- 1Department of Epidemiology and Health Statistics, School of Public Health, Wannan Medical College, Wuhu, China
- 2Department of Oral Medicine, School of Stomatology, Wannan Medical College, Wuhu, China
- 3Department of Hospital Infection Management Office, Wuhu Hospital of Traditional Chinese Medicine, Wuhu, China
- 4School of Humanities and Management, Wannan Medical College, Wuhu, China
Background: The purpose of this study was to assess the mental health status of medical students engaged in online learning at home during the pandemic, and explore the potential risk factors of mental health.
Methods: A cross-sectional study was conducted via an online survey among 5,100 medical students from Wannan Medical College in China. The Depression, Anxiety and Stress scale (DASS-21) was used to measure self-reported symptoms of depression, anxiety, and stress among medical students during online learning in the pandemic.
Results: In total, 4,115 participants were included in the study. The prevalence symptoms of depression, anxiety, and stress were 31.9, 32.9, and 14.6%, respectively. Depression was associated with gender, grade, length of schooling, relationship with father, students' daily online learning time, and students' satisfaction with online learning effects. Anxiety was associated with gender, length of schooling, relationship with father, relationship between parents, students' daily online learning time, and students' satisfaction with online learning effects. Stress was associated with grade, relationship with father, relationship between parents, students' daily online learning time, and students' satisfaction with online learning effects.
Conclusions: Nearly one-third of medical students survived with varying degrees of depression, anxiety, and stress symptoms during online learning of the COVID-19 pandemic. Gender, grade, length of schooling, family environment, and online learning environment play vital roles in medical students' mental health. Families and schools should provide targeted psychological counseling to high-risk students (male, second-year and third-year, four-year program). The findings of this study can provide reference for educators to cope with the psychological problems and formulate the mental health curriculum construction among medical students during online learning.
Introduction
Since December 2019, the coronavirus disease 2019 (COVID-19) has spread rapidly in China and around the world (1). As of April 5, 2020, there were more than 1.20 million diagnosed cases and more than 68,000 deaths in 215 countries and regions around the world (2). The WHO classified COVID-19 as a pandemic on March 11, 2020 (3). As of 24:00, May 31, 2020, a total of 83,001 COVID-19 cases had been confirmed and 4,634 people had died due to COVID-19-related illnesses in China (4).
COVID-19 is a respiratory infectious disease with strong transmission intensity (5). In order to control the spread of the epidemic, strict traffic control has been implemented throughout China, and a large number of university students have been implemented strict self-isolation in their hometowns (6). In order to solve the problem of students unable to study in school, the Department of Education of Anhui Province (China) issued a notice On February 24, 2020: all kinds of schools (universities, middle schools, etc.) in Anhui Province postponed the opening of classes, and implemented the online education on March 2, 2020 (7). In response to the Ministry of Education' s call for “Disrupted classes, undisrupted learning,” teachers have begun to prepare for online learning from mid-February. For the first time, the teaching and learning of all courses has completely changed from offline to online, which is undoubtedly a severe test for college students who are used to classroom learning (8).
As a global public health event, COVID-19 can lead to psychological crises such as acute stress disorder, post-traumatic stress disorder (PTSD), anxiety, and depression (9). Several studies have indicated that the outbreak of infectious diseases causes mental health problems (10–13). After the occurrence of severe acute respiratory syndrome (SARS), the positive detection rate of PTSD in first-line medical workers was 25.8%, while the total score of anxiety and depression of medical students was significantly higher than that of medical workers (14). During the COVID-19 pandemic, the mental health of patients and front-line medical staff has received significant attention (10, 15). Medical students have more academic pressure, and they are at higher risk of mental diseases, such as anxiety and suicidal ideation (16, 17). As a new force in the medical field, medical students have insufficient clinical experience and no opportunity to participate in the front-line anti-epidemic work. Ye et al. reported that medical students were suffering from more stress than non-medical students (18). During the period of home isolation, medical students have reduced social contact and support from peers (6, 19). A systematic review from 100 eligible studies indicated that social support was associated with depression protection, and parental support was the most important among adolescents (20). During the period of home isolation, the COVID-19 pandemic had a negative impact on the mental health of college students (21, 22). For college students who are used to classroom learning, online teaching may have a certain impact on their psychology (23). The study studied by Zhang et al. indicated that the percentage of learning burnout among medical students engaged in online learning was as high as 46.05% (24). The above researches suggests that medical students engaged in online learning during the epidemic might be more prone to develop negative psychological, owning to face the double pressure of the pandemic and online learning.
Therefore, mental health of medical students engaged in online learning should cause concern. This study first investigated the mental health of medical students during online learning after the outbreak of COVID-19 in China, and further examined the potential risk factors of mental health. The results of this study can provide a theoretical basis for psychological intervention for medical students. This study will also strengthen the impact of medical education and provide reference for better creating innovative online teaching strategies among medical students.
