banypersad, S.M.; Treibel, T.; Captur, G.; Fontana, M.; Maestrini, V.; Flett, A.S.; Robson, M.D. Identification and assessment of Anderson-Fabry disease by cardiovascular magnetic resonance noncontrast myocardial T1 mapping. Circ. Cardiovasc. Imaging 2013, 6, 392–398. [Google Scholar] [CrossRef] [Green Version]
- Hinojar, R.; Varma, N.; Child, N.; Goodman, B.; Jabbour, A.; Yu, C.-Y.; Gebker, R.; Doltra, A.; Kelle, S.; Khan, S. T1 mapping in discrimination of hypertrophic phenotypes: Hypertensive heart disease and hypertrophic cardiomyopathy: Findings from the International T1 Multicenter Cardiovascular Magnetic Resonance Study. Circ. Cardiovasc. Imaging 2015, 8, e003285. [Google Scholar] [CrossRef] [Green Version]
- Gastl, M.; Gotschy, A.; von Spiczak, J.; Polacin, M.; Bönner, F.; Gruner, C.; Kelm, M.; Ruschitzka, F.; Alkadhi, H.; Kozerke, S. Cardiovascular magnetic resonance T2* mapping for structural alterations in hypertrophic cardiomyopathy. Eur. J. Radiol. Open 2019, 6, 78–84. [Google Scholar] [CrossRef] [Green Version]
- Gastl, M.; Gruner, C.; Labucay, K.; Gotschy, A.; Von Spiczak, J.; Polacin, M.; Boenner, F.; Kelm, M.; Ruschitzka, F.; Alkadhi, H. Cardiovascular magnetic resonance T2* mapping for the assessment of cardiovascular events in hypertrophic cardiomyopathy. Open Heart 2020, 7, e001152. [Google Scholar] [CrossRef] [Green Version]



| Multimodality Imaging | Indications | Therapeutic Implications |
|---|---|---|
| Echocardiography |
|
|
| Cardiac magnetic resonance |
|
|
| Computed tomography angiography |
|
|
| Cardiac nuclear imaging |
|
|
| Cardiopulmonary exercise testing |
|
|
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Anghel, L.; Stătescu, C.; Șerban, I.-L.; Mărănducă, M.A.; Butcovan, D.; Clement, A.; Bostan, M.; Sascău, R. The Advantages of New Multimodality Imaging in Choosing the Optimal Management Strategy for Patients with Hypertrophic Cardiomyopathy. Diagnostics 2020, 10, 719. https://doi.org/10.3390/diagnostics10090719
Anghel L, Stătescu C, Șerban I-L, Mărănducă MA, Butcovan D, Clement A, Bostan M, Sascău R. The Advantages of New Multimodality Imaging in Choosing the Optimal Management Strategy for Patients with Hypertrophic Cardiomyopathy. Diagnostics. 2020; 10(9):719. https://doi.org/10.3390/diagnostics10090719
Chicago/Turabian StyleAnghel, Larisa, Cristian Stătescu, Ionela-Lăcrămioara Șerban, Minela Aida Mărănducă, Doina Butcovan, Alexandra Clement, Mădălina Bostan, and Radu Sascău. 2020. "The Advantages of New Multimodality Imaging in Choosing the Optimal Management Strategy for Patients with Hypertrophic Cardiomyopathy" Diagnostics 10, no. 9: 719. https://doi.org/10.3390/diagnostics10090719