1. Introduction
The majority of pathological skin conditions are treated with topical formulations delivering therapeutically effective concentration of drugs in skin layers and exert a local effect. By contrast, many potent drugs display scarce ability to penetrate the skin, in particular the
stratum corneum, which represents the main obstacle that limit their absorption after topical application and hence inherent potency. Particularly, many skin inflammatory diseases are characterized by leucocyte invasion leading to a proliferation and abnormal differentiation of keratinocytes with a subsequent increase in skin thickness and alterations of skin barrier properties [
1]. Nano-delivery systems can represent proper carriers for skin delivery of suitable therapeutic drug concentrations within the deeper skin layers and provide a sustained and/or controlled release [
2]. Phospholipid-based nanovesicles are particularly suitable for topical formulations because of their high biocompatibility with skin lipids and negligible toxicity [
3]. Conversely, conventional liposomes composed of pure or mixtures of phospholipid(s) and cholesterol generally accumulate in the
stratum corneum and in the skin appendages, with negligible permeation through deeper skin layers, because of their low flexibility, as reported by most of the literature [
4,
5,
6].
Some molecules can impart deformability or elasticity to the bilayer membrane of nanosized liposomes, resulting in markedly improved drug permeability through the skin by several orders of magnitude [
7,
8,
9]. Besides yielding a deeper penetration through skin, nanovesicles can effectively protect the drug against the environment, retain the drug in the target tissue, reduce systemic absorption and minimize side effects [
10].
The principal aim of the present work was to design and develop novel nanovesicles for topical delivery loaded with escin (ESN,
Figure 1a), a natural bioactive saponin, and berberine chloride (BRB,
Figure 1b), a quaternary isoquinoline alkaloid.
Natural products represent attractive molecules in drug discovery for their broad structure variability and also for their capability to interact with multiple targets, representing a more versatile approach to successful therapies [
11,
12,
13]. Saponins are natural non-ionic surfactants with useful pharmacological and biological properties, mainly distributed in plants, lower marine animals, and some bacteria. Saponins contain an aglycone with a steroid (C27) structure or a triterpene (C30) moiety, represented by a four-ringed steroid nucleus or a five-ringed structure. The amphiphilic properties of saponins are due to sugar moieties attached with one (monodesmosidic saponins, usually glycosylated at C-3 position) or two (bidesmosidic) hydroxyl or carboxyl moieties. When dissolved in water, saponins produce foam, which is related to their name from the Latin word sapo [
14].
ESN is the major active saponin isolated from the seed of
Aesculus hippocastanum. ESN is a triterpenoid glycoside with three sugar units linked at C-3 of the aglycone moiety, and consisted of a mixture of α-escin and β-escin. ESN is clinically used to increase venous wall tone and to achieve antiedematous and anti-inflammatory effects, accounting for its efficacy in the treatment of chronic venous insufficiency, hemorrhoids, and post-operative oedema [
15]. It has been shown that, after application on dorsal and ventral skin in mice and rats, 25% and 50%, respectively, of the topical dose was absorbed by the skin. Following topical administration in pigs, high ESN concentrations were found under the site of application, even in deeper muscle structures [
15].
Previously, a study using 1,2-dimyristoyl-sn-glycero-phosphocholine (DMPC, 15 mg/mL) vesicles evaluated the effects of ESN addition. Vesicles were stable below 1 mol % of ESN. Between 1 and 6–7 mol % of ESN, the formation of vesicles was also observed, but large aggregates that precipitate over time occurred. Micelle-sized structures were formed at ESN contents above 6–7 mol % [
16].
In a further study, the interaction of ESN with cholesterol and natural dipalmitoylphosphatidylcholine monolayers was investigated using Langmuir isotherms [
17]. The monolayer was obtained by DPPC and cholesterol or a mixture of them. Intercalation of ESN in a monolayer made of pure cholesterol was low, whereas in a pure DPPC monolayer, no intercalation of ESN was detectable. By contrast, in aqueous pseudo-ternary systems (ESN, dipalmitoylphosphatidylcholine, cholesterol) and in pseudo-binary systems (ESN, cholesterol), colloidal microstructures built up from ring-like and worm-like subunits were observed [
17].