Methods
Participants and Procedure
The participants of this study were medical students who participated in online learning in the 2019/2020-2 semester from Wannan Medical College in Anhui Province, China. The school has a total of 15,813 students in the 2019/2020-2 semester, including 18 majors with four-year programs and 7 majors with five-year programs. Different majors include 2–30 classes, with about 25–33 students in each class. Students in grades 4 and 5 participated in their internship and did not need to partake the school's online learning. All students in grades 1–3 (10,923 students) participated in online learning. Using stratified random cluster sampling method, 5,100 students in 170 classes were selected as the participants. The specific implementation method was as follows: (1) Firstly, we stratified the students according to the length of schooling (four-year programs and five-year programs), and then stratified according to the majors; (2) Secondly, 40–50% of classes in each grade (grade 1–3) were randomly selected from different majors; and (3) Finally, the researcher contacted the counselors of each grade in different majors to count the numbers of students in the selected class.
As the students were required to quarantine online learning at home, a web-based survey was distributed through the Wenjuan platform (https://www.wenjuan.com/list/). Before the formal survey, we selected 10 students to conduct an online pre-survey. According to the results of students' feedback, the questionnaire was revised and improved. The formal survey period was from June 1 to June 15, 2020. The counselor sent the online questionnaire to the students via WeChat and QQ. The purpose of the online survey and the precautions for filling in the online questionnaire was told to the students by the counselor. Students were informed that they could participate in the survey voluntarily. The survey took about five min on average to complete. This study was approved by School of Public Health of Wannan Medical College (LL-2020BH2086).
A total of 4,356 online questionnaires surveys were collected. However, 241 participants were excluded from analysis because they took too little time (5–30 s) to complete the questionnaire. Finally, 4,115 respondents were included in the final analysis (80.69% response rate: 4115/5100).
Survey Instrument
The structured questionnaire included the following four aspects: basic information, online learning, family factors, and the mental health of students.
The basic information included gender (male, female), age, grade (first-year, second-year, third-year), length of schooling (four-year program, five-year program), birthplace (city, town, village), father's education level (primary school or below, junior high school, senior high school, junior college, bachelor degree and above), mother's education level (primary school or below, junior high school, senior high school, junior college, bachelor degree and above), the records of students in the class in the past six months (top-grade, middle-grade, bottom-grade).
The online learning-related information included students' daily online learning time (0–2 h, 2–4 h, ≥4 h) and students' satisfaction with online learning effects (satisfied, general, dissatisfied). Family factors included the relationship between parents (good, general, poor), relationship with mother (good, general, poor), and relationship with father (good, general, poor).
The Chinese version of the 21-item Depression Anxiety Stress Scale (DASS-21) was used to measure the mental health of medical students (25). Each item was scored on a 4-point Likert scale from 0 (did not apply to me at all) to 3 (applied to me very much or most of the time). A total of 21-items included three subscales: depression (questions 3, 5, 10, 13, 16, 17, and 21), anxiety (questions 2, 4, 7, 9, 15, 19, and 20), and stress (questions 1, 6, 8, 11, 12, 14, and 18). The three subscales were divided into five levels as follows: depression (normal, 0–9 scores; mild, 10–13 scores; moderate, 14–20 scores; severe, 21–27 scores; extremely severe, 28–42 scores), anxiety (normal, 0–7 scores; mild, 8–9 scores; moderate, 10–14 scores; severe, 15–19 scores; extremely severe, 20–42 scores), and stress (normal, 0–14 scores; mild, 15–18 scores; moderate, 19–25 scores; severe, 26–33 scores; extremely severe, 34–42 scores) (26). The scores of DASS 21 were divided into two groups of normal and symptomatic (mild/moderate/severe/extremely severe). The DASS-21 has good reliability and validity, which has been widely used in college students (27–29). In present study, the Cronbach's α for the depression, anxiety, and stress subscale was 0.896, 0.859, and 0.873, respectively, indicating a good internal consistency for each subscale.
Data Analysis
Data were analyzed using SPSS 26.0 software. Descriptive statistics were performed to reflect the basic characteristics of students using mean (M) and standard deviation (SD) for quantitative data and percentages for qualitative data.
Depression, anxiety, and stress subscale scores were classified as normal and symptomatic (26). A Chi-square test which was used to screen the candidate variables affecting the mental health of medical students was performed to compare the prevalence of symptoms of depression, anxiety, and stress in two (gender, length of schooling) or more groups (grade, birthplace, father's education level, mother's education level, the records of students in the class in the past six months, students' daily online learning time, students' satisfaction with online learning effects, the relationship between parents, relationship with mother, and relationship with father).
The variables with P ≤ 0.1 in the univariate analysis (a Chi-square test) were included in the multivariate regression model: 9 variables for depression (gender, grade, length of schooling, the relationship between parents, relationship with mother, relationship with father, the records of students in the class in the past six months, students' daily online learning time, and students' satisfaction with online learning effects), 8 variables for anxiety (gender, length of schooling, the relationship between parents, relationship with mother, relationship with father, the records of students in the class in the past six months, students' daily online learning time, and students' satisfaction with online learning effects), and 10 variables for stress (gender, grade, length of schooling, father's education level, the relationship between parents, relationship with mother, relationship with father, the records of students in the class in the past six months, students' daily online learning time, and students' satisfaction with online learning effects).
Finally, taking depression, anxiety, and stress (binary dependent variables: normal vs. symptomatic) as dependent variables, the multivariate logistic regression analysis (forward method, 95% confidence interval) was used to explore the potential associated factors of mental health among medical students. A value of P < 0.05 (two-tailed) was considered statistically significant.
