Minimally Invasive vs. Open Surgery for Hallux Valgus: A Meta-Analysis
- Department of Ankle and Foot Surgery, Beijing Tongren Hospital, Capital Medical University, Beijing, China
Purpose: In recent years, minimally invasive surgery (MIS) for hallux valgus has emerged and gained popularity. To date, evidence on the benefits of MIS for hallux valgus is still controversial. This updated meta-analysis aimed to comprehensively evaluate the efficiency of MIS vs. open surgery for hallux valgus.
Methods: A systematic literature search of PubMed, Embase, and the Cochrane Library was performed. Two independent reviewers conducted data extraction and analyzed data with R software. Data were presented with risk ratio (RR) and standardized mean difference (SMD) along with 95% confidence interval (CI).
Results: A total of 22 studies in which there were 790 ft treated with the MIS procedure and 838 ft treated with an open procedure were included. The correction of sesamoid position was better in the MIS group. The post-operative distal metatarsal articular angle (DMAA) of the MIS group was lower. There was less pain at the early phase in the MIS group. The MIS group had a shorter surgery time and shorter hospitalization time compared with the open group. Our meta-analysis revealed no statistically significant difference in hallux valgus angle (HVA), first intermetatarsal angle (IMA), the first metatarsal shortening, the American Orthopedic Foot and Ankle Society (AOFAS) score, visual analog scale (VAS) score at the final follow-up or complication rate (when all studies were considered). When taking into consideration only randomized controlled trial (RCT), the AOFAS score was higher in the MIS group while HVA, IMA, DMAA, and complication rate remained no significance. Post-operative IMA of the MIS group was significantly lower when only studies reporting the second-generation (2G) MIS were included. When just studies adopting the third-generation (3G) MIS were included, the HVA and DMAA were lower in the MIS group.
Conclusion: The MIS procedures were more effective than open surgeries in the treatment of hallux valgus. Moreover, the MIS group achieved better radiologic and clinical outcomes compared with the open group.
Introduction
Hallux valgus is a common forefoot disorder involving a lateral deviation of the hallux and medial deviation of the first metatarsal (1). Hallux valgus is often associated with first metatarsophalangeal joint osteoarthritis, and it has been linked to notable health problems, such as disability, a greater risk of falling, impaired balance, and lesser quality of daily life (2). Symptomatic hallux valgus is usually treated with surgeries such as chevron osteotomy, Lapidus procedure, and scarf osteotomy (3–7). There are over 150 open surgical procedures for hallux valgus, but none of them have been proven to be better than others. In recent years, minimally invasive surgery (MIS) has become popular for hallux valgus because of its shorter operation time, smaller scar, and shorter recovery time compared with open surgeries. So far, three generations of minimally invasive techniques have been developed. The first generation was the Reverdin–Isham technique (8), which used angular medial closed wedge osteotomy without osteosynthesis. The second generation (2G) was the Bösch osteotomy (9), which was a modification of Hohmann osteotomy. Temporary internal fixation with Kirschner wires were used after distal transverse osteotomy. The third generation (3G) was minimally invasive chevron and akin (MICA) (10), which used percutaneous osteotomies and was fixed with compression screws.
Recently, two meta-analyses (11, 12) have been carried out to determine the effects of MIS vs. open surgery, showing no significant difference in radiological outcomes and functional scores. However, relatively a few outcome measures (OMs) had been included in Singh's meta-analysis (11). Lu et al. conducted a meta-analysis in which most of the included studies were of low or moderate quality (12). In the last 3 years, several new studies (13–18) performed a comparison between MIS and open surgery for hallux valgus have reported. Therefore, we conducted this updated meta-analysis and included more OMs to comprehensively evaluate the efficacy of MIS vs. open surgery for hallux valgus.
Materials and Methods
This meta-analysis was conducted in accordance with the preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement (19) and the Cochrane Handbook guidelines (20).
Search Strategy
A systematic literature search of Pubmed, Embase, and the Cochrane Library was performed from January 1, 1980 to October 1, 2021, using the following item: (“Hallux Abductovalgus” OR “Hallux valgus” OR “Bunion”) AND (“Percutaneous” OR “Bosch” OR “minimally invasive surgery” OR “minimally invasive” OR “Bösch” OR “SERI” OR “simple, effective, rapid, inexpensive” OR “minimally invasive chevron-Akin” OR “percutaneous chevron-Akin”), without a language filter.
Inclusion and Exclusion Criteria
All studies included in this meta-analysis need to meet the following criteria: (1) comparative studies reporting comparisons of MIS vs. open surgery for hallux valgus; (2) patients with hallux valgus; (3) at least a 6-month follow-up; and (4) OMs including at least one of the following: hallux valgus angle (HVA), first intermetatarsal angle (IMA), the American Orthopedic Foot and Ankle Society (AOFAS) score, visual analog scale (VAS) score, operating time, and complications. The exclusion criteria were: (1) unpublished data; (2) case series, case reports, reviews, and proceedings of meetings; (3) biomechanical research; and (4) no available data describing OMs mentioned earlier.
Data Extraction and Quality Assessment
Duplicates were initially excluded using Endnote Version X9. Two investigators independently screened titles and abstracts of the remaining studies. Then, full texts of the remaining studies were reviewed for eligibility according to the inclusion and exclusion criteria. Two independent reviewers performed data extraction from the included studies. The following data were extracted: the time of publication, country, study design, sample size, patients' age, technique, the duration of follow-up, HVA, IMA, AOFAS, and complications. Two authors used the Cochrane Handbook for Systematic Reviews of Interventions 5.2.0. (20) to assess the methodological quality and risk of bias of randomized controlled trials (RCTs), while the methodological qualities and risk of bias of non-RCTs were evaluated by the methodological index for non-randomized studies (MINORS) (21). MINORS score > 14 was set as the level of inclusionw. Disagreements were resolved by a discussion to reach a consensus.
Statistical Analysis
The data analysis was performed with Review Manager (Version 5.3; The Cochrane Collaboration, Oxford, UK) and the statistical software R 4.0.3 with the meta package. For dichotomous data, the risk ratio (RR) along with 95% confidence intervals (CIs) was calculated. For continuous data, standardized mean difference (SMD) with 95% CIs was calculated. p < 0.05 indicated a statistical significance. I2-test was used to evaluate the heterogeneity between studies. When I2 > 50% and p < 0.10, the heterogeneity was significant, and a random effect model was used. Otherwise, a fixed-effects model was applied in the meta-analysis. Subgroup meta-analysis was conducted according to study design (RCT or non-RCT) and technique (2G or 3G MIS). The publication bias was assessed by the Egger' test.