BRB is a natural quaternary isoquinoline alkaloid isolated from several medicinal plants of the genera
Berberis,
Hydrastis,
Coptis,
Coscinium, and
Mahonia, which are traditionally used for various skin conditions. BRB is a representative natural constituent having a variety of biological effects through different mechanisms of actions [
18]. Despite the evidenced potentiality of BRB in the treatment of skin diseases, its topical application is limited due to its high hydrophilicity, the aqueous solubility of 1–2 mg/mL at 25 °C and the approximate log
p value of −1.5 hinder its delivery across the skin layers [
19]. Recently, to increase its dermal bioavailability, BRB was formulated with sodium oleate as complexing agent, because of its low toxicity and skin penetrating characteristics. This complex displayed about 250-fold higher saturation solubility in
n-octanol, endorsing the improved lipid solubility of the complex compared with free drug [
20].
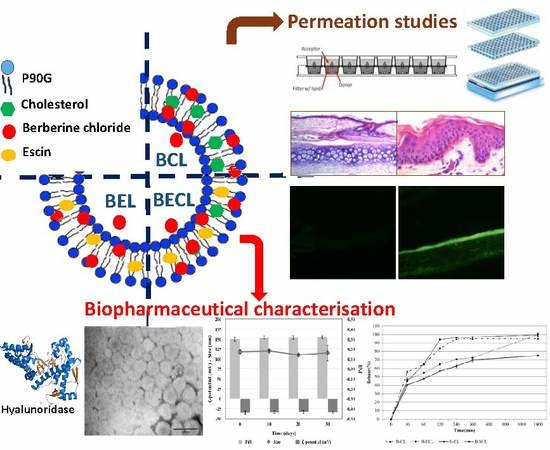
The present study was designed to explore the conversion of the biologically active amphiphilic saponin ESN, into a vesicle bilayer-forming component. In order to assess that ESN potential activity remained after the formulation in the vesicles, the hyaluronidase inhibition activity of these escinosomes was evaluated. Nanovesicle deformability after vesicle loading with BRB was also examined, in order to evaluate their passage through the skin and BRB transport in the different skin layers. A further aim of the present work was to investigate the anatomical similarities of rabbit ear skin with human abdominal skin with respect to the stratum corneum and epidermal thickness as well as the hair follicular density, in order to evaluate permeation properties of the different formulations using vertical diffusion Franz cells.
2. Materials and Methods
2.1. Materials
Phospolipon 90G (P90G) was purchased from Lipoid AG (Cologne, Germany) with the support of its Italian agent AVG srl. Cholesterol (CHOL), ESN, BRB and hydroxypropyl methylcellulose (HPMC) were provided by Sigma-Aldrich (Milan, Italy). Methanol (MeOH), methanol HPLC grade, acetonitrile (ACN), formic acid, dichloromethane (CH2Cl2), dimethylsulfoxide (DMSO) and formaldehyde solution, phosphate saline buffer (PBS), acetate buffer, NaOH, potassium borate, hyaluronidase from bovine testes Type IV-S, powder (mouse embryo tested, 750–3000 units/mg solid), compound 48/80 (condensation product of N-methyl-p-methoxyphenethylamine with formaldehyde, hyaluronic acid potassium salt from human umbilical cord, p-dimethylaminobenzaldehyde (98%, Ehrlich′s reagent) were purchased from Sigma-Aldrich (Milan, Italy). Piroxicam, progesteron, Prisma Buffer (P/N 110151), Hydration Solution (P/N: 120706) and Skin-PAMPATM system were purchased from pION Inc. (Billerica, MA, USA). Ultrapure water was produced by a synergy UV Simplicity water purification system provided by Merck KGaA (Molsheim, France). Phosphotungstic acid (PTA) was purchased from Electron Microscopy Sciences (Hatfield, PA, USA).
