- 1School of Nursing, Oregon Health and Science University, Portland, OR, United States
- 2Oregon Center for Aging and Technology, Oregon Health & Science University (OHSU), Portland, OR, United States
- 3National Institute on Aging (NIA) - Layton Aging and Alzheimer's Disease Research Center, OHSU, Portland, OR, United States
- 4Department of Psychology, Portland State University, Portland, OR, United States
- 5Glenn Biggs Institute for Alzheimer's and Neurodegenerative Diseases, University of Texas Health Sciences Center San Antonio, San Antonio, TX, United States
- 6William F. Connell School of Nursing, Boston College, Chestnut Hill, MA, United States
Objective: The objective of this study was to examine associations between level of depressive symptoms in older adult spouse/partner couples and their physical health and social factors (social activity and number of close friends).
Methods: Using data from 116 community-dwelling couples (age 76.2 ± 8.5), we simultaneously analyzed associations between depressive symptoms (Geriatric Depression Scale, range 0–11) and dyadic physical health, engagement in social activities, and connectedness with close friends.
Results: Greater engagement in social activities was associated with fewer depressive symptoms in men, whereas more close friendships were associated with fewer depressive symptoms in women, controlling for partner effects, age, education, and cognitive function, with good model fit. Additionally, more disparate physical health within the couple (latent incongruence score) was associated with greater depressive symptoms in men.
Discussion: Less social activity and fewer close friends were associated with depressive symptoms in older adult couples, but may be distinctly influential depending on gender and in the context of the older adult couple's physical health.
Introduction
It is well-known that major depressive disorder is less common among adults ages 65 and older than in adults of any other age in the United States (1, 2). Yet, the prevalence of mild depressive symptoms (i.e., subsyndromal depression) is similar across all community-dwelling adult age groups in the United States (roughly 10%), and the consequences of subsyndromal depression for older adults in particular include elevated risk of morbidity and lower quality of life (3–5). Known protective factors against depressive symptoms among older adults include better physical health (6), and social factors such as social engagement (7–9) and social connectedness (10–12). While the majority of older adults are married or have a co-habiting intimate partner relationship (13), few studies have considered the context of the physical health of the couple (rather than the individual), or the added and potentially distinct benefits beyond marriage of engaging in social activity and maintaining social connectedness with friends.
Dyadic theory and context for mental health in couples
Research provides consistent evidence of the health benefits of being married or partnered (14, 15), yet there is also clear indication that older adults' health problems can negatively impact their partners' mental health (16–19). Incongruent physical health in a dyad (i.e., differences between partners' health) has implications for imbalances in the relationship, shifting social roles (e.g., caregiving), and overall mental health (20). Thus, it is important to look beyond individual-level physical health and consider how the dyad's health as a unit may be contributing to depressive symptoms.
Interdependence theory and related research explains that for older adults who are married or partnered, their health, behaviors and social milieu are also interdependent and connected as a couple (10, 21, 22). There are gender differences, though, in the manner and degree to which one construes their identity as interdependent (23). Markus and Kitayama (24) posit the interdependent self-construal is more magnified in women, who are socialized to be caring and closely bonded with others; whereas, the independent self-construal is magnified in men, who are more socialized to stand out from their peers and lead. Alternatively, a more relational typology of interdependence is proposed as dominant in females (i.e., interdependence with one's partner and other dyadic bonds such as close friends), vs. a more collectivist typology of interdependence in males (i.e., self-construed as is interdependent with the group or community to which one belongs) (25).
Spouses and close intimate partners are vital social ties that contribute to wellbeing and also enhance social opportunities (26). Yet little dyadic research has examined the distinct roles of other social factors–beyond the effects of one's partner–on the mental health of the older couple. Social-Emotional Selectivity Theory, though not a dyadic theory, posits that older adults experience an intrinsic motivational shift to de-emphasize potentially negative social and emotional influences and maximize positive ones in accordance with the degree to which it is perceived that there is limited time left to achieve one's life goals (27). The ability to identify and select positive social and emotional influences and give less attention to negative ones contributes to enhanced emotional regulation and helps explain the paradox of lower rates of depression among older adults despite greater physical health challenges (28). By selecting the marital context for examining the influence of social factors on depression, it allows us to examine the additive benefit of social connectedness and social activity engagement beyond the support and enrichment that is available through one's own spouse. Additionally, it allows us to examine partner effects that may be present due to the “marital capital” that is gained by having access to a partner's social network and activities (10, 29).
The protective role of social factors
Social connectedness with close friends and engaging in social activities are clearly related (30), but the two constructs and the benefits they convey are also be distinct. Close friends are the strongest forms of social connections and are considered vital relationships: they provide social support, and prevent social isolation, loneliness (30–33). More frequent contact with close friends is also associated with fewer depressive symptoms in older adults (11) and among other age groups (34). Social activities, on the other hand, can be engaged in without close friends (e.g., playing a game with an acquaintance), but enrich and involve older adults in a facet of life that is beyond one's necessary activities of daily living (35). Social activities are also associated with a lower risk of developing depressive symptoms as well as an improvement in depressive symptoms when present (8, 9).
It is possible to have and benefit from close friends without engaging in social activities, just as it is possible to engage in and benefit from social activities without having close friends. Though the two can also be interrelated, it is necessary to simultaneously examine the distinct protective benefit that each concept may offer against depressive symptoms. In a rare example, one study of older adults examined the impact of diverse social ties and daily activities on behaviors and daily mood, and found that interactions with close friends and engagement in diverse behaviors (i.e., social activities) both improved daily positive mood, but did not decrease daily negative mood (36). Although this study provided important insight into the minutia of social factors and daily mood shifts, it is still unclear what the distinct protective influences of social connectedness and engagement in social activities are against depression in older adults. Further research is needed in order to understand and help promote the benefits of social factors for mental health.