Results
Characteristics of the Included Studies
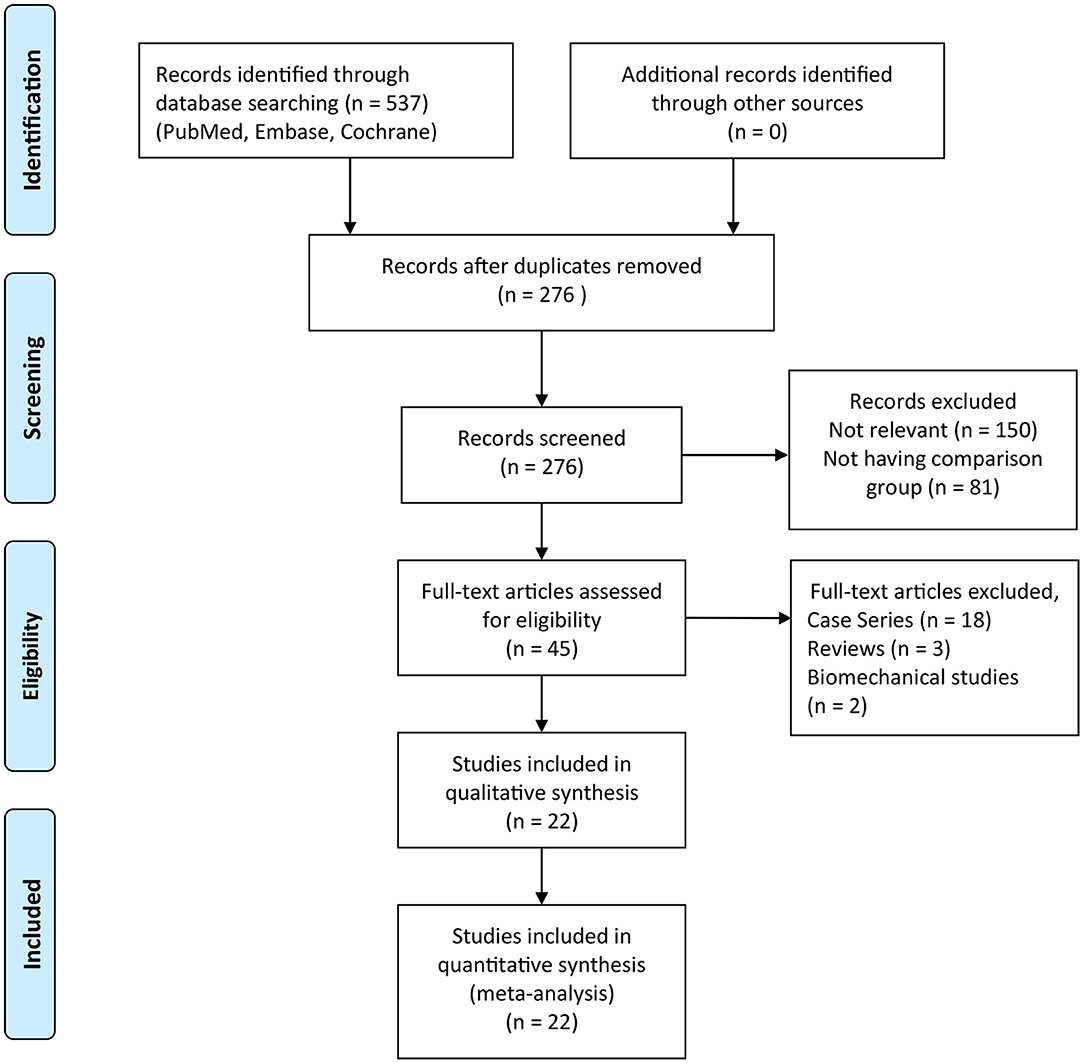
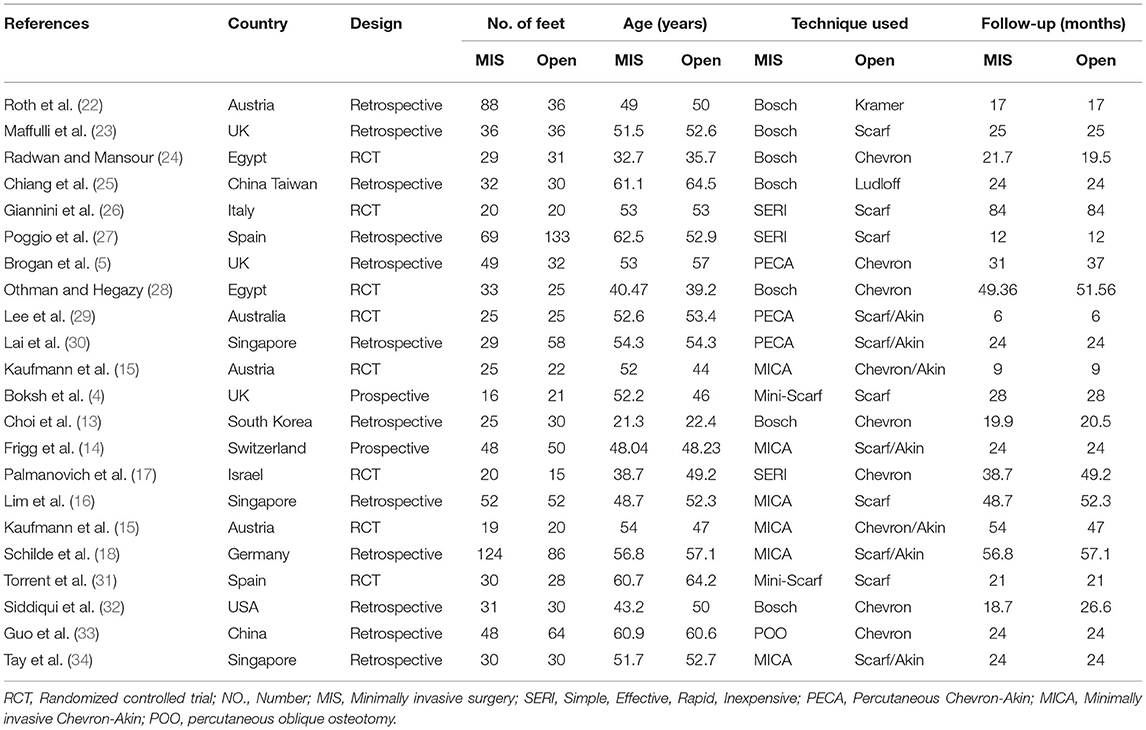
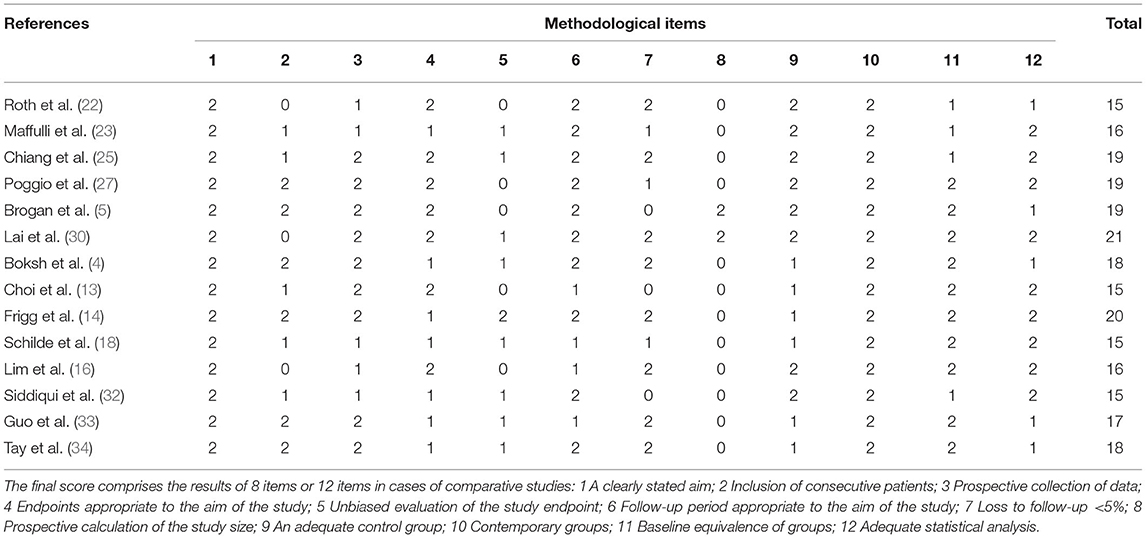
As presented in Figure 1, a total of 537 articles were identified after the primary literature search. After the removal of duplicates, 276 articles remained. During the screening of titles and abstracts of the remaining studies, 150 irrelevant articles and 81 articles without a comparison group were excluded, and a total of 45 articles remained. Then, full-text reviewing according to inclusion and exclusion criteria was conducted. A total of 23 articles (including 18 case series, 3 reviews, and 2 biomechanical studies) were eliminated. Eventually, 22 studies were included in this meta-analysis, in which 790 ft were treated with MIS procedure and 838 ft with the open procedure. The characteristics of the included studies are depicted in Table 1. Follow-up times were highly variable, ranging from 6 months to 7 years. Among the included studies, 8 studies (15, 17, 24, 26, 28, 29, 31, 35) were RCTs, 2 studies (4, 14) were prospective comparative studies, and 12 studies (5, 13, 16, 18, 22, 23, 25, 27, 30, 32–34) were retrospective comparative studies. A total of 10 studies (13, 17, 22–28, 32) reported on the 2G percutaneous hallux valgus surgery, in which 7 studies (13, 22–25, 28) involved Bösch osteotomy and 3 studies (17, 26, 27) involved a simple, an effective, a rapid, and an inexpensive (SERI) technique. Roth et al. (22) conducted a retrospective comparative study to compare between Bösch and Kramer osteotomies. Maffulli et al. (23) performed a comparison between the Bösch technique and open Scarf osteotomy. Radwan and Mansour (24) performed a RCT to compare between Bösch and Chevron osteotomies. Chiang et al. (25) performed a retrospective comparison between Bösch and Ludloff osteotomies. Giannini et al. (26) conducted a RCT to determine the efficiency of the SERI technique and scarf surgery. Poggio et al. (27) conducted a