2.2. HPLC-DAD Analytical Method
Quantitative determination of active constituents was carried out by the 1200 High Performance Liquid Chromatograph (HPLC) equipped with a Diode Array Detector (DAD) from Agilent Technologies Italia Spa (Rome, Italy). DAD was set up at the two wavelengths of 210 nm for ESN and 346 nm for BRB. Chromatographic analysis were performed using a reverse-phase column Luna-C18, 250 mm × 4.6 mm, 5 µm particle size, maintained at 27 °C. A gradient elution method with 1 mL/min flow rate for 32 min was applied, using (A) acetonitrile and (B) water at pH 3.2 (by formic acid) like mobile phases. Acetonitrile was selected because of its low UV cut off, which avoids interference with the ESN signal. The analytical method was: 0–3 min 85% (B), 3–9 min 85%–70% (B), 9–10 min 70% (B), 10–17 min 70%–50% (B), 17–19 min 50% (B), 19–26 min 50%–45% (B), 26–30 min 45%–40% (B), 30–35 min 40%–1% (B), 35–40 min 1%, 40–47 min 1%–85% (B).
R2 was calculated both for BRB and ESN and resulted respectively 0.99925 and 0.99979. Limit of detection (LOD) and limit of quantification (LOQ) were calculated both for BRB and ESN by determination of signal-to-noise ratio, in accordance to the ICH guidelines. LOD was 0.60 ng for BRB and 400.00 ng for ESN, while LOQ was 1.51 ng for BRB and 988.00 ng for ESN.
2.3. Development and Optimisation of Nanovesicles
Nanovesicles were prepared using the thin layer evaporation method at specific conditions [
21,
22]. Different liposomes were developed by varying the lipid constituents and loading BRB. In particular, 330 mg of P90G, 100 mg of CHOL and 50 mg of ESN were used as lipophilic components and they were dissolved in CH
2Cl
2/MeOH, while 13 mg of BRB were solubilized in water (10 mL). The organic solvent was removed by rotary evaporator for 20 min and the dried lipid film was then hydrated with the aqueous phase (with or without BRB) for 30 min at 35 °C [
23]. First, conventional liposomes with P90G and CHOL were prepared; then, the same liposomes were prepared by adding ESN; finally, in the third formulation, P90G plus ESN were used to prepare the vesicles. The same three types of vesicles, loaded with BRB, were prepared in parallel. Finally, the Sonopuls Ultrasonic Homogenizer HD 2200 by Bandelin electronic GmbH & Co. KG (Berlin, German), was used in order to reduce vesicle size and improve sample homogeneity.
2.4. Physical Characterization of Nanovesicles
Nanovesicle characterization during the development and the optimization steps was made by measuring size, homogeneity and possible aggregation state by Dynamic and Electrophoretic Light Scattering (DLS and ELS, Zetasizer Nanoseries ZS90) by Malvern instrument (Worcestershire, UK), with a scattering angle of 90° at 25 °C [
24,
25]. Average Hydrodynamic Diameter (AHD, nm), size distribution expressed as Polydispersity Index (PdI, dimensionless measurement) and ζ-Potential (mV), were obtained using the software provided by Malvern. Scattering was measured on samples diluted 50/100-fold in ultrapure water and every measurement was performed in triplicate. Nanovesicle morphological characterization was performed by transmission electron microscope (CM12 TEM, PHILIPS, The Netherlands) equipped with an OLYMPUS Megaview G2 camera with an accelerating voltage of 80 kV. TEM allowed to visualize vesicle dispersion and dimensions. A drop of the diluted sample was applied and dried by desiccation on a carbon film copper grid. This was then counterstained with 1% (
w/v) of phosphotungstic acid solution and examined at different magnifications [
26]. The deformability of vesicles was measured by extrusion [
27]. It was performed by 21 passages through polycarbonate extrusion membranes with 50 nm cut-off, using the LiposoFast-Basic extruder by Avestin Europe GmbH (Mannheim, Germany) joined to a 7 atm pressure source. Before the extrusion, each formulation was properly diluted in water. Deformability was expressed as the ratio among vesicles diameter before and after extrusion (Equation (1)). Values around the unit are index of good deformability.