Study objective
The overall objective of this study was to examine the associations between dyadic health, social activity and social connectedness on depressive symptoms in older adult couples. We expected to observe: (1) associations between one's own social activities and close friends on one's own level of depressive symptoms, such that higher levels of both social measures would be associated with lower levels of depression; (2) one's partner's levels of social measures would also be related to depressive symptoms in couples; and (3) an association between incongruent dyadic physical health and depressive symptoms.
Methods
Sample
Cross-sectional data from community-dwelling older adult couples in the Pacific Northwest region of the United States (primarily Portland, Oregon and surrounding areas) who participated in observational studies between the years of 2011–2019 were included in this secondary analysis. Each of the three original studies' recruitment and inclusion criteria are detailed in previously published papers (37–39). The inclusion criteria for minimum age of the primary participant enrolling: 50 years of age or older (39), 62 years of age or older (37), and 80 years or older (38), respectively, however there was no age restriction on co-habiting spouses/partners for the original studies. For this analysis data from participants who lived alone were excluded, and data from all participants who were living with a spouse/partner at the time of completing the baseline measure of depressive symptoms were included in this analysis. In total, the current study included data from 116 co-habiting spouses or partners (a total of 232 older adults). All data were collected prior to the start of social distancing and other social restrictions imposed during the COVID-19 pandemic. A clinical assessor from the study team collected data from participants in-person on health variables (depressive symptoms, physical health, and cognitive function). All other study variables were collected with an online survey (via Qualtrics) at the same time point as the in-person visit. Ethical approval was obtained from a university health center IRB for data to be stored and shared through a data repository, which was accessed for the current study.
Measures
Depressive symptoms
Depressive symptoms were measured with the 15-item Geriatric Depression Scale (GDS), which is a valid and reliable self-report screening instrument for assessing depressive symptoms in older adults (40). A research clinician completed the GDS with participants during in-person study visits. Responses are yes/no and the scale range is 0–15, with 1 point assigned for each item endorsed with a yes response. Depressive symptoms were treated as a continuous variable in this study, however the clinical diagnostic relevance of scores of 0–2 can be interpreted as no depression, scores of 3–5 as subsyndromal depression, and scores of 6+ as syndromal depression (3).
Engagement in social activity
Engagement in social activity was measured by the frequency (0 = rarely or never, 1 = yearly, 2 = monthly, 3 = weekly, 4 = daily) of engaging in eight activities: visits from others, visits to others, eating meals out in restaurants, spending time doing hobbies or games, attending clubs or group meetings, attending a class, attending church or religious services, and travel out of town. Items were averaged across all eight activities for a scale score range of 0–4. This measure was adapted from the Brief Assessment of Social Engagement scale (41).
Social connectedness
Social connectedness from close friends was self-reported with a single item on a scale of 0–5, where a response choice of 5 = 9 or more close friends, a score of 4 = 5–8 close friends, a score of 3 = 3 or 4 close friends, a score of 2 = 2 close friends, 1 = 1 close friend, and 0 = 0 close friends.
Physical health
Physical health was measured using the modified Cumulative Illness Rating Scale (M-CIRS), which has 14 items, each representing the presence of an illness type that is rated on a 5-point Likert-type scale of severity (0 = “None” to 4 = “Extremely Severe”) (42). The total score ranges from 0 to 56, with a higher score indicating more severe illness, or less physical health. A research clinician completed the M-CIRS with participants during in-person study visits. Reliability of the M-CIRS was not calculated for this study due to the nature of the scale's items, which each focus on a distinct source of pathology (e.g., cardiovascular or psychiatric). Thus, we would not necessarily expect items to be correlated. Previous research has established the test-retest reliability of the CIRS-G and its validity with a sample of community-dwelling older adults (42).
Cognitive function
Cognitive function was measured using the 30-point Mini-Mental State Examination (MMSE) (43) among 68 couples, and the MMSE conversion equivalency score (44, 45) was used for this analysis for the remaining 41 couples who completed the 30-point Montreal Cognitive Assessment (MoCA-30) (46). The MMSE is designed for clinician assessment of 11 cognitive domains spanning aspects of orientation, working memory, language, delayed recall, attention, and comprehension. The scale range is 0–30, with higher scores indicating higher cognitive function. The resulting variable for cognitive function in this sample was a unified score from the MMSE/MMSE conversion scale. Although there are differences in the emphasis on domains measured by the MoCA vs. the MMSE, both scales are widely used and it is often necessary to convert scores from one scale to the other (44, 45).
Demographic variables
Demographic variables included self-reported gender identity, age in years, race, ethnicity, and education in number of years completed. Age and education were included as covariates based upon previous literature indicating the effects of education on social factors and depressive symptoms (7, 9, 10, 12, 36), as well as our theoretical framework specifying that adults become increasingly more selective of social influences as they age (27), and that education expands the intrinsic and extrinsic resources available to older adults' for emotional regulation (28).