Results
Basic Characteristics of Medical Students
Among 4,115 medical students, 1,626 (39.51%) were males, and ages ranged between 17 and 26 years (20.27 ± 1.30 years). 1,328 (32.27%), 1,639 (39.83%), and 1,148 (27.90%) students were from the first, second, and third-year, respectively. In term of length of schooling, five-year and four-year accounted for 56.82% and 43.18%, respectively. More than half (n = 2,105, 51.15%) students were located in village.
Most of students reported that, they had a good relationship with mother (86.56%) and father (74.73%), and their parents had a good relationship (77.47%). With respect to students' daily online learning time, 2,971 (72.20%) students studied for 4 h or more, 794 (19.30%) studied for 2–4 h, and 350 (8.50%) students studied for <2 h. Lower than half of students (36.45%) satisfied with the effect of online teaching, and 48.19% of students were generally satisfied with online teaching. Other basic characteristics was shown in Table 1.
Mental Health of Medical Students Engaged in Online Learning at Home During the Pandemic
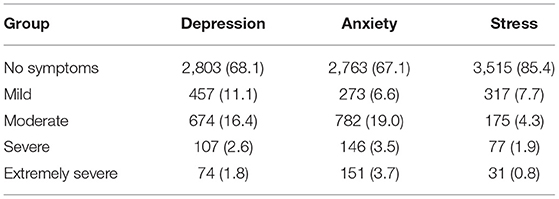
The overall mean score for each of the DASS-21 subscales was 6.66 ± 7.17 for depression symptoms, 5.73 ± 6.34 for anxiety symptoms, and 8.36 ± 7.20 for stress symptoms. 31.9, 32.9, and 14.6% of participants were at symptomatic levels (mild to extremely severe) according to depression (scores ≥10), anxiety (scores ≥8), and stress scores (scores ≥15), respectively.
The prevalence of depression symptoms at mild, moderate, severe, and extremely severe levels were 11.1, 16.4, 2.6, and 1.8%, respectively, and depression symptoms were mainly at moderate level (16.4%). The prevalence of anxiety symptoms at mild, moderate, severe, and extremely severe levels were 6.6, 19.0, 3.5, and 3.7%, respectively, and anxiety symptoms were mainly at moderate level (19.0%). 7.7, 4.3, 1.9, and 0.8% of participants were at mild, moderate, severe, and extremely severe levels, respectively, and stress symptoms were mainly at mild level (7.7%) (Table 2).
Factors Influencing Medical Students' Mental Health During the Pandemic Online Learning at Home
Univariate Analysis
The prevalence of symptoms of depression, anxiety, and stress among males were higher than females (36.59 vs. 28.80%; 38.01 vs. 29.50%; 15.74 vs. 13.82%, respectively) (χ2 = 27.454, 32.344, and 2.921; P < 0.001, P < 0.001, and P = 0.087, respectively). The prevalence of symptoms of depression and anxiety among students whose length of schooling is four-year were higher than those of five-year (34.33 vs. 30.03%; 35.23 vs. 31.05%, respectively) (χ2 = 8.603 and 7.980; P = 0.003 and P = 0.005, respectively) (Table 3).
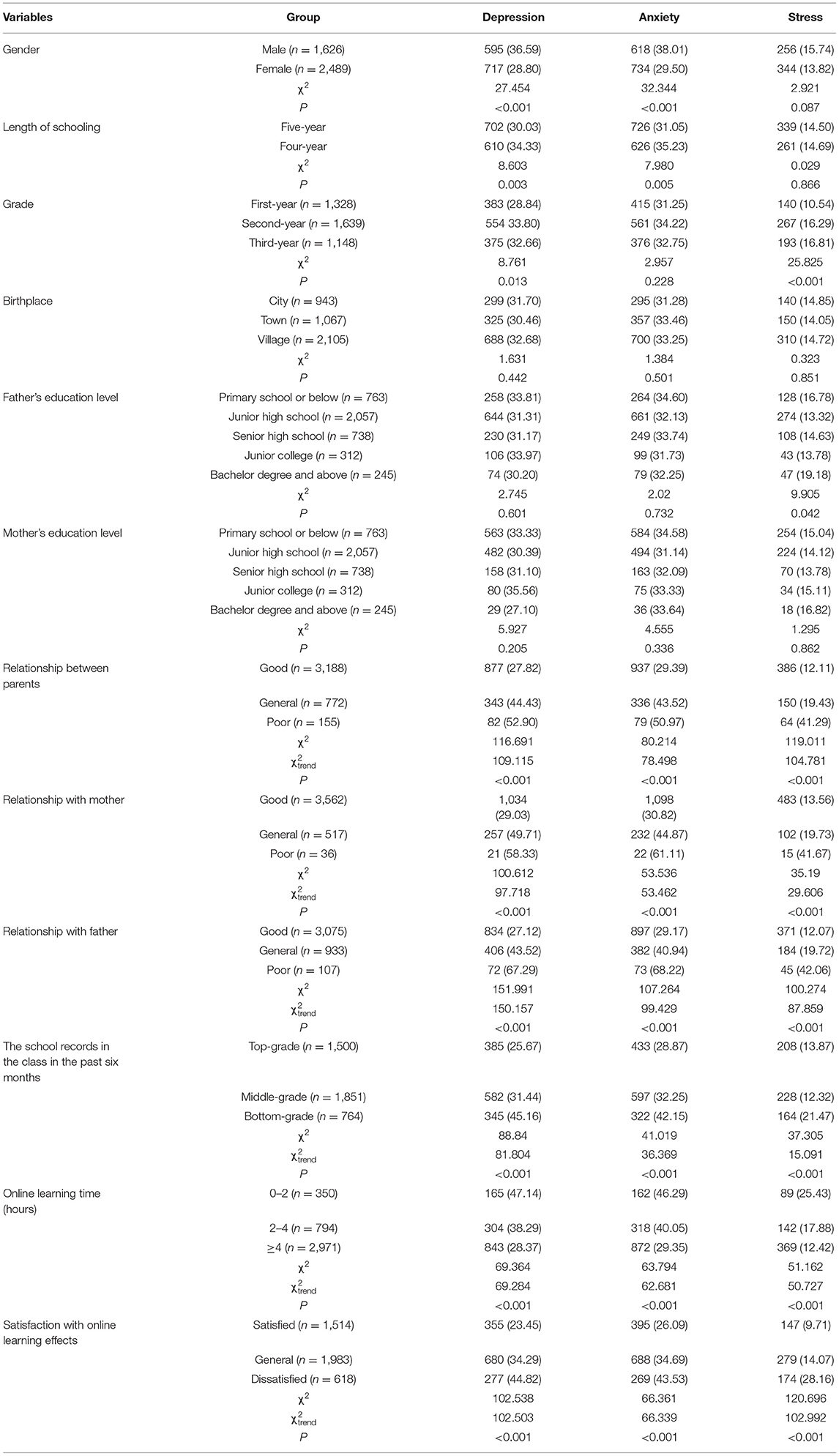
Table 3. Comparison of mental health levels among medical students with different characteristics [n (%)].
The worse the relationship between parents, the relationship with mother, and the relationship with father, the higher the prevalence of symptoms of depression, anxiety, and stress (depression: = 109.115, 97.718, and 150.157; anxiety: = 78.498, 53.462, and 99.429; stress: = 104.781, 29.606, and 87.859; P < 0.001). The prevalence of symptoms of depression, anxiety, and stress was higher in the students with the bottom-grade school records in the past half year, compared with the students with the middle- and the top-grades (P < 0.001) (Table 3).