retrospective study to compare between the SERI technique and open scarf technique for hallux valgus. Othman and Hegazy (28) performed a RCT to compare between Bösch surgery and open Chevron osteotomy. Choi et al. (13) performed a retrospective comparison between the Bösch technique and Chevron surgery. Palmanovich et al. (17) conducted a RCT to compare between the SERI and Chevron technique. Siddiqui et al. (32) performed a retrospective comparison between Bösch and Chevron surgery. Nine studies (5, 14–16, 18, 29, 30, 34, 35) reported on the 3G percutaneous hallux valgus surgery, including percutaneous chevron–akin (PECA) and MICA. Brogan et al. (5) performed a retrospective study to compare between the PECA and Chevron technique. Lee et al. (29) conducted a RCT to compare between the PECA and open scarf/akin technique. Lai et al. (30) performed a retrospective comparison between the PECA and scarf/akin technique. Kaufmann et al. (35) conducted a RCT to compare between the MICA and chevron/akin technique. Frigg et al. (14) performed a prospective comparative study to compare between the MICA and scarf/akin technique. Lim et al. (16) performed a retrospective comparison between MICA and scarf surgery. Schilde et al. (18) conducted a retrospective comparative study to compare between the MICA and scarf/akin technique. Tay et al. (34) performed a retrospective study to compare between the MICA and scarf/akin surgery. Two studies (4, 31) performed a comparison of the mini-scarf with open scarf osteotomy. Guo et al. (33) conducted a retrospective comparative study for a comparison of percutaneous oblique osteotomy (POO) with open chevron osteotomy. The methodological quality of RCTs is shown in Figure 2. The MINORS score of comparative studies was 17.4 ± 2.0 (ranged from 15 to 21) (Table 2), which indicated a high quality of the included studies.
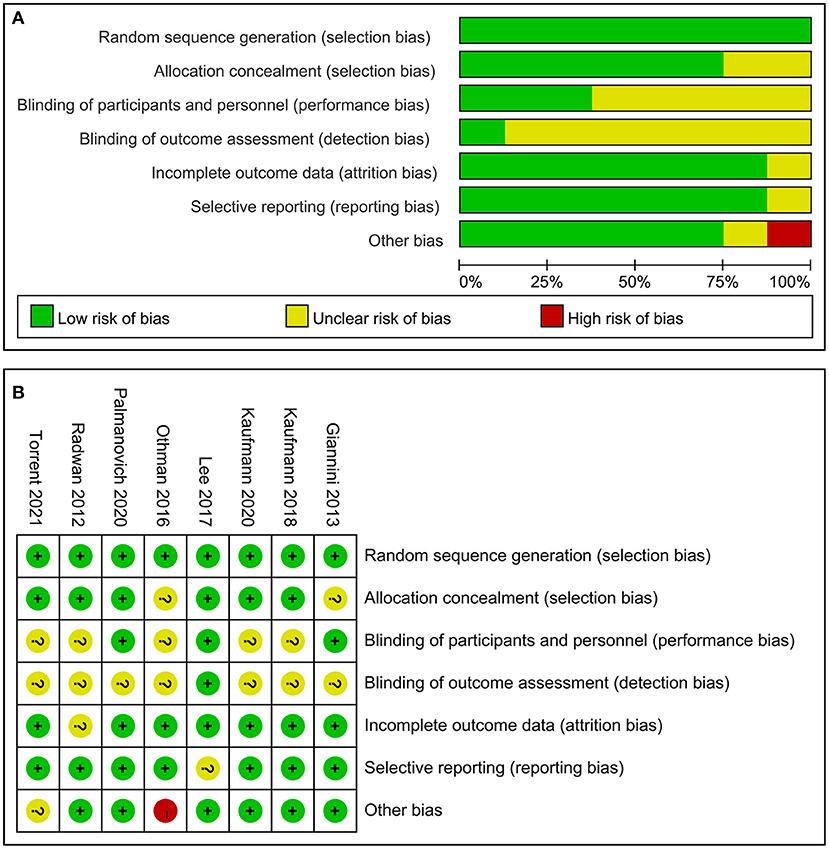
Figure 2. Quality assessment for randomized controlled trials (RCTs). (A) Risk of bias summary and (B) risk of bias graph.