Analytic approach
Dyadic modeling
In order to examine the relationship between social factors and depressive symptoms in older adult couples, we adopted a dyadic modeling perspective wherein measures and outcomes for both partners are modeled simultaneously. Specifically, the Actor Partner Interdependence Model (APIM) (47) was used to assess both individual level, or actor effects, along with any potential reciprocal, or partner, effects of social factors, physical health, and cognitive function on levels of mental health. Structural equation modeling (SEM) was used since it provides a straightforward way to specify individual and reciprocal effects for both partners simultaneously. This approach also addresses the dependence inherent in measuring partners in a relationship, wherein individual socializing or health behaviors are interdependent. Such interdependence violates traditional statistical assumptions which treat each individual and their observations as independent.
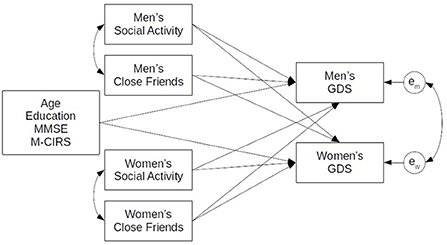
The integrated model examined the associations between social factors, measured through close friends (friends) and social activities (soc8), on depressive symptoms (GDS) of individuals living together in a couple. In the model, levels of GDS for both partners were associated by individual levels of soc8 and friends as well as soc8 and friends from their partner. A structural model diagram of this APIM model is illustrated in Figure 1. This allowed us to assess both types of effects, actor and partner, simultaneously while also addressing missing data through use of full information maximum likelihood (FIML) for model estimation. All models were estimated using R version 3.6.3 (2020-02-29), and the package lavaan 0.6-5 for structural equation modeling. Syntax for these analyses is provided in Appendix A.
Model fit was assessed using a combination of indices including the Chi square (p-values > 0.05 indicative of close model fit), the comparative fit index (CFI) and the Tucker Lewis Index (TLI), both of which compare the fit of the specified model to that of a null model (values > 0.95 for both indices indicative of good model fit), the Root Mean Square Error of Approximation (RMSEA), a per degree of freedom index of model fit (values < 0.05 indicative of good model fit), and the Standardized Root Mean Square Residual (SRMR) with values < 0.08 considered a good fit (48–50). Significance is reported at the level of p < 0.05.
Procedure for analyzing dyadic physical health
In order to incorporate physical health from a dyadic health perspective (51) in our analyses, we adopted a second-order approach wherein individual scores on a measure are replaced by a dyad level average and a dyad level difference (incongruence) score (52, 53). Specifically, we incorporated two latent variables (procedure specified in R using the code in Appendix A). The first indexed the average level of physical health by constraining the loadings from the latent variable to both partner measures to be equal to one. The other latent variable coded the incongruence between partners' physical health by setting one partner's loading to 0.5 and the other to −0.5 thus indexing the difference between partner measures. With these two latent measures specified, we were able to assess the associations between both the couple level average and the degree of incongruence in physical health on each partner's level of depressive symptoms.
Results
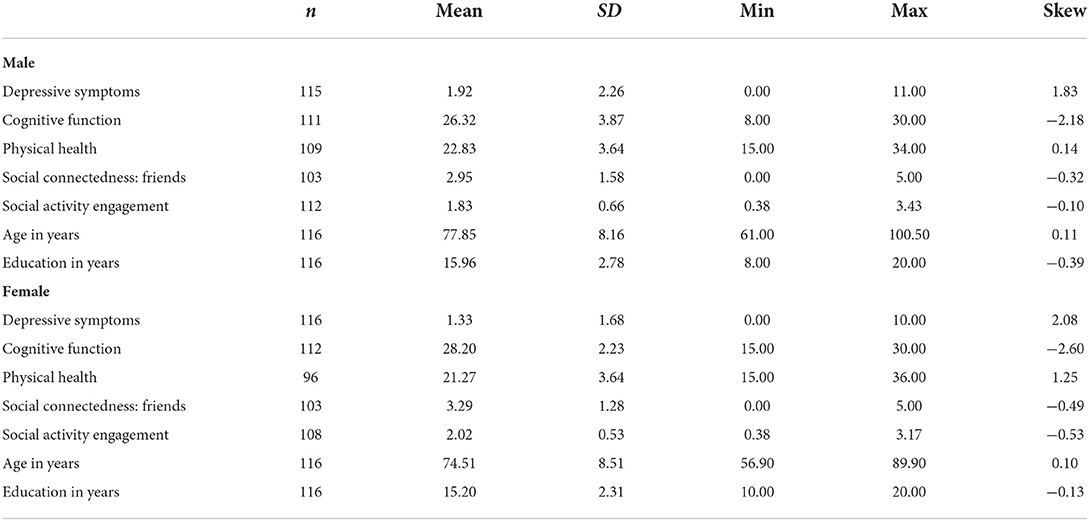
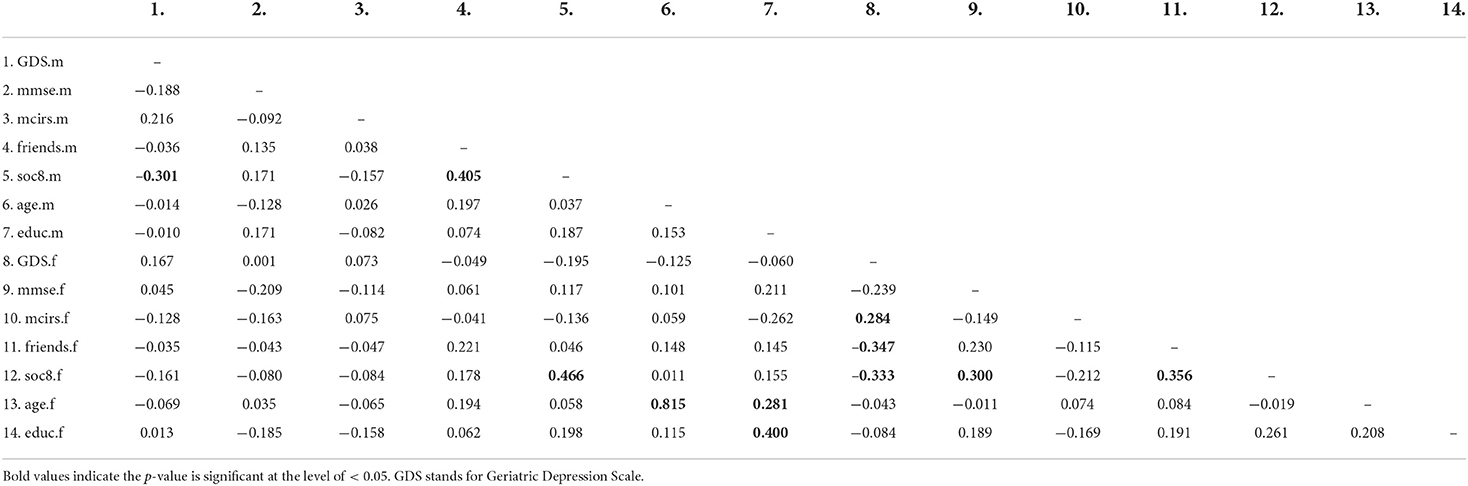
Depressive symptoms were low on average for both women (1.33 ± 1.68) and men (1.92 ± 2.62), but among the 116 couples, scores for 14 women (12%) and 19 men (16%) were indicative of subsyndromal depression, and scores for 4 women (3%) and 9 men (8%) were indicative of syndromal depression. Women and men in the sample were, on average, 75 and 78 years of age, respectively, of predominantly non-Hispanic white ethnicity/race (91%), and had obtained on average some college education. Means and standard deviations for all study variables are provided in Table 1. Pairwise correlations between study variables are provided in Table 2.
Our dyadic model included depressive symptoms for both partners which were simultaneously regressed on social measures (activity engagement and number of close friends) from both the individual and their partner, and dyadic health, controlling for age, cognitive function, and years of education (Table 3). Greater engagement in social activities was associated with fewer depressive symptoms in men, whereas more close friendships were associated with fewer depressive symptoms in women, controlling for partner effects (NS), age (NS), cognitive function (NS), and education (NS), with good model fit.
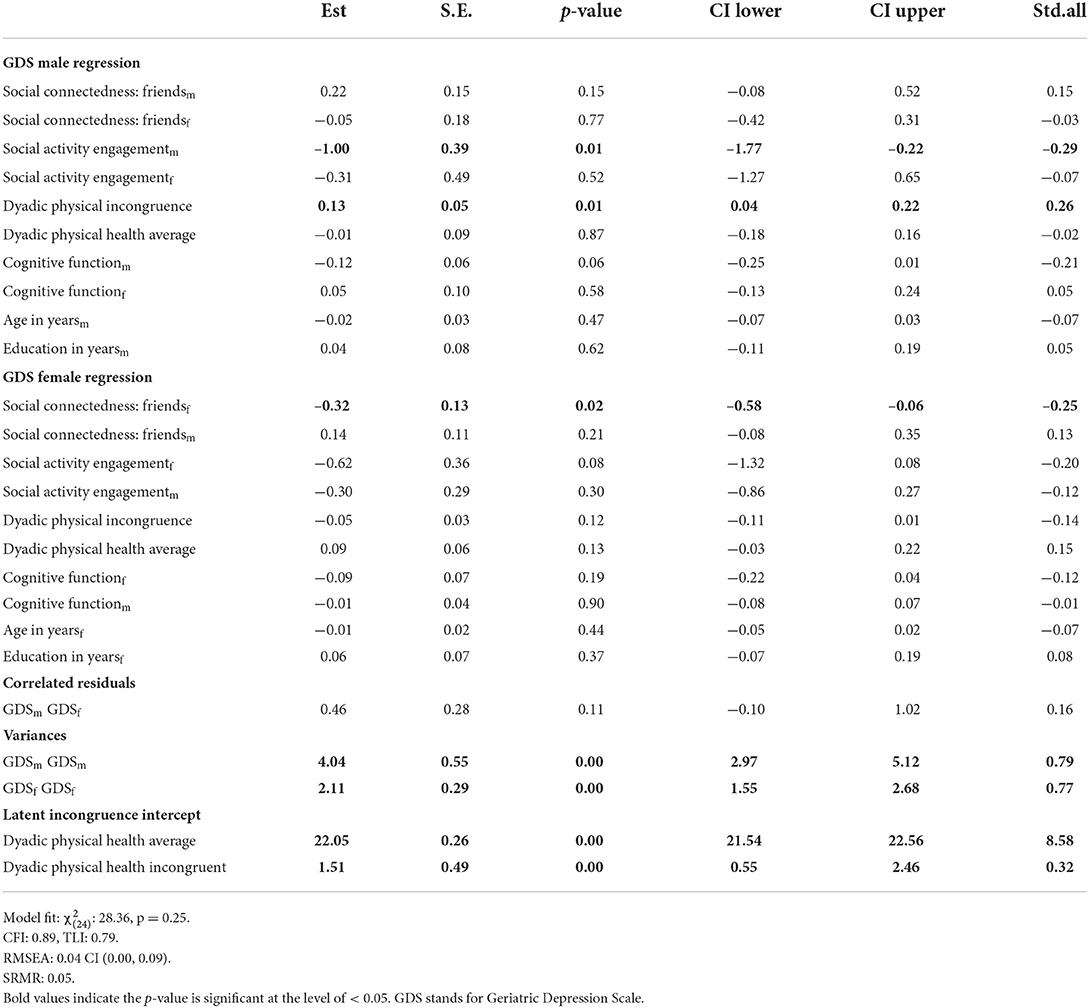
Table 3. Associations between social factors and depressive symptoms within the context dyadic physical health.
Our model also simultaneously incorporated dyadic physical health, which allowed us to compare whether it was the overall level of dyadic health in the couple that was the salient factor for higher levels of depressive symptoms, or whether it was the incongruence/discordance between partners regarding physical health that was significant, since both of these aspects of dyadic physical health have potential implications for mental health (54). From the results in Table 3, it can be seen that greater incongruence in couples' physical health was significantly associated with males' depressive symptoms. The coding of the incongruence was such that positive values indicated higher levels of physical illness for males than for females. Thus, men exhibited greater depressive symptoms in this study when there was more incongruence between their own amount of physical illness and their (more often healthier) female partner's.
Discussion
This study found that social activity and connectedness are positively associated with mental health in older adult couples, but appear to be distinctly influential depending on the individual's gender and in the context of the dyad's health. The findings of this study support our hypotheses that social factors may protect against depressive symptoms, however we did not find partner effects that suggested that social engagement or connectedness of one's partner influenced older adults depressive symptoms. This study builds upon the existing literature by highlighting the differential benefits of two distinct social factors–social activity engagement for men and social connectedness from close friends for women. This study also highlights the association between the couple's physical health and depressive symptoms, with a novel focus and methodological approach to dyadic incongruence in physical health.
A recent review of friendship in late life specifically noted the need for greater understanding of gender effects (30). In this study, our expectation for the first study hypothesis was supported, and we found that more close friends were associated with fewer depressive symptoms, however the finding was only among women in older adult couples, and not in men. This confirms findings from other recent studies of depressive symptoms in older adult couples (10, 29), and across a larger (non-dyadic) study that found women, but not men, report greater depressive symptoms when they lack a close friend (55). These findings also support theoretical explanations of gender differences in interdependence, and the importance that women place on social relationships (24, 25).
Although it is thus not a surprise that women significantly benefitted from more close friends, it was surprising that our expectation for the second study hypothesis was not supported and there was no partner/cross-over benefit to men. Husbands are often part of their wife's social network and thus may benefit from the marital capital (10). Our study adds to this body of literature by including the effects of engagement in social activities in the analysis. Indeed, another gender-specific finding of this study is that higher engagement in social activities were associated with fewer depressive symptoms in men, but not women. In the context of protecting against depressive symptoms, this distinct social influence may reflect “his and hers interdependence”, with a more collectivist typology related to shared social activities in men (25). Extending this to the marital context, these two distinct findings favor a gender-as-relational model from within a social construct (marriage) that is inextricably linked to health (56).
The results of this study also indicated support for our third study hypothesis with a negative association between incongruent dyadic physical health within couples on the mental health of men. This incongruence represents an imbalance in health within the couple that may disturb the homeostasis of the relationship, placing the couple in a vulnerable context where roles may shift (e.g., one partner providing care to another, or recognition that one partner is becoming more frail) (20, 57). Men in particular may feel less prepared or socialized for viewing themselves as being more frail or needing more care than their female partners. Recent research by Polenick et al. (54) found incongruence in type of chronic health conditions was significantly associated with higher depressive symptoms for husbands but not wives. An imbalance in physical health within couples may diminish the ability to remain as socially active and require renegotiations within the dyad regarding household tasks, lifestyle, and in some cases daily management of illness (e.g., diabetes). Although an emerging area of research, the research on dyadic health emphasizes the importance of understanding the implications of imbalance in health within dyads (and particularly couples) through the use of dyadic approaches and second-order dyadic variables (20, 53). These approaches are also crucial to fully evaluate interventions that are efficacious for the dyad, not just the individuals within it (20, 57).
Limitations
We were unable to examine the influence of spousal relationship quality in this secondary dyadic analysis, which may help to further distinguish the benefits of social activities or social connectedness to older adults' mental health (11), or the potential interactions between types of social engagement and being in a spousal relationship with mental health in couples (58). It is possible that support from spouses would also mitigate the effect of incongruent dyadic health on depressive symptoms (59). Our definition of social connectedness from close friends is narrower than one that includes all types of social connections, and our measure is a single item. Further research is needed to understand if this study's findings translate to weaker social ties, and whether it holds with a more robust measure of social connectedness that takes into account dimensions of closeness such as having a confidant. We were also unable to examine the effects of social influences on depressive symptoms across non-binary gender identities or in same-sex couples in this study. It will be important to include same-sex couples in future studies to understand the unique context of this type of partnership, but also to help determine whether the gender differences found in different-sex couples hold true or if the finding is more reflective of the social role adopted in the relationship (i.e., gender as a social construct).
The average endorsement of depressive symptoms across men and women in our sample was low. It is possible that the strength of the association with social activities and/or connectedness with close friends may vary among individuals with greater depressive symptom severity, as well as couples from diverse cultures, backgrounds, and environments. Future research is needed to further explore the replication of these associations across samples. Finally, the data used for these analyses are cross sectional and therefore estimated effects are not causal. While social activity and connectedness may offer psychological benefits, having depressive symptoms may also reduce social activity and connectedness. However, given the alignment of these findings with prior research and theory, we feel confident that the estimated effects that resulted from our models will replicate in future studies. Ideally, longitudinal studies will examine our results to more definitively determine the direction of causality.
Strengths and conclusions
This study adds to the literature on the importance of social activity engagement and social connectedness to depressive symptoms among older adults by examining these two distinct social factors simultaneously. This study also extends the findings to the vital context of the marital environment, which previous research has emphasized as necessary to consider when evaluating and treating depression in older adults (17). Lastly, this study takes into account the varying degrees of physical health within and across community-dwelling couples. There are clearly positive implications for the mental health of couples who are able to remain socially active and connected with close friends, and who remain physically healthy together.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: https://octri.ohsu.edu/redcap/surveys/?s=EW4HKW47XH.
Ethics statement
The studies involving human participants were reviewed and approved by Oregon Health and Science University IRB. The patients/participants provided their written informed consent to participate in this study.
Author contributions
LM was primarily responsible for the manuscript writing and performed initial data analysis. JS created R code for the incongruence analysis. LM, JS, C-YW, MG, and KL contributed to the study design and manuscript writing. HD and JK were responsible for data collection, study supervision, and manuscript revisions. All authors contributed to the article and approved the submitted version.
Funding
This work was supported in part by the National Institutes of Health (K01AG059839, P30AG008017, P30AG066518, P30AG024978, R01AG024059, and U2CAG0543701); the Merck Investigator Study Program (55172); and the Veterans Administration (IIR 17-144). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or other funders.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.989182/full#supplementary-material
References
1. Fiske A, Wetherell JL, Gatz M. Depression in older adults. Annu Rev Clin Psychol. (2009) 5:363–89. doi: 10.1146/annurev.clinpsy.032408.153621
2. Hasin DS, Sarvet AL, Meyers JL, Saha TD, Ruan WJ, Stohl M, et al. Epidemiology of adult DSM-5 major depressive disorder and its specifiers in the United States. JAMA Psychiatry. (2018) 75:336–46. doi: 10.1001/jamapsychiatry.2017.4602
3. Ludvigsson M, Marcusson J, Wressle E, Milberg A. Morbidity and mortality in very old individuals with subsyndromal depression: an 8-year prospective study. Int Psychogeriatr. (2019) 31:1569–79. doi: 10.1017/S1041610219001480
4. Meeks TW, Vahia IV, Lavretsky H, Kulkarni G, Jeste DV. A tune in “a minor” can “b major”: a review of epidemiology, illness course, and public health implications of subthreshold depression in older adults. J Affect Disord. (2011) 129:126–42. doi: 10.1016/j.jad.2010.09.015
5. Pietrzak RH, Kinley J, Afifi TO, Enns MW, Fawcett J, Sareen J. Subsyndromal depression in the United States: prevalence, course, and risk for incident psychiatric outcomes. Psychol Med. (2013) 43:1401–14. doi: 10.1017/S0033291712002309
6. Maier A, Riedel-Heller SG, Pabst A, Luppa M. Risk factors and protective factors of depression in older people 65+. A systematic review. PLoS ONE. (2021) 16:e0251326. doi: 10.1371/journal.pone.0251326
7. Chen YC, Putnam M, Lee YS, Morrow-Howell N. Activity patterns and health outcomes in later life: the role of nature of engagement. Gerontologist. (2019) 59:698–708. doi: 10.1093/geront/gny023
8. Hong SI, Hasche L, Bowland S. Structural relationships between social activities and longitudinal trajectories of depression among older adults. Gerontologist. (2009) 49:1–11. doi: 10.1093/geront/gnp006
9. Isaac V, Stewart R, Artero S, Ancelin ML, Ritchie K. Social activity and improvement in depressive symptoms in older people: a prospective community cohort study. Am J Geriatr Psychiatry. (2009) 17:688–96. doi: 10.1097/JGP.0b013e3181a88441
10. Ermer AE, Proulx CM. Social support and well-being among older adult married couples: a dyadic perspective. J Soc Pers Relat. (2019) 37:1073–91. doi: 10.1177/0265407519886350
11. Han SH, Kim K, Burr JA. Friendship and depression among couples in later life: the moderating effects of marital quality. J Gerontol B Psychol Sci Soc Sci. (2019) 74:222–31. doi: 10.1093/geronb/gbx046
12. Taylor HO, Taylor RJ, Nguyen AW, Chatters L. Social isolation, depression, and psychological distress among older adults. J Aging Health. (2018) 30:229–46. doi: 10.1177/0898264316673511
13. Carr D, Utz RL. Families in later life: a decade in review. J Marr Fam. (2020) 82:346–63. doi: 10.1111/jomf.12609
14. Hughes ME, Waite LJ. Marital biography and health at mid-life. J Health Soc Behav. (2009) 50:344–58. doi: 10.1177/002214650905000307
15. Wright MR, Brown SL. Psychological well-being among older adults: the role of partnership status. J Marriage Fam. (2017) 79:833–49. doi: 10.1111/jomf.12375
16. Ayotte BJ, Yang FM, Jones RN. Physical health and depression: a dyadic study of chronic health conditions and depressive symptomatology in older adult couples. J Gerontol B Psychol Sci Soc Sci. (2010) 65:438–48. doi: 10.1093/geronb/gbq033
17. Monin JK, Doyle M, Van Ness PH, Schulz R, Marottoli RA, Birditt K, et al. Longitudinal associations between cognitive functioning and depressive symptoms among older adult spouses in the cardiovascular health study. Am J Geriatr Psychiatry. (2018) 26:1036–46. doi: 10.1016/j.jagp.2018.06.010
18. Monserud MA, Peek MK. Functional limitations and depressive symptoms: a longitudinal analysis of older Mexican American couples. J Gerontol B Psychol Sci Soc Sci. (2014) 69:743–62. doi: 10.1093/geronb/gbu039
19. Rayens MK, Reed DB. Predictors of depressive symptoms in older rural couples: the impact of work, stress and health. J Rural Health. (2014) 30:59–68. doi: 10.1111/jrh.12028
20. Lyons KS, Lee CS. The theory of dyadic illness management. J Fam Nurs. (2018) 24:8–28. doi: 10.1177/1074840717745669
21. Kalmijn M. Shared friendship networks and the life course: an analysis of survey data on married and cohabiting couples. Soc Networks. (2003) 25:231–49. doi: 10.1016/S0378-8733(03)00010-8
23. Cross SE, Madson L. Models of the self: self-construals and gender. Psychol Bull. (1997) 122:5–37. doi: 10.1037/0033-2909.122.1.5
24. Markus H, Kitayama S. Culture and the self: Implications for cognition, emotion, and motivation. Psychol Rev. (1991) 98:224–52. doi: 10.1037/0033-295X.98.2.224
25. Gabriel S, Gardner WL. Are There “His” and “Hers” types of interdependence? The implications of gender differences in collective versus relational interdependence for affect, behavior, and cognition. J Pers Soc Psychol. (1999) 77:642–55. doi: 10.1037/0022-3514.77.3.642
26. Lee HJ, Szinovacz ME. Positive, negative, and ambivalent interactions with family and friends: associations with well-being. J Marr Fam. (2016) 78:660–79. doi: 10.1111/jomf.12302
27. Löckenhoff CE, Carstensen LL. Socioemotional selectivity theory, aging,and health: the increasingly delicate balance between regulating emotions and making tough choices. J Pers. (2004) 72:1395–424. doi: 10.1111/j.1467-6494.2004.00301.x
28. Urry HL, Gross JJ. Emotion regulation in older age. Curr Dir Psychol Sci. (2010) 19:352–7. doi: 10.1177/0963721410388395
29. Ang S. Your friends, my friends, and our family: informal social participation and mental health through the lens of linked lives. Soc Sci Med. (2021) 276:113848. doi: 10.1016/j.socscimed.2021.113848
30. Blieszner R, Ogletree AM, Adams RG. Friendship in later life: a research agenda. Innov Aging. (2019) 3:igz005. doi: 10.1093/geroni/igz005
31. Pinquart M, Sörensen S. Influences on loneliness in older adults: a meta-analysis. Basic Appl Soc Psychol. (2001) 23:245–66. doi: 10.1207/S15324834BASP2304_2
32. Thoits PA. Mechanisms linking social ties and support to physical and mental health. J Health Soc Behav. (2011) 52:145–61. doi: 10.1177/0022146510395592
33. Utz RL, Swenson KL, Caserta M, Lund D, deVries B. Feeling lonely versus being alone: loneliness and social support among recently bereaved persons. J Gerontol B Psychol Sci Soc Sci. (2014) 69:85–94. doi: 10.1093/geronb/gbt075
34. Santini ZI, Koyanagi A, Tyrovolas S, Mason C, Haro JM. The association between social relationships and depression: a systematic review. J Affect Disord. (2015) 175:53–65. doi: 10.1016/j.jad.2014.12.049
35. Hertzog C, Kramer AF, Wilson RS, Lindenberger U. Enrichment effects on adult cognitive development: can the functional capacity of older adults be preserved and enhanced? Psychol Sci Public Interest. (2009) 9:1–65. doi: 10.1111/j.1539-6053.2009.01034.x
36. Fingerman KL, Huo M, Charles ST, Umberson DJ. Variety is the spice of late life: social integration and daily activity. J Gerontol B Psychol Sci Soc Sci. (2020) 75:377–88. doi: 10.1093/geronb/gbz007
37. Beattie Z, Miller LM, Almirola C, Au-Yeung W-TM, Bernard H, Cosgrove KE, et al. The collaborative aging research using technology initiative: an open, sharable, technology-agnostic platform for the research community. Digital Biomark. (2020) 4:100–18. doi: 10.1159/000512208
38. Kaye J, Maxwell SA, Mattek N, Hayes TL, Dodge H, Pavel M, et al. Intelligent systems for assessing aging changes: home-based, unobtrusive, and continuous assessment of aging [Research Support, N.I.H.. Extramural Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, Non-P.H.S.]. J Gerontol B Psychol Sci Soc Sci. (2011) 66(Suppl. 1):i180–190. doi: 10.1093/geronb/gbq095
39. Thomas NWD, Beattie Z, Marcoe J, Wright K, Sharma N, Mattek N, et al. An ecologically valid, longitudinal, and unbiased assessment of treatment efficacy in Alzheimer disease (the EVALUATE-AD Trial): proof-of-concept study. JMIR Res Protoc. (2020) 9:17603. doi: 10.2196/17603
40. Sheikh JI, Yesavage JA. Geriatric depression scale (GDS): recent evidence and development of a shorter version. Clin Gerontol. (1986) 5:165–73. doi: 10.1300/J018v05n01_09
41. Morgan K, Dallosso HM, Ebrahim SBJ. A brief self-report scale for assessing personal engagement in the elderly. In: A. Butler, editor. Ageing: Recent Advances and Creative Responses. London: Croom Helm (1985). p. 298–304.
42. Parmelee PA, Thuras PD, Katz IR, Lawton MP. Validation of the Cumulative Illness Rating Scale in a geriatric residential population [Research Support, U.S. Gov't, P.H.S.]. J Am Geriatr Soc. (1995) 43:130–7. doi: 10.1111/j.1532-5415.1995.tb06377.x
43. Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. (1975) 12:189–98. doi: 10.1016/0022-3956(75)90026-6
44. Melikyan ZA, Malek-Ahmadi M, O'Connor K, Atri A, Kawas CH, Corrada MM. Norms and equivalences for MoCA-30, MoCA-22, and MMSE in the oldest-old. Aging Clin Exp Res. (2021) 33:3303–11. doi: 10.1007/s40520-021-01886-z
45. Roalf DR, Moberg PJ, Xie SX, Wolk DA, Moelter ST, Arnold SE. Comparative accuracies of two common screening instruments for classification of Alzheimer's disease, mild cognitive impairment, and healthy aging. Alzheimers Dement. (2013) 9:529–37. doi: 10.1016/j.jalz.2012.10.001
46. Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I, et al. The montreal cognitive assessment, MoCA: A Brief screening tool for mild cognitive impairment. J Am Geriatr Soc. (2005) 53:695–9. doi: 10.1111/j.1532-5415.2005.53221.x
47. Cook WL, Kenny DA. The actor-partner interdependence model: a model of bidirectional effects in developmental studies. Int J Behav Dev. (2005) 29:101–9. doi: 10.1080/01650250444000405
48. Bentler PM, Bonett DG. Significance tests and goodness-of-fit in the analysis of covariance structures. Psychol Bull. (1980) 88:588–600. doi: 10.1037/0033-2909.88.3.588
49. Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Eq Model Multidiscip J. (1999) 6:1–55. doi: 10.1080/10705519909540118
50. MacCallum RC, Browne MW, Sugawara HM. Power analysis and determination of sample size for covariance structure modeling. Psychol Methods. (1996) 1:130–49. doi: 10.1037/1082-989X.1.2.130
51. Lyons KS, Hutton-Johnson S, Lee CS. The role of symptom appraisal, concealment and social support in optimizing dyadic mental health in heart failure. Aging Mental Health. (2021) 25:734–41. doi: 10.1080/13607863.2020.1711866
52. Lyons KS, Lee CS. Understanding the family care dyad: a comparison of two multilevel models. Eur J Cardiovasc Nurs. (2020) 19:178–84. doi: 10.1177/1474515120902368
53. Thompson L, Walker AJ. The dyad as the unit of analysis: conceptual and methodological issues. J Marriage Fam. (1982) 44:889–900. doi: 10.2307/351453
54. Polenick CA, Birditt KS, Turkelson A, Bugajski BC, Kales HC. Discordant chronic conditions and depressive symptoms: longitudinal associations among middle-aged and older couples. J Gerontol B Psychol Sci Soc Sci. (2021) 76:451–60. doi: 10.1093/geronb/gbz137
55. Antonucci TC, Lansford JE, Akiyama H. Impact of positive and negative aspects of marital relationships and friendships on well-being of older adults. Appl Dev Sci. (2001) 5:68–73. doi: 10.1207/S1532480XADS0502_2
56. Springer KW, Hankivsky O, Bates LM. Gender and health: relational, intersectional, and biosocial approaches. Soc Sci Med. (2012) 74:1661–6. doi: 10.1016/j.socscimed.2012.03.001
57. Lyons KS, Sayer AG. Using multilevel modeling in caregiving research. Aging Ment Health. (2005) 9:189–95. doi: 10.1080/13607860500089831
58. Brauer K, Sendatzki R, Scherrer T, Chick G, Proyer RT. Revisiting adult playfulness and relationship satisfaction: APIM analyses of middle-aged and older couples. Int J Appl Posit Psychol. (2021). doi: 10.1007/s41042-021-00058-8. [Epub ahead of print].
Keywords: social factors, depression, dyadic health, couple (spouses), gender
Citation: Miller LM, Steele JS, Wu C-Y, Kaye J, Dodge HH, Gonzales MM and Lyons KS (2022) Depressive symptoms in older adult couples: Associations with dyadic physical health, social engagement, and close friends. Front. Psychiatry 13:989182. doi: 10.3389/fpsyt.2022.989182
Received: 08 July 2022; Accepted: 24 August 2022;
Published: 13 September 2022.
Edited by:
Serena Sabatini, University of Italian Switzerland, SwitzerlandReviewed by:
Gabriela Cabett Cipolli, State University of Campinas, BrazilRichard Morycz, University of Pittsburgh, United States
Copyright © 2022 Miller, Steele, Wu, Kaye, Dodge, Gonzales and Lyons. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lyndsey M. Miller, millerly@ohsu.edu
 Lyndsey M. Miller
Lyndsey M. Miller Joel S. Steele
Joel S. Steele Chao-Yi Wu
Chao-Yi Wu Jeffrey Kaye
Jeffrey Kaye Hiroko H. Dodge
Hiroko H. Dodge Mitzi M. Gonzales
Mitzi M. Gonzales Karen S. Lyons6
Karen S. Lyons6