As students' satisfaction with online teaching decreased, the prevalence of symptoms of depression, anxiety and stress rose ( = 102.503, 66.339, and 102.992; all P < 0.001). The longer the students' online learning time, the lower the prevalence of symptoms of depression, anxiety, and stress ( = 69.284, 62.681, and 50.727; all P < 0.001) (Table 3).
Multivariate Analysis
Variables with P < 0.10 in univariate analysis were included in the multivariate analysis: 9 variables for depression, 8 variables for anxiety, and 10 variables for stress. Taking depression, anxiety, and stress of medical students as dependent variables (0 = No, 1 = Yes), logistic regression analysis was conducted to explore factors associated factors. The risk of depression was significantly increased among medical students with the following variables: males (OR = 1.304, 95% CI: 1.130–1.505), four-year programs (OR = 1.277, 95% CI: 1.105–1.476), grade (second grade: OR = 1.210, 95% CI: 1.021–1.434; third grade: OR = 1.304, 95% CI: 1.081–1.572), relationship with father (poor: OR = 4.706, 95% CI: 3.036–7.296; general: OR = 1.618, 95% CI: 1.339–1.955), the school records in the past six months (bottom: OR = 2.169, 95% CI: 1.784–2.638; middle: OR = 1.301, 95% CI: 1.109–1.526), satisfaction with online learning effects (dissatisfied: OR = 2.308, 95% CI: 1.873–2.844; general: OR = 1.596, 95% CI: 1.365–1.868), and online learning time (0–2 h: OR = 1.779, 95% CI: 1.400–2.259; 2–4 h: OR = 1.398, 95% CI: 1.177–1.660) (Table 4).

Table 4. Wald (forward) logistic regression analyses for factors associated with depression, anxiety, and stress of medical students (n = 4115).
The risk of anxiety was significantly increased among medical students with the following variables: males (OR = 1.421, 95% CI: 1.235–1.634), four-year programs (OR = 1.224, 95% CI: 1.068–1.403), the relationship between parents (general: OR = 1.395, 95% CI: 1.124–1.732), relationship with father (poor: OR = 3.609, 95% CI: 2.252–5.784; general: OR = 1.289, 95% CI: 1.054–1.576), the school records in the past six months (bottom: OR = 1.580, 95% CI: 1.305–1.913), satisfaction with online learning effects (dissatisfied: OR = 1.963, 95% CI: 1.602–2.405; general: OR = 1.422, 95% CI: 1.221–1.655), and online learning time (0–2 h: OR = 1.684, 95% CI: 1.332–2.129; 2–4 h: OR = 1.453, 95% CI: 1.229–1.718) (Table 4).
The risk of stress was significantly increased among medical students with the following variables: grade (second-year: OR = 1.438, 95% CI: 1.143–1.810; third-year: OR = 1.633, 95% CI: 1.279–2.086), the relationship between parents (poor: OR = 3.010, 95% CI: 1.992–4.547), relationship with father (poor: OR = 2.495, 95% CI: 1.507–4.132; general: OR = 1.378, 95% CI: 1.060–1.793), the school records in the past six months (bottom: OR = 1.587, 95% CI: 1.250–2.015), satisfaction with online learning effects (dissatisfied: OR = 3.058, 95% CI: 2.368–3.950; general: OR = 1.405, 95% CI: 1.127–1.750), and online learning time (0–2 h: OR = 1.853, 95% CI: 1.394–2.463; 2–4 h: OR = 1.409, 95% CI: 1.128–1.760) (Table 4).