2.5. Technological Characterization of Nanovesicles
In order to characterize the liposomal dispersions, the encapsulation efficiency (EE) and the total recovery (R) were calculated for each formulation. EE is defined as the percentage of entrapped drug in relation to the weighed drug (Equation (2)):
In order to determine the amount of entrapped drug, vesicles were purified from free BRB and free ESN, by dialysis bag method [
28,
29], using Spectra/Por
® regenerated cellulose membranes with 3.5 KDa molecular weight cut-off (MWCO), by Repligen Europe B.V. (Breda, The Netherlands). The dialysis bag was stirred in ultrapure water (1 L), at room temperature for 1 h. After the purification, the samples were diluted in methanol, in order to dissolve and break the vesicles and release the encapsulated substances. Finally, a centrifugation at 14000 rpm for 10 min was applied and the amounts of BRB and ESN were determined by HPLC-DAD. Rather, R is defined as the percentage of total drug recovered after the preparation procedure in relation to the weighed drug (Equation (3)):
and it was measured using the same procedure without the purification step by dialysis. Moreover, the pH-meter (Basic 20+) by Crison Instrument (Barcelona, Spain) was used to measure the pH of each formulation.
2.6. Stability Studies
The stability studies were carried out storing the samples for 1 month at 4 °C in the dark [
30]. Every ten days, physical (size, PdI, ζ-potential) and chemical (EE% and R%) parameters of the vesicles were investigated by DLS/ELS and HPLC-DAD.
2.7. Release of Active Constituents from the Vesicles
The dialysis bag method, with Spectra/Por
® regenerated cellulose membranes of 3.5 KDa MWCO by Repligen Europe B.V. (Breda, The Netherlands), was applied to study the release kinetic of ESN and BRB from liposomes [
30,
31] and from aqueous solution (BRB aqueous solution, B-SOL) or dispersion (ESN water dispersion, E-W), at the same concentrations used in liposomes, 1.3 mg/mL and 5 mg/mL respectively. 250 mL of PBS (pH 7.4) was used as release medium and the experiment was carried out in sink conditions at 37 °C under magnetic stirring, until 24 h. Therefore, 0.5 mL withdrawals were done at specified time points (30, 60, 120, 240, 360, and 1440) min and replaced by equal volumes of fresh buffer. Finally, all samples were centrifuged at 14,000 rpm for 10 min and analyzed by HPLC-DAD.
2.8. Hyaluronidase Inhibition Assay
The hyaluronidase inhibition activity was investigated using a colorimetric assay reported by Murata and coworkers [
32]. Samples were dissolved in 0.1 M acetate buffer (pH 4.0, 0.2 mL) and were mixed with 0.1 mL hyaluronidase (400 unit/mL buffer) and incubated for 20 min at 37 °C. Next, compound 48/80 in buffer (0.3 mg/mL, 0.2 mL) was added as activator and allowed to react for 20 min at 37 °C. Then, hyaluronic acid potassium salt in buffer (0.4 mg/mL, 0.5 mL) was added and the mixture was incubated for 40 min at 37 °C. NaOH (0.4 M, 0.2 mL) was added to the mixture and cooling with ice stopping the reaction. Then, potassium borate solution (0.4 M, 0.2 mL) was added, vortexed and the mixture boiled for three minutes. The mixture was cooled using ice and 6 mL of a solution of p-dimethylaminobenzaldehyde (1%
w/v in acetate buffer) was then added and the sample was placed for 20 min at 37 °C. The hyaluronidase inhibitory activities (HIA%) were measured at 600 nm, mean ± SD (
n = 3), and calculated as follows:
where control was acetate buffer and blank was the hyaluronidase enzyme in acetate buffer.
2.9. Skin-PAMPA™: In Vitro Simulation of Stratum Corneum Permeation by Vesiscles
The Skin-PAMPA
TM model from pION was employed as in vitro permeation assay, in order to evaluate and compare the permeability of the three formulations with BRB and predict BRB skin absorption [
33]. B-SOL, was used as reference of free-BRB permeability. The skin-PAMPA membranes were used after an overnight hydration by the Hydration Solution, until all wells turned into translucent. After that, the wells in the bottom plate (donor) were filled with 200 µL of samples, while the wells in skin-PAMPA
TM top plate (P/N: 120656, pION) (acceptor) were filled with 200 µL of fresh acceptor solution, Prisma Buffer, at pH 7.4. A lid was used to cover the top plate, once the sandwich was assembled and a Parafilm layer was applied around the perimeter to seal the two compartments. Then, the 96-well STIRWELL
TM PAMPA sandwiches (P/N: 110243, pION) were incubated into a chamber with a wet filter paper under the lid, to maintain a high relative humidity and minimize evaporation. The assay was carried out at room temperature (25 °C ± 2 °C) for 5 h, according to the protocol. After the permeation time had elapsed, samples from acceptor and donor plate were collected and analyzed by HPLC-DAD. The Effective Permeability (P
e) expressed as cm/s was calculated according to the following approximate equation [
34]:
where
A is the filter area [0.3 cm
2], multiplied by a nominal porosity of 70% according to the manufacturer,
VD is the donor volume [0.2 cm
3],
t is the incubation time,
CD(t) is the concentration [mol x cm
−3] of the compound in the donor phase at time
t,
CD(0) is the initial concentration [mol × cm
−3] of the compound in the donor phase at time 0, and
R is the membrane retention factor (Equation (5)):
and
ra is the sink asymmetry ratio (gradient-pH-induced), defined according to the following equation:
2.10. Histological Evaluation of Rabbit Ear Skin and Human Abdominal Skin
Cross-sections of rabbit ear skin were prepared at the Department of Experimental and Clinical Medicine, of the University of Florence, Florence, Italy. Human skin samples were kindly provided by operators from the Surgical Clinic, Careggi General Hospital, Florence, Italy, taken from surgical specimens removed for reductive abdominoplasty and intended for disposal. Both the rabbit and human skin samples were taken from discarded specimens intended for disposal, which exempted us from the need for a preliminary ethical permission. In the present study, the histological comparison between human abdominal skin and rabbit ear skin was investigated by conventional light microscopical analysis, in order to confirm the suitability of this animal model in the percutaneous studies [
35]. Whole-thickness rabbit skin tissue was peeled off the inner part of the ear, close to the acoustic meatus, since preliminary studies showed little or no permeation through the skin from the ear apex. In particular, skin layers were manually stripped from the underlying cartilage within a rectangular incision made with a sharp blade and cut into discs 2 cm in diameter, paying attention not to damage the skin surface. Skin integrity was verified by light microscopy.
2.11. Percutaneous Penetration Studies using Rabbit Ear Skin
The skin discs thus prepared were used for the permeation study by the Franz cell system [
36], in order to compare the permeation characteristics of the three formulations with BRB and BRB aqueous solution; all of them having the same BRB concentration (1.3 mg/mL). In order to avoid dehydration, the freshly cut skin was kept moisten between sheets of filter paper wet with PBS and the skin outer surface was gently dried by dabbing with filter paper, before placement on the vertical diffusion Franz cells (3.14 cm
2 diffusion area). The donor chamber was filled with 1 mL of sample and the acceptor chamber was filled with 7 mL of PBS under magnetic stirring. During the experiment, the apparatus was maintained at 37 °C by a thermostatic bath circulation. The skin was placed between the two compartments, with the external layer facing the donor chamber and with dermis touching the buffer solution in the acceptor chamber. A suitable O-ring seal was used between the donor chamber and the skin, in order to prevent leakage of the sample and its spreading out over the entire skin surface [
37]. Finally, the cells were clamped together and the donor chamber was sealed by Parafilm to avoid evaporation during the assay. The system was incubated for 6 h and 24 h. After 24 h, the acceptor solutions were analyzed by HPLC-DAD after 14,000 rpm centrifugation for 10 min, while the donor samples were first diluted with MeOH in order to allow vesicle break and fully dissolution of ESN/BRB. The amounts of BRB and ESN retained in the skin were also determined. Each skin lamina was washed 3 times with 3 mL PBS and dried with filter paper. The inner part of the skin specimen, in contact with the sample, was cut and divided into equal pieces. These were soaked in 1 mL of methanol, exposed to 3 h of ultrasonication bath and then shaken in a water bath for 3 h, in order to extract all the accumulated drugs [
38]. Finally, the samples were centrifuged 10 min at 14,000 rpm and analyzed by the liquid chromatograph. The permeation parameters were calculated as following: absorbed dose (A
24), expressed as percentage of the applied dose absorbed through the skin and that recovered in the receptor compartment; absorbable dose retained inside the skin (S
24), expressed as percentage of the applied dose recovered inside the skin; total absorbed dose (TA
24), expressed as sum of the two percentages A
24 and S
24.
2.12. Histological Studies of Rabbit Ear Skin after Percutaneous Penetration Studies
After the permeation experiments, 6 h and 24 h respectively, fragments of cutaneous tissue were resected from the central part of each skin disc exposed to the different BRB samples, fixed in cold 4% formaldehyde in 0.1 M PBS, pH 7.4, at 4 °C for 4 h, cryoprotected by 5 min incubation in cold saccharose 10% in PBS, washed in PBS, embedded in KillikTM medium by Bio-Optica (Milan, Italy), quickly frozen by immersion in isopenthane and stored at −80 °C until needed. Sections, 7 µm thick, were cut with a Reichert/Leica 2800 Frigocut cryostat (Wetzlar, Germany). Part of specimens were stained with hematoxylin and eosin (HE) for conventional light microscopical analysis, others were observed directly under a Zeiss Axioskop fluorescence microscope (Oberkochen, Germany) equipped with a λ 350 filter, close to the absorption peak of BRB, which emits in the yellow-green region of the visible spectrum (λ 550). The fluorescence of BRB was assumed as an index of drug penetration into different skin tissues.
4. Discussion
Nanoparticle formulations represent a smart approach to increase stability and/or solubility and as a consequence bioavailability of natural products [
23,
26,
29,
42,
43,
44] but also to enhance permeation and crossing biological barriers including the blood–brain barrier [
45,
46,
47].
Particularly, nanovesicles have great ability to modulate drug penetration through the skin and allow sustained and controlled release of the encapsulated drugs. Their composition, size and charge strongly affect their interaction with the skin and penetrability: therefore, a direct evaluation of the skin penetration enhancement in comparison with conventional drug formulations is helpful for the optimization of efficient nanopharmaceuticals for dermatological purposes. Different in vitro approaches have been suggested to investigate the permeation of drugs loaded in nanovectors as alternative to human skin, principally skin from different animals and, more recently, smart simulation systems such as Skin-PAMPA™. These tests can provide a valuable alternative to human skin but in some cases, due to obvious anatomic and physiological differences, they show substantial differences in trans-cutaneous absorption as compared with human skin.
In this study, BRB, a natural quaternary ammonium benzylisoquinoline alkaloid, was chosen as the active drug to be loaded in the nanovesicles, due to the numerous biological activities against diverse skin diseases. This alkaloid is hydrophilic in nature (log P −1.5), and its water solubility is pH- and temperature-dependent. A solution of about 2 mg/mL of BRB was reported to be stable at 25 °C [
48].
In this study, three different nanovesicles (CL, ECL, and escinosomes EL), based on P90G, CHOL, and ESN, were developed and optimized. In particular, ESN, a natural mixtures of structurally correlated pentacyclic triterpene saponins [
49], largely employed as a vasoprotective anti-inflammatory, anti-edematous and antinociceptive agent, was used at a dose of 5 mg/mL to formulate ECL and EL nanovesicles.
BRB was loaded in the developed nanovesicles and the physical and chemical properties were investigated in terms of AHD, PdI, ζ-potential, deformability, R% and EE%, stability, and release kinetics. The results demonstrated that B-EL possesses the best characteristics for skin application, particularly optimal PdI (0.17) and deformability, high-negative ζ-potential value, great EE (ca. 67%), high physical and chemical stability and the best BRB release properties (ca. 75% after 24 h). At the end of the release study, only 16%–18% of ESN was found in the release medium, indicating that ESN was strongly retained in the vesicles and suggesting that ESN could work as a bilayer-forming material. ESN hyaluronidase inhibition activity was unaffected by the formulation and the presence of BRB. Thus, ESN anti-inflammatory, venotonic and anti-oedematous potential activities were preserved, once it was formulated as vesicle component.
The Effective Permeability (Pe) of BRB in solution (B-SOL) or loaded in vesicles, namely B-CL, B-ECL, and B-EL was firstly evaluated using the Skin-PAMPA™, a smart, validated test for fast prediction of human skin penetration through an artificial membrane mimicking the human stratum corneum. Pe of B-SOL (1.12 × 10−6 cm/s) was very similar to that of progesterone (1.19 × 10−6 cm/s), used as reference standard drug of high permeability. Surprisingly, B-ECL displayed a 4-fold higher Pe value than that calculated for B-SOL, probably explained by the simultaneous presence of ESN and CHOL. B-CL and B-EL displayed similar Pe values, which were twice times the value of B-SOL. These results evidenced that ESN was able to replace CHOL not only structurally but also functionally.
The in vitro permeation studies were preceded by the histological comparison between rabbit ear skin and human abdominal skin. Both tissues showed comparable characteristics with respect to the
stratum corneum and epidermal thickness as well as hair follicular structure and density. The permeation of BRB with the different formulations was then evaluated by the vertical diffusion Franz cells, observing the distribution of BRB fluorescence and performing quantitative analysis. Despite the higher TA
24 values found for B-CL, it was found that the skin samples treated with B-EL displayed a comparable BRB absorption as compared with those treated with B-CL. B-EL and B-CL displayed similar composition, except for ESN replacing CHOL in B-EL. CHOL in the bilayer structure of liposomes influences the lipid dynamics because of its rigid ring structure, reducing gauche–trans isomerization and rotational and lateral diffusion of lipids, which results in an ordering effect on the liquid crystalline state with a final fluidizing effect in the gel state [
50]. Probably the rigid ring structure of ESN, which is very similar to that of sterols, could have a similar, significant effect on membrane dynamics, confirming that ESN was not simply encapsulated but it is included within the membrane bilayer of the vesicle, giving physical stability and allowing a certain deformability and permeability. It is noteworthy that these two nanovesicles shared major favourable characteristics for skin delivery purposes, i.e., high deformability, proper size, PdI, and ζ-potential. In addition, B-EL was superior to B-CL in terms recovery, encapsulation efficiency, and release properties.
Of note, the results of the permeation tests with rabbit ear skin and Skin-PAMPA™ were substantially different. The latter test principally simulated the permeation through the
stratum corneum, the main barrier of the epidermis owing to the presence of an abundant lipid matrix containing ceramides, CHOL and free fatty acids, constituents that are different from those of the lower epidermal layers. These characteristics can clarify the faster crossing properties of the epidermis shown by BRB loaded in liposomes when compared with aqueous BRB. By contrast, the test with rabbit ear skin indicated a different performance of the aqueous BRB, with improved permeation through the deepest epidermal layers,
annexa and dermis, characterized by less lipids and more aqueous tissues. The behavior of BRB in the Skin-PAMPA™ and in the test with rabbit ear skin showed striking differences with the results reported in the literature, which identify BRB having high hydrophilicity and low dermal permeability [
20]. Indeed, BRB has an amphiphilic structure, ascribable to the hydrophilic portion of the quaternary ammonium salt and to the lipophilic benzylisoquinoline moiety: these features can extremely influence its penetration through the
stratum corneum, as well as the underlying epidermal layers. Future studies should be focused on evaluating the concentration role of ESN, when combined with P90G, in the bilayer stability and on better investigating the cohesive interactions occurring between the sugar groups of ESN and the phospholipid headgroups, possibly driven by hydrogen bonds, in particular with the carbonyl and negatively charged phosphate groups of the phospholipid.