Radiologic Outcomes
Hallux Valgus Angle
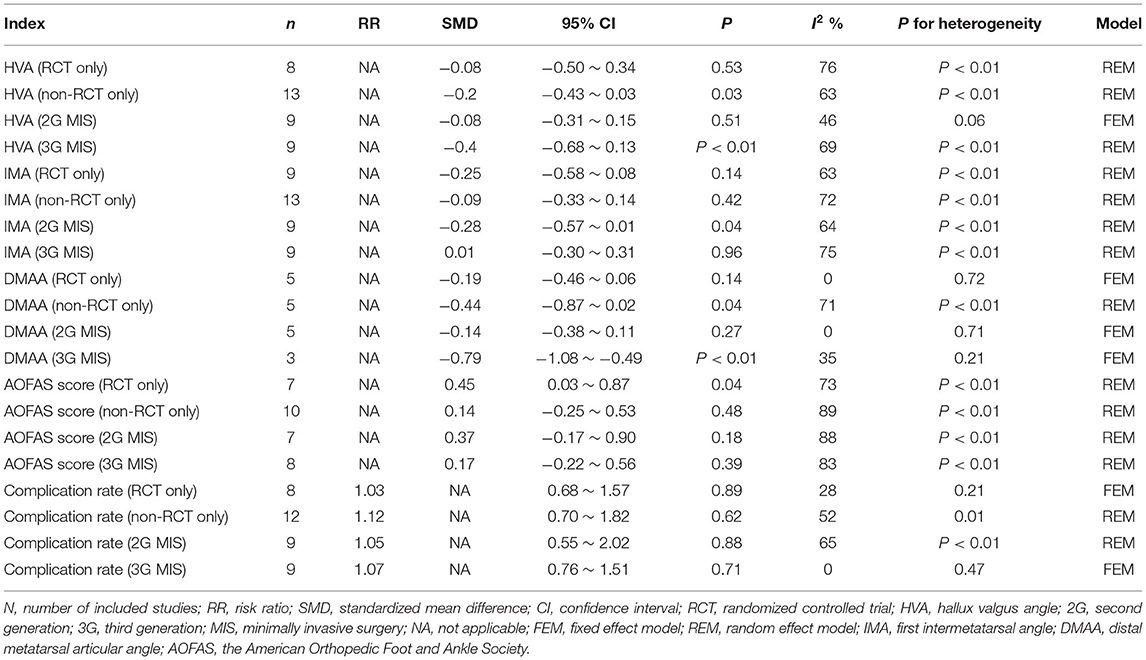
A total of 21 studies reported post-operative HVA. When evaluating all studies, the pooled SMD of HVA at the final follow-up was not significant between MIS and open groups (Figure 3A). When only studies reporting 3G MIS were included, the post-operative HVA was significantly lower in the MIS group (SMD: −0.4; 95% CI −0.68–0.13; p = 0.004; I2 = 69%;), but this significance was lost when comparing the just studies reporting 2G MIS (Table 3). Eight RCTs evaluated HVA, which did not reach a statistical significance (SMD: −0.08; 95% CI −0.50–0.34; p = 0.53; I2 = 76%; Table 3).

Figure 3. Forest plots of radiologic outcomes. (A) HVA between the MIS and open groups; (B) IMA; (C) DMAA; (D) the first metatarsal shortening; and (E) the medial sesamoid position correction. HVA, hallux valgus angle; MIS, minimally invasive surgery; IMA, first intermetatarsal angle; DMAA, distal metatarsal articular angle.
First Intermetatarsal Angle
First intermetatarsal angle was assessed in 21 studies, and there was no significant difference in the post-operative IMA between these two groups (Figure 3B). Nine RCTs documented IMA post-operatively, which demonstrated no statistical significance between MIS and open groups (SMD: −0.25; 95% CI −0.58–0.08; p = 0.14; I2 = 63%; Table 3). 2G MIS was assessed in 9 studies, which found that IMA was significantly lower in the MIS group (SMD: −0.28; 95% CI −0.57–0.01; p = 0.04; I2 = 64%; Table 3). However, the significance lost when comparing the studies reporting 3G MIS (SMD: 0.01; 95% CI −0.30–0.31; p = 0.96; I2 = 75%; Table 3).
Distal Metatarsal Articular Angle
A total of 10 studies provided a post-operative distal metatarsal articular angle (DMAA). The post-operative DMAA was significantly lower in the MIS group compared with the open group (SMD: −0.34; 95% CI −0.58–0.08; Z = −2.67; p = 0.007; I2 = 51%; Figure 3C). Three studies reported DMAA after 3G MIS, in which the post-operative DMAA was significantly lower in the MIS group (SMD: −0.79; 95% CI −1.08 to −0.49; p < 0.01; I2 = 35%; Table 3). Nevertheless, there was no significance between the MIS and open group when just comparing the 3G MIS studies (SMD: −0.14; 95% CI −0.38–0.11; p = 0.27; I2 = 0%; Table 3).
The First Metatarsal Shortening
Three studies assessed the first metatarsal shortening, in which there were 98 ft treated with the MIS procedure and 84 ft treated with the open procedure. As shown in Figure 3D, the pooled SMD was also not significant between these two groups.
Sesamoid Position Correction
A total of 4 studies (5, 13, 14, 25) reported the medial sesamoid position as demonstrated by Hardy and Clapham (36). The pooled results showed that there were more sesamoid position changes in the MIS group compared with the open group (SMD: 0.58; 95% CI 0.34–0.82; Z = 4.69; p < 0.001; I2 = 24%; Figure 3E).
Clinical Outcomes
AOFAS Score
The AOFAS score (37) was available in 17 studies, and no significant difference between MIS and surgery groups was observed (Figure 4A). Seven RCTs reported the AOFAS score, and demonstrated a higher score in the MIS group (SMD: 0.45; 95% CI 0.03–0.87; p = 0.04; I2 = 73%; Table 3). Subgroup meta-analysis of techniques (2G or 3G MIS) found no significant difference (Table 3).
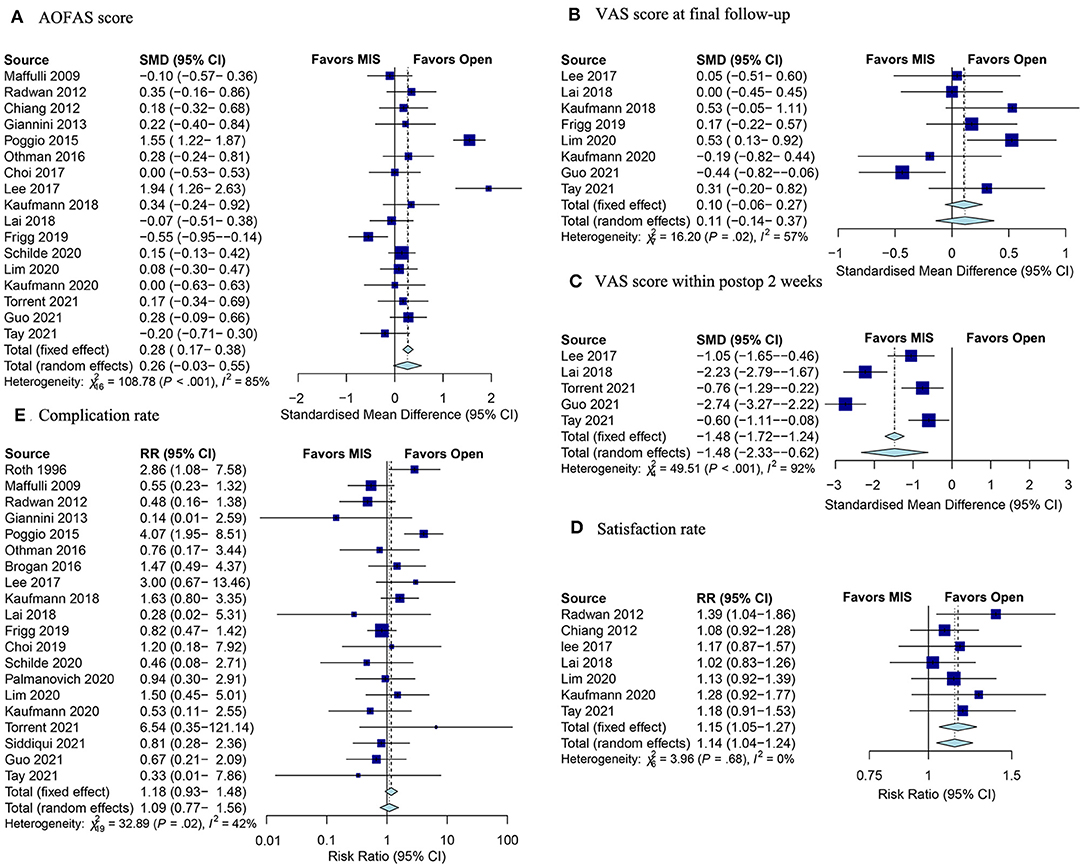
Figure 4. Forest plots of clinical outcomes. (A) SMD for the AOFAS score improvement between the MIS and open groups; (B) VAS score at the final follow-up; (C) VAS score within post-operative 2 weeks; (D) satisfaction rate; and (E) complication rate. SMD, standardized mean difference; AOFAS, the American Orthopedic Foot and Ankle Society; MIS, minimally invasive surgery; VAS, visual analog scale; postop, post-operative.
VAS Score
Eight studies were incorporated in the analysis of VAS score at the final follow-up (38). The overall results indicated no significant difference between MIS and open groups (Figure 4B). Besides, 5 studies assessed the VAS score within post-operative 2 weeks. The pooled results showed that the MIS procedure was associated with obviously less pain in the early post-operative phase (SMD: −1.48; 95% CI −2.33–0.62; Z = −3.38; p < 0.001; I2 = 92%; Figure 4C).
Satisfaction Rate
A total of 7 studies documented the satisfaction rate. The pooled results indicated that the satisfaction rate was remarkably higher in the MIS group (RR: 1.15; 95% CI: 1.05–1.27; Z = 3.09; p = 0.002; I2 = 0%; Figure 4D).
Complication Rate
There were some post-operative complications in MIS and open surgery for hallux valgus, such as screw irritation, recurrence, and non-union. In total, 20 studies reported complication rates. According to the pooled results, there was no difference between MIS and open groups with respect to the complication rate (Figure 4E). Subgroup analysis of study design (RCT or non-RCT) and techniques (2G or 3G MIS) demonstrated no significance difference in the complication rate between the two groups (Table 3).
Secondary Outcomes
Duration of Surgery
The duration of surgery was available in 7 studies. Figure 5A showed that the pooled SMD was statistically significant (SMD: −2.81; 95% CI −3.55 to −2.07; Z = −5.64; p < 0.001; I2 = 90%), indicating the less duration of surgery in the MIS group in comparison with the open group.
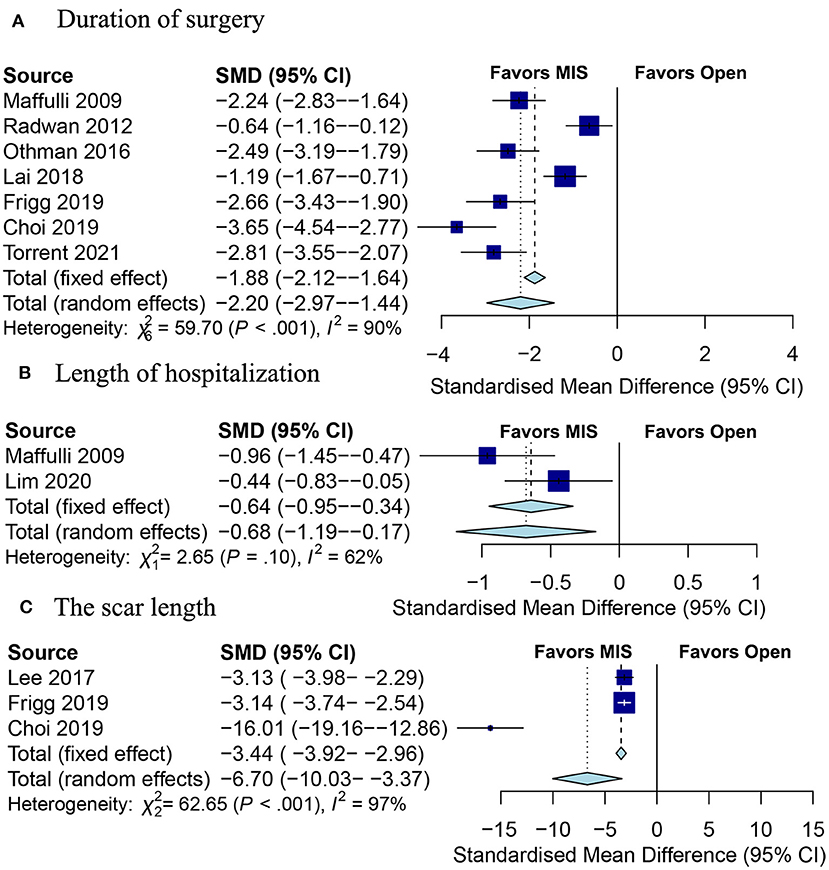
Figure 5. Forests plot of secondary outcomes between the MIS and open groups. (A) Duration of surgery; (B) length of hospitalization; (C) the scar length. MIS, minimally invasive surgery.
Length of Hospitalization
Two studies (16, 23) assessed the length of hospitalization, and the pooled results demonstrated that the MIS group was associated with a shorter length of hospitalization (SMD: −0.64; 95% CI −0.95 to −0.34; Z = −4.13; p < 0.001; I2 = 62%; Figure 5B).
The Scar Length
Three studies (13, 14, 29) documented the scar length. The pooled results indicated that the scar length was less in the MIS group as compared to the open group (SMD: −6.70; 95% CI −10.03 to −3.37; Z = −3.94; p < 0.001; I2 = 97%; Figure 5C).
Publication Bias
The Egger' test of HVA suggested that there was no obvious publication bias (p = 0.58).
Discussion
More than 150 open surgical procedures have been described for the treatment of hallux valgus (39). There was a trend toward more minimally invasive surgery for hallux valgus, involving the theoretical advantages of less soft tissue dissection, reduced surgical time, and a faster recovery time (3). In this meta-analysis, MIS procedure showed better radiologic and clinical outcomes compared with the open group.
Compared to the former meta-analysis conducted by Singh et al. (11), 13 new studies were included in this meta-analysis, making it more comprehensive. Most of the included studies in the meta-analysis performed by Lu et al. (12) were of low or moderate quality, and limited OMs were assessed due to incomplete information. Our meta-analysis included all new studies according to the inclusion and exclusion criteria and pooled 12 OMs.
Hallux valgus angle and IMA were the most common radiologic OMs to evaluate hallux valgus because they have been shown to determine the severity of hallux valgus. IMA correction was a marker to determine the corrective potential of a metatarsal osteotomy (40). Singh et al. (11) pooled 8 studies for HVA and IMA, showing no significant difference between MIS and open groups. Our meta-analysis found no significant difference in HVA and IMA between the two groups when all 22 studies were included. Nevertheless, post-operative IMA of the MIS group was significantly lower when only studies reporting 2G MIS were included. The 2G MIS was Bösch osteotomy or the SERI technique, which adopted an axial wire to displace and maintain the metatarsal head in the initial few weeks (5). When just studies adopted 3G MIS were included, the HVA were lower in the MIS group. Lai et al. (30) performed a comparison between the PECA and open scarf/akin technique, showing a better HVA correction but a comparable IMA correction in the MIS group. The 3G MIS included MICA and PECA. PECA is a modification from the MICA procedure as introduced by Vernois and Redfern (10). The MICA technique adopted phalangeal osteotomy with burr, which had a direct impact on the correction of HVA (35). Lim et al. (16) also demonstrated lower post-operative HVA in the MIS group, and they believed that it was possibly owing to the use of toe alignment splint after the MICA procedure. DMAA is the angle between the perpendicular line to the distal metatarsal articular surface and the first metatarsal axis. A pathological joint line is associated with a significantly increased recurrence rate (41), so it is essential to restore the DMAA. Brogan et al. (5) reported a trend toward a difference in DMAA in favor of the PECA group compared with the open chevron group, perhaps because of the effect of the wire causing a slight varus displacement of the metatarsal head fragment. Frigg et al. (14) performed a retrospective comparison of MICA with open scarf-akin surgery for hallux valgus and reported a lower DMAA in the MICA group. This meta-analysis pooled the data from 10 studies reporting DMAA, indicating a lower DMAA in the MIS group.
The diameter of burrs used in MIS procedures is about 2 mm, which may lead to shorter metatarsal compared with open techniques (5). The shortened first metatarsal will transfer more load to the lateral metatarsal heads, which could cause metatarsalgia (42). This meta-analysis indicated that MIS surgery do not cause more metatarsal shortening compared with open surgery.
The change of the sesamoid position was better in the MIS group than in the open group, which perhaps was due to more use of image intensifier. Okuda et al. (43) pointed out that insufficient sesamoid position correction was an important risk factor for hallux valgus recurrence, so the correction of the sesamoid position was needed.
The AOFAS score (37) was to evaluate the functional outcome, including pain (40 points), function (45 points), and alignment (15 points). Singh et al. (11) conducted a meta-analysis to demonstrate that the open group provided more improvement in the AOFAS score. Poggio et al. (27) reported that the open scarf technique showed more increases in the AOFAS score than the Kramer technique (also known as the 2G MIS technique). Radwan and Mansour (24) and Lee et al. (29) reported a trend toward a better improvement in the AOFAS score in the MIS group. This meta-analysis pooled 17 studies and found no difference in the improvement of the AOFAS score between the two groups. When taking into consideration only RCTs, the AOFAS score was higher in the MIS group. The VAS score of the early post-operative phase was lower in the MIS group, which reflected that the MIS surgery required a minor soft tissue dissection (15). The VAS score at the final follow-up was not found to be significant, which was in accordance with Singh's meta-analysis.
Singh's meta-analysis pooled 4 studies and found no significant difference in the satisfaction rate between MIS and open groups. Lu's meta-analysis pooled 3 studies and demonstrated a higher satisfaction level in the MIS group. Our meta-analysis included 7 studies, showing a higher satisfaction rate in the MIS group. The high satisfaction rate in the MIS was possibly due to the cosmetic result of surgery. Choi et al. reported 2G MIS for young female patients, and believed that the MIS technique could be considered for young female patients who desire a less visible scar (13). The scar length was significantly shorter in the MIS group. Because of the limited scar on the medial side, MIS is expected to result in fewer soft tissue complications, less stiffness, and a higher satisfaction rate.
The duration of surgery and the length of hospitalization were shorter in the MIS group, possibly due to the limited exposure and steps involved in the MIS technique (23). The shorter length of hospitalization in the MIS group made the MIS procedure a beneficial choice for high-risk patients suffering recurrent ulceration (23). However, Lai et al. reported that the fluoroscopy time was longer in the MIS group compared with the open group, involving higher radiation exposures (30).
Jowett et al. described a steep learning curve for MIS techniques. Jowett et al. made a comparison of a single surgeon series and found a higher reoperation rate and a lower satisfaction rate in the first 53 ft compared with the subsequent 53 ft (44). To minimize the learning curve, cadaveric training was recommended for any surgeon considering performing MIS surgery (30).
To our knowledge, this meta-analysis includes the largest number of studies (22 studies) evaluating the efficiency of MIS vs. open surgery for hallux valgus. There were some limitations in this meta-analysis. First, different surgical techniques were used in the MIS and open groups, involving a high heterogeneity. Secondly, non-randomized controlled studies were included; therefore, the results of this study must be interpreted with caution due to the natural defects of retrospective studies. Larger sample multicenter randomized controlled studies are needed to further verify the results of this meta-analysis.
Conclusion
The MIS procedures were more effective than open surgery in the treatment of hallux valgus. Moreover, the MIS group achieved better radiologic and clinical outcomes compared with the open group. The 2G MIS demonstrated better corrective power to IMA while the 3G MIS provided a stronger correction to HVA. The MIS procedures offered benefits mainly in the early post-operative period, including a shorter surgery time, a more cosmetic scar, a higher satisfaction rate, and a faster recovery time. These features of the MIS procedure make it a better choice for young female patients who favor a cosmetic scar and patients who are at high risk due to recurrent ulceration.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author Contributions
MZ designed this study. KW and SD conducted the literature search and data extraction. SD and CS performed quality assessment of the included studies. LJ and SS performed a statistical analysis. LJ and KW wrote this manuscript. All authors have read and approved this final manuscript.
Funding
This work was supported by the Natural Science Foundation of Beijing (Grant No. 7212020), Science and Technology Planning Project of Beijing Municipal Education Commission (Grant No. KM202110025013), and the Beijing Thousand Talents Project (Grant No. 2020A43).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Perez Boal E, Becerro de Bengoa Vallejo R, Fuentes Rodriguez M, Lopez Lopez D, Losa Iglesias ME. Geometry of the proximal phalanx of hallux and first metatarsal bone to predict hallux abducto valgus: a radiological study. PLoS ONE. (2016) 11:e0166197. doi: 10.1371/journal.pone.0166197
2. Palomo-López P, Becerro-de-Bengoa-Vallejo R, Losa-Iglesias ME, Rodríguez-Sanz D, Calvo-Lobo C, López-López D. Impact of hallux valgus related of quality of life in Women. Int Wound J. (2017) 14:782–5. doi: 10.1111/iwj.12695
3. Malagelada F, Sahirad C, Dalmau-Pastor M, Vega J, Bhumbra R, Manzanares-Céspedes MC, et al. Minimally invasive surgery for hallux valgus: a systematic review of current surgical techniques. Int Orthop. (2019) 43:625–37. doi: 10.1007/s00264-018-4138-x
4. Boksh K, Qasim S, Khan K, Tomlinson C, Mangwani J. A comparative study of mini-scarf versus standard scarf osteotomy for hallux valgus correction. J Foot Ankle Surg. (2018) 57:948–51. doi: 10.1053/j.jfas.2018.03.039
5. Brogan K, Lindisfarne E, Akehurst H, Farook U, Shrier W, Palmer S. Minimally invasive and open distal chevron osteotomy for mild to moderate hallux valgus. Foot Ankle Int. (2016) 37:1197–204. doi: 10.1177/1071100716656440
6. Russell NA, Regazzola G, Aiyer A, Nomura T, Pelletier MH, Myerson M, et al. Evaluation of nitinol staples for the lapidus arthrodesis in a reproducible biomechanical model. Front Surg. (2015) 2:65. doi: 10.3389/fsurg.2015.00065
7. López-López D, Larrainzar-Garijo R, De-Bengoa-Vallejo RB, Losa-Iglesias ME, Bayod-López J. Effectiveness of the Lapidus plate system in foot surgery: A PRISMA compliant systematic review. Int Wound J. (2021) 18:359–66. doi: 10.1111/iwj.13649
8. Isham SA. The Reverdin-Isham procedure for the correction of hallux abducto valgus. A distal metatarsal osteotomy procedure. Clin Podiatr Med Surg. (1991) 8:81–94.
9. Bösch P, Wanke S, Legenstein R. Hallux valgus correction by the method of Bösch: a new technique with a seven-to-ten-year follow-up. Foot Ankle Clin. (2000) 5:485–98. Available online at: https://europepmc.org/article/med/11232393
10. Vernois J, Redfern D. Percutaneous chevron; the union of classic stable fixed approach and percutaneous technique. Fuß Sprunggelenk. (2013) 11:70–5. doi: 10.1016/j.fuspru.2013.03.001
11. Singh MS, Khurana A, Kapoor D, Katekar S, Kumar A, Vishwakarma G. Minimally invasive vs open distal metatarsal osteotomy for hallux valgus - a systematic review and meta-analysis. J Clin Orthop Trauma. (2020) 11:348–56. doi: 10.1016/j.jcot.2020.04.016
12. Lu J, Zhao H, Liang X, Ma Q. Comparison of minimally invasive and traditionally open surgeries in correction of hallux valgus: a meta-analysis. J Foot Ankle Surg. (2020) 59:801–6. doi: 10.1053/j.jfas.2019.03.021
13. Choi JY, Ahn HC, Kim SH, Lee SY, Suh JS. Minimally invasive surgery for young female patients with mild-to-moderate juvenile hallux valgus deformity. Foot Ankle Surg. (2019) 25:316–22. doi: 10.1016/j.fas.2017.12.006
14. Frigg A, Zaugg S, Maquieira G, Pellegrino A. Stiffness and range of motion after minimally invasive chevron-akin and open scarf-akin procedures. Foot Ankle Int. (2019) 40:515–25. doi: 10.1177/1071100718818577
15. Kaufmann G, Mortlbauer L, Hofer-Picout P, Dammerer D, Ban M, Liebensteiner M. Five-Year follow-up of minimally invasive distal metatarsal chevron osteotomy in comparison with the open technique: a randomized controlled trial. J Bone Joint Surg Am. (2020) 102:873–9. doi: 10.2106/JBJS.19.00981
16. Lim WSR, Rikhraj IS, Koo KOT. Simultaneous bilateral hallux valgus surgery: percutaneous or conventional? Early results of a matched study from a tertiary institution. Foot Ankle Surg. (2020) 27:377–80. doi: 10.1016/j.fas.2020.04.014
17. Palmanovich E, Ohana N, David S, Small I, Hetsroni I, Amar E, et al. Distal chevron osteotomy vs the simple, effective, rapid, inexpensive technique (SERI) for mild to moderate isolated hallux valgus: a randomized controlled study. Indian J Orthop. (2020) 55:110–8. doi: 10.1007/s43465-020-00209-0
18. Schilde S, Delank KS, Arbab D, Gutteck N. Minimally invasive vs open akin osteotomy. Foot Ankle Int. (2021) 42:278–86. doi: 10.1177/1071100720962411
19. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
20. Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane Handbook for Systematic Reviews of Interventions. Chichester: John Wiley & Sons (2019).
21. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. (2003) 73:712–6. doi: 10.1046/j.1445-2197.2003.02748.x
22. Roth A, Kohlmaier W, Tschauner CJF, Surgery A. Surgery of hallux valgus. Distal metatarsal osteotomy—subcutaneous (‘Bösch') versus open (‘Kramer') procedures. Foot Ankle Surgery. (1996) 2:109–17. doi: 10.1046/j.1460-9584.1996.00009.x
23. Maffulli N, Longo UG, Oliva F, Denaro V, Coppola C. Bosch osteotomy and scarf osteotomy for hallux valgus correction. Orthop Clin North Am. (2009) 40:515–24. doi: 10.1016/j.ocl.2009.06.003
24. Radwan YA, Mansour AM. Percutaneous distal metatarsal osteotomy versus distal chevron osteotomy for correction of mild-to-moderate hallux valgus deformity. Arch Orthop Trauma Surg. (2012) 132:1539–46. doi: 10.1007/s00402-012-1585-5
25. Chiang CC, Lin CF, Tzeng YH, Huang CK, Chen WM, Liu CL. Distal linear osteotomy compared to oblique diaphyseal osteotomy in moderate to severe hallux valgus. Foot Ankle Int. (2012) 33:479–86. doi: 10.3113/FAI.2012.0479
26. Giannini S, Cavallo M, Faldini C, Luciani D, Vannini F. The SERI distal metatarsal osteotomy and scarf osteotomy provide similar correction of hallux valgus. Clin Orthop Relat Res. (2013) 471:2305–11. doi: 10.1007/s11999-013-2912-z
27. Poggio D, Melo R, Botello J, Polo C, Fernandez de Retana P, Asuncion J. Comparison of postoperative costs of two surgical techniques for hallux valgus (Kramer vs. scarf). Foot Ankle Surg. (2015) 21:37–41. doi: 10.1016/j.fas.2014.09.004
28. Othman AMA, Hegazy IHA. Treatment of mild to moderate hallux valgus, percutaneous osteotomy versus distal chevron osteotomy. Open J Orthop. (2016) 06:150–7. doi: 10.4236/ojo.2016.66023
29. Lee M, Walsh J, Smith MM, Ling J, Wines A, Lam P. Hallux valgus correction comparing percutaneous chevron/akin (PECA) and open scarf/akin osteotomies. Foot Ankle Int. (2017) 38:838–46. doi: 10.1177/1071100717704941
30. Lai MC, Rikhraj IS, Woo YL, Yeo W, Ng YCS, Koo K. Clinical and radiological outcomes comparing percutaneous chevron-akin osteotomies vs open scarf-akin osteotomies for hallux valgus. Foot Ankle Int. (2018) 39:311–7. doi: 10.1177/1071100717745282
31. Torrent J, Baduell A, Vega J, Malagelada F, Luna R, Rabat E. Open vs minimally invasive scarf osteotomy for hallux valgus correction: a randomized controlled trial. Foot Ankle Int. (2021) 42:982–93. doi: 10.1177/10711007211003565
32. Siddiqui NA, Mayer BE, Fink JN. Short-Term, retrospective radiographic evaluation comparing pre- and postoperative measurements in the chevron and minimally invasive distal metatarsal osteotomy for hallux valgus correction. J Foot Ankle Surg. (2021) 60:1144–8. doi: 10.1053/j.jfas.2021.04.019
33. Guo C-J, Li C-G, Li X-C, Xu Y, Cai M, Xu X-Y. Hallux valgus correction comparing percutaneous oblique osteotomy and open chevron osteotomy at a 2-year follow-up. Orthop Surg. (2021) 13:1546–55. doi: 10.1111/os.13029
34. Tay AYW, Goh GS, Koo K, Yeo NEM. Third-Generation minimally invasive chevron-akin osteotomy for hallux valgus produces similar clinical and radiological outcomes as scarf-akin osteotomy at 2 years: a matched cohort study. Foot Ankle Int. (2021) 5:10711007211049193. doi: 10.1177/10711007211049193
35. Kaufmann G, Dammerer D, Heyenbrock F, Braito M, Moertlbauer L, Liebensteiner M. Minimally invasive versus open chevron osteotomy for hallux valgus correction: a randomized controlled trial. Int Orthop. (2018) 43:343–50. doi: 10.1007/s00264-018-4006-8
36. Hardy RH, Clapham JCR. Observations on hallux valgus; based on a controlled series. J Bone Joint Surg Br. (1951) 33:376–91. doi: 10.1302/0301-620X.33B3.376
37. Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. (1994) 15:349–53. doi: 10.1177/107110079401500701
38. Price DD, McGrath PA, Rafii A, Buckingham B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain. (1983) 17:45–56. doi: 10.1016/0304-3959(83)90126-4
39. Robinson AHN, Limbers JP. Modern concepts in the treatment of hallux valgus. J Bone Joint Surg Br. (2005) 87:1038–45. doi: 10.1302/0301-620X.87B8.16467
40. Deenik AR, de Visser E, Louwerens J-WK, de Waal Malefijt M, Draijer FF, de Bie RA. Hallux valgus angle as main predictor for correction of hallux valgus. BMC Musculoskelet Disord. (2008) 9:1–6. doi: 10.1186/1471-2474-9-70
41. Iyer S, Demetracopoulos CA, Sofka CM, Ellis SJ. High rate of recurrence following proximal medial opening wedge osteotomy for correction of moderate hallux valgus. Foot Ankle Int. (2015) 36:756–63. doi: 10.1177/1071100715577195
42. Jung H-G, Zaret DI, Parks BG, Schon LC. Effect of first metatarsal shortening and dorsiflexion osteotomies on forefoot plantar pressure in a cadaver model. Foot Ankle Int. (2005) 26:748–53. doi: 10.1177/107110070502600913
43. Okuda R, Kinoshita M, Yasuda T, Jotoku T, Kitano N, Shima H. Postoperative incomplete reduction of the sesamoids as a risk factor for recurrence of hallux valgus. J Bone Joint Surg Am. (2009) 91:1637–45. doi: 10.2106/JBJS.H.00796
Keywords: minimally invasive, percutaneous, hallux valgus, bunion, osteotomy
Citation: Ji L, Wang K, Ding S, Sun C, Sun S and Zhang M (2022) Minimally Invasive vs. Open Surgery for Hallux Valgus: A Meta-Analysis. Front. Surg. 9:843410. doi: 10.3389/fsurg.2022.843410
Received: 25 December 2021; Accepted: 21 February 2022;
Published: 21 March 2022.
Edited by:
Daniel López-López, University of A Coruña, SpainReviewed by:
Dong Jiang, Peking University Third Hospital, ChinaMinwei Zhao, Peking University Third Hospital, China
Copyright © 2022 Ji, Wang, Ding, Sun, Sun and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mingzhu Zhang, michaelzhang120@hotmail.com
 Linfeng Ji
Linfeng Ji Ketao Wang
Ketao Wang Shenglong Ding
Shenglong Ding Chengyi Sun
Chengyi Sun Songmin Sun
Songmin Sun Mingzhu Zhang
Mingzhu Zhang