Discussion
Public health emergencies not only have a direct impact on individual life and social economy, but also may lead to individual psychological stress reaction, which threatens social stability and economic development (30). COVID-19 is a large-scale worldwide disaster in the 21st century. In a US study, depressive symptoms were found to have increased from 8.5% before COVID-19 to 27.8% during the outbreak (31). Evidence from a systematic review and meta-analysis concluded that COVID-19 pandemic had a negative impact on the mental health of the global population, particularly medical workers and quarantined persons (32). A cross-sectional survey among the Iranian population found that compared with community population, medical students had higher scores of stress, anxiety and depression due to lower experience. At the same time, the compulsory measures from face-to-face teaching to completely online teaching have become new challenges for medical students (33). A comprehensive and large-scale study from 62 countries (30,383 students) in the transition to one learning showed that students were mainly concerned their future professional career and studies, and experienced boredom and frustration (34). In order to formulate the targeted psychological interventions, it is essential to focus on the levels and associated factors of mental health among medical students engaged in online learning during the pandemic.
In the present study, the prevalence of depression, anxiety, and stress symptoms among medical students during online learning were 31.9, 32.9, and 14.6%, respectively, which was significantly higher than the prevalence of students during the non-epidemic period in China (35, 36). Our finding is different from a previous study which showed the prevalence of depression and anxiety was 43.77 and 20.60%, respectively, during the COVID-19 pandemic (37). In that study, Patient Health Questionnaire-9 items (PHQ-9) and Self-Rating Anxiety Scale (SAS) which is different from our study were used to measure the mental health of college students, and only three-fifths (59.52%) were medical majors. Due to the difference in education, the negative impact of the COVID-19 pandemic on medical students and non-medical students is different (38). The different mental health levels among college students in different studies might be related to different psychological scales and different types of students (39). As we all know, the severity of the pandemic varies in different countries, which may cause different degrees of negative psychological impact. An online questionnaire survey conducted in April 2020 among university students in Malaysia utilizing the DASS 21 reported that the prevalence of depression, anxiety, and stress were 29.4, 51.3, and 56.5%, respectively, which were significantly different from our study (40). Combined with the above research results, the COVID-19 pandemic had a negative impact on the mental health of college students, especially medical students. It is important to note that 4.4, 7.2, and 2.7% of medical students reported that the symptoms of depression, anxiety, and stress were at severe and extremely severe levels. While college students with severe depression and anxiety symptoms were at increased risk of suicidal behavior (41). The study reported by Aristovnik et al. concluded that online learning students were more likely to interrupt their studies and felt more socially isolated, compared with students receiving traditional education (34). Social isolation and loneliness increased the risk of depression and anxiety (42). This cross-sectional survey was nearing the end of online learning. Students often face more serious pressure at the end of their study, mainly from the pressure of examination (43). Therefore, it is necessary for colleges and universities to pay special attention to the students whose symptoms were at severe and extremely severe levels and carry out targeted psychological interventions to prevent students from committing suicide.
Multi-factor analysis in our study found that the risk of depression and anxiety was significantly increased among males, which was consistent with the findings from previous studies (28, 44, 45) Online learning at home requires greater self-discipline to complete online courses, particularly in the earlier period when students are adapting to the new system (34). Self-regulation and self-management ability are very important in the process of online learning (46). While, the self-management ability of males was lower than that of females (47). Compared with females, males may be less adaptable to online learning. According to a study, males showed higher psychological pressure during online learning (48). This survey was conducted in June, one month before the final exam for medical students. Several studies reported that most of medical students had exam anxiety (43–49). For the above reasons, males are more likely to experienced negative emotions such as anxiety and depression than females engaged in online learning period in the pandemic. Thus, we need to pay special attention to males. Compared with first-year students, second-year and third-year students experienced higher depression and stress, in agreement with other study (50). It may be related to the fact first-year students mainly study general education courses, and senior students mainly study professional basic and education courses, which is much more difficult than general education courses. The transition from pre-clinical to clinical year is a major turning point, resulting in significant changes in students' learning needs and teaching mode (51). Senior students experienced higher symptoms of depression and stress, which may be due to the improper adjustment of basic courses of online learning, resulting in more worry about the final exam. A study from China reported that compared with first-year students, second-year and third-year students were less satisfied with teachers' teaching effectiveness and teaching methods and arrangements (48). The study also found that the risk of depression and anxiety was significantly increased among medical students with four-year school year. The four-year program has short professional years, many types of medical courses, and great difficulty in course learning. At the same time, these difficulties are exacerbated by the unadaptability brought by the sudden online learning. Finally, it has a negative impact on the mental health of medical students. Online learning environment support was critical for relieving the negative impacts of COVID-19 on the psychosocial health among medical students (50). During the special period of online learning, schools should pay attention to psychological counseling and provide crisis-oriented psychological services, especially the following groups of people: males, students with four-year school year, and senior students.
Family is generally considered to be one of the most influential factors in the social and psychological development of adolescents (52, 53). Based on this research, several family variables (relationship with mother, with father, and between parents) seem to be related to the depression, anxiety, and stress symptoms among medical students engaged in online learning period in the pandemic. The parent-child relationship plays a relatively key role in the development of the individual's psychological well-being and the cultivation of a good personality (54). A systematic review from 100 eligible studies indicated that social support was associated with depression protection, and parental support was the most important among adolescents (20). A harmonious parent-child relationship was more conducive to the cultivation of students' positive academic emotions, which was beneficial to their mental health (55). During this special period of online learning in the pandemic, parents, especially fathers, should pay more attention to students' thoughts and be aware of their psychological needs. At the same time, parents should communicate more with their children, so as to reduce students' mental health problems in special periods.
Our findings indicated that the students' daily online learning time was associated with the depression, anxiety, and stress. Medical students who study online 0–2 and 2–4 h a day had higher negative emotions. The short online learning time results in less communication between students and teachers and less communication between students and students (6, 19). A recent study conducted in Switzerland on 236 students indicated that less social contact has a negative psychological impact on students during the COVID-19 pandemic (56). The present study also demonstrated that as students' satisfaction with online learning effects decreased, the prevalence of symptoms of depression, anxiety, and stress were found to rise both in males and females, suggesting that teachers' online learning effects has a significant impact on students' negative emotions. The transition to online learning occurred suddenly, which is a new challenge for both teachers and students (57). In offline teaching, teachers can communicate face-to-face with students, observe students' listening status at any time, and adjust the speed and content of lectures in time according to students' understanding of the course, which ensure the effective transmission of knowledge (58). Students who used to the traditional face-to-face classroom teaching method can not fully accept online teaching in a short time. In a cross-sectional study of 243 medical students found that 22.3% of medical students perceived severe stress as they did not prefer online learning and had difficulties in time management (51). A cross-sectional survey from more than 13 medical schools in Libya showed that most medical students (64.7%) did not think that online learning could be easily implemented during the COVID-19 pandemic (59). An online survey among 7,084 Chinese college students indicated that percentage of psychological pressure among college students who were unfamiliar with the operation of the learning platform (32.9%) were higher than that of students who were proficient (48). Another cross-sectional survey of 99,559 valid samples from 90 medical schools in China revealed that students' satisfaction with their current online education was positively correlated with their previous learning experiences (60). In China, the vast majority of medical students had online learning experience, and 36.84 and 35.00% of students were most familiar with recorded broadcast courses and MOOCs (60). Therefore, teachers should choose the teaching platform familiar to students for online teaching, so as to improve the quality of online medical education. In Chinese medical education, teachers prefer traditional teaching methods, such as face-to-face teaching (60). Online education has attracted global attention, but it is not common in China (61). Therefore, in order to continuously and effectively carry out online medical education and improve students' satisfaction with online learning, schools should provide more support and training in teachers' teaching. Before carrying out online teaching, teachers should master the various functions of online teaching platform. At the same time, for students, schools should provide more training to improve their self-management ability.
Limitations
There are limitations that should be considered when interpreting these findings. First, this study was cross-sectional, unlike a longitudinal design, which cannot explain the causal relationships among the study variables. Second, students completed the questionnaire online, which reduced the the return rate of the questionnaire. In addition, information bias is inevitable, although we explained the purpose and significance of this survey to students before the survey. Third, all information was obtained from a self-reported questionnaire, which may lead to recalling bias and reporting bias. Fourth, during the pandemic period, The Ministry of Education of the People's Republic of China launched a policy called “Disrupted classes, undisrupted learning” to provide online learning in Colleges and universities across the country for the first time. In the whole process of using online teaching in Colleges and universities, there may be differences in school level, students' autonomous learning ability, and implementation scheme. The results of this study come from one medical college, and the extrapolation of the results is not necessarily applicable to non-medical students. A nationwide survey should be conducted to compare several provinces, including urban and rural areas in the future. Meanwhile, the COVID-19 pandemic is still ongoing and online learning is still an important means. Prospective studies should be used to explore the influencing factors of college students' mental health in the future.
Conclusion
In conclusion, during the online learning period in the pandemic, nearly one-third of medical students survived with varying degrees of depression, anxiety, and stress symptoms. Some individual characteristics (gender, grade, length of schooling), family environment (relationship with father, relationship between parents), and online learning environment (students' daily online learning time, and students' satisfaction with online learning effects) play vital roles in medical students' mental health. This study implies that families and schools should pay attention to the negative emotions among medical students engaged in online learning at home during the pandemic, and provide targeted psychological counseling to high-risk students (male, second-year and third-year, four-year program) to alleviate the negative emotions during the pandemic. The findings of this study can provide reference for educators to cope with the psychological problems and formulate the mental health curriculum construction among medical students during online learning.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by School of Public Health of Wannan Medical College (LL-2020BH2086). Written informed consent to participate in this study was provided by the participants' legal guardian/next of kin. Written informed consent was obtained from the minor(s)' legal guardian/next of kin for the publication of any potentially identifiable images or data included in this article.
Author Contributions
W-wC: conceptualization, methodology, investigation, writing-original draft, and supervision. L-xS: methodology, investigation, and writing-original draft. LZ: methodology, investigation, and writing-original draft. J-gY: project administration. Y-lJ: methodology, investigation, resources, and project administration. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by Talent Project of Education Department of Anhui Province (gxfx2017070; gxyqZD2017066), Anhui Province Quality Engineering (2020jyxm2086; 2018JYXM1275; 2015zjjh017), Anhui Province philosophy and social science planning general project (AHSKY2018D55), and Talents Program for Academic Leaders and Reserve Candidates of Wannan Medical College (No. School Administration Letter [2021] No. 46).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors thank all the participating students for their willingness to complete the questionnaires. The authors would also like to thank the editors of this manuscript.
References
1. Bao Y, Sun Y, Meng S, Shi J, Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. (2020) 395:e37–38. doi: 10.1016/S0140-6736(20)30309-3
2. Johns Hopkins University & Medicine. Coronavirus COVID-19 Global Cases by the Center for Systems Science and Engineering at Johns Hopkins. (2020). Available online at: https://coronavirus.jhu.edu/map.html (accessed April 5, 2020).
3. WHO. WHO Director-General's Opening Remarks at the Media Briefifing on COVID-19 - 11 March 2020. World Health Organization. (2020). Available online at: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefifing-on-covid-19-\protect\T1\textdollar-\protect\T1\textdollar11-march-2020 (accessed March 15, 2020).
4. National Health Commission of the People's Republic of China. Update on Novel Coronavirus Pneumonia at 24:00 as at 31st May, 2020. (2020). Available online at: http://www.nhc.gov.cn/xcs/yqtb/202005/230cf04dc30149709ddf4114f81688bf.shtml (accessed July 3, 2021).
5. Gasmi A, Noor S, Tippairote T, Dadar M, Menzel A, Bjørklund G. Individual risk management strategy and potential therapeutic options for the COVID- 19 pandemic. Clin Immunol Jun. (2020) 215:108409. doi: 10.1016/j.clim.2020.108409
6. Deng SQ, Peng HJ. Characteristics of and public health responses to the coronavirus disease 2019 outbreak in China. J Clin Med. (2020) 9:575. doi: 10.3390/jcm9020575
7. China AP,. Department of Education. Important Notice (Notice of education and school teaching line). (2020). Available online at: http://jyt.ah.gov.cn/tsdw/ahsjyxczx/tzgg/39850684.html (accessed March 5, 2020).
8. Khalil R, Mansour AE, Fadda WA, Almisnid K, Aldamegh M, Al-Nafeesah A, et al. The sudden transition to synchronized online learning during the COVID-19 pandemic in Saudi Arabia: a qualitative study exploring medical students' perspectives. BMC Med Educ. (2020) 20:285. doi: 10.1186/s12909-020-02208-z
9. Price M, Legrand AC, Brier ZMF, Gratton J, Skalka C. The short-term dynamics of posttraumatic stress disorder symptoms during the acute posttrauma period. Depress Anxiety. (2020) 37:313–20. doi: 10.1002/da.22976
10. Kang L, Li Y, Hu S, Chen M, Yang C, Yang BX, et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. (2020) 7:e14. doi: 10.1016/S2215-0366(20)30047-X
11. Liem A, Wang C, Wariyanti Y, Latkin CA, Hall BJ. The neglected health of international migrant workers in the COVID-19 epidemic. Lancet Psychiatry. (2020) 7:e20. doi: 10.1016/S2215-0366(20)30076-6
12. Yang Y, Li W, Zhang Q, Zhang L, Cheung T, Xiang YT. Mental health services for older adults in China during the COVID-19 outbreak. Lancet Psychiatry. (2020) 7:e19. doi: 10.1016/S2215-0366(20)30079-1
13. Yuan LL, Lu L, Wang XH, Guo XX, Ren H, Gao YQ, et al. Prevalence and predictors of anxiety and depressive symptoms among international medical students in China during COVID-19 pandemic. Front Psychiatry. (2021) 12:761964. doi: 10.3389/fpsyt.2021.761964
14. Sun Y. Analysis and Follow-Up Study on Related Factors of PTSD in SARS Patients. Taiyuan: Shanxi Medical University (2005).
15. Deng J, Zhou F, Hou W, Silver Z, Wong CY, Chang O, et al. The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: a meta-analysis. Ann N Y Acad Sci. (2021) 1486:90–111. doi: 10.1111/nyas.14506
16. Kötter T, Wagner J, Brüheim L, Voltmer E. Perceived medical school stress of undergraduate medical students predicts academic performance: an observational study. BMC Med Educ. (2017) 17:256. doi: 10.1186/s12909-017-1091-0
17. Quek TT, Tam WW, Tran BX, Zhang M, Zhang Z, Ho CS, et al. The global prevalence of anxiety among medical students: a meta-analysis. Int J Environ Res Public Health. (2019) 16:2735. doi: 10.3390/ijerph16152735
18. Ye W, Ye X, Liu Y, Liu Q, Vafaei S, Gao Y, et al. Effect of the novel coronavirus pneumonia pandemic on medical students' psychological stress and its influencing factors. Front Psychol. (2020) 11:548506. doi: 10.3389/fpsyg.2020.548506
19. Zhou J, Yu H. Contribution of social support to home-quarantined Chinese college students' well-being during the COVID-19 pandemic: the mediating role of online learning self-efficacy and moderating role of anxiety. Soc Psychol Educ. (2021) 25:1–20. doi: 10.1007/s11218-021-09665-4
20. Gariépy G, Honkaniemi H, Quesnel-Vallée A. Social support and protection from depression: systematic review of current findings in Western countries. Br J Psychiatry. (2016) 209:284–93. doi: 10.1192/bjp.bp.115.169094
21. Li Y, Peng J, Tao Y. Relationship between social support, coping strategy against COVID-19, and anxiety among home-quarantined Chinese university students: a path analysis modeling approach. Curr Psychol. (2021) 4:1–16. doi: 10.1007/s12144-021-02334-x
22. Tang W, Hu T, Hu B, Jin C, Wang G, Xie C, et al. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J Affect Disord. (2020) 274:1–7. doi: 10.1016/j.jad.2020.05.009
23. Bolatov AK, Seisembekov TZ, Askarova AZ, Baikanova RK, Smailova DS, Fabbro E. Online-learning due to COVID-19 improved mental health among medical students. Med Sci Educ. (2020) 31:1–10. doi: 10.1007/s40670-020-01165-y
24. Zhang JY, Shu T, Xiang M, Feng ZC. Learning burnout: evaluating the role of social support in medical students. Front Psychol. (2021) 12:625506. doi: 10.3389/fpsyg.2021.625506
25. Gong Y, Xie XY, Xu R, Luo YJ. Psychometric properties of the Chinese versions of DASS-21 in Chinese college students. Chin J Clin Psychol. (2010) 18:443–6. doi: 10.16128/j.cnki.1005-3611.2010.04.020
26. Lovibond SH, Lovibond PF. Manual for the depression anxiety stress scales. Sydney, New South Wales: Psychology Foundation. (1995). doi: 10.1037/t01004-000
27. Wang K, Shi HS, Geng FL, Zou LQ, Tan SP, Wang Y, et al. Cross-cultural validation of the depression anxiety stress scale-21 in China. Psychol Assess. (2016) 28:e88–100. doi: 10.1037/pas0000207
28. Alam MD, Lu J, Ni L, Hu S, Xu Y. Psychological outcomes and associated factors among the international students living in china during the COVID-19 pandemic. Front Psychiatry. (2021) 12:707342. doi: 10.3389/fpsyt.2021.707342
29. Gu S, He Z, Sun L, Jiang Y, Xu M, Feng G, et al. Effects of coronavirus-19 induced loneliness on mental health: sleep quality and intolerance for uncertainty as mediators. Front Psychiatry. (2021) 12:738003. doi: 10.3389/fpsyt.2021.738003
30. Barello S, Graffigna G. Caring for health professionals in the COVID-19 pandemic emergency: toward an “epidemic of empathy” in healthcare. Front Psychol. (2020) 11:1431. doi: 10.3389/fpsyg.2020.01431
31. Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw Open. (2020) 3:e2019686. doi: 10.1001/jamanetworkopen.2020.19686
32. Wu T, Jia X, Shi H, Niu J, Yin X, Xie J, et al. Prevalence of mental health problems during the COVID-19 pandemic: a systematic review and meta-analysis. J Affect Disord. (2021) 281:91–8. doi: 10.1016/j.jad.2020.11.117
33. Vahedian-Azimi A, Moayed MS, Rahimibashar F, Shojaei S, Ashtari S, Pourhoseingholi MA. Comparison of the severity of psychological distress among four groups of an Iranian population regarding COVID-19 pandemic. BMC Psychiatry. (2020) 20:402. doi: 10.1186/s12888-020-02804-9
34. Aristovnik A, KerŽič D, Ravšelj D, TomaŽevič N, Umek L. Impacts of the COVID-19 pandemic on life of higher education students: a global perspective. Sustainability. (2020) 12:8438. doi: 10.3390/su12208438
35. Cheung DK, Tam DKY, Tsang MH, Zhang DLW, Lit DSW. Depression, anxiety and stress in different subgroups of first-year university students from 4-year cohort data. J Affect Disord. (2020) 274:305–14. doi: 10.1016/j.jad.2020.05.041
36. Zou P, Sun L, Yang W, Zeng Y, Chen Q, Yang H, et al. Associations between negative life events and anxiety, depressive, and stress symptoms: a cross-sectional study among Chinese male senior college students. Psychiatry Res. (2018) 270:26–33. doi: 10.1016/j.psychres.2018.09.019
37. Zhan H, Zheng C, Zhang X, Yang M, Zhang L, Jia X. Chinese college students' stress and anxiety levels under COVID-19. Front Psychiatry. (2021) 12:615390. doi: 10.3389/fpsyt.2021.615390
38. Xie L, Luo H, Li M, Ge W, Xing B, Miao Q. The immediate psychological effects of coronavirus disease 2019 on medical and non-medical students in China. Int J Public Health. (2020) 65:1445–53. doi: 10.1007/s00038-020-01475-3
39. Luo W, Zhong BL, Chiu HF. Prevalence of depressive symptoms among Chinese university students amid the COVID-19 pandemic: a systematic review and meta-analysis. Epidemiol Psychiatr Sci. (2021) 30:e31. doi: 10.1017/S2045796021000202
40. Moy FM, Ng YH. Perception towards E-learning and COVID-19 on the mental health status of university students in Malaysia. Sci Prog. (2021) 104:368504211029812. doi: 10.1177/00368504211029812
41. Guo L, Wang W, Wang T, Li W, Gong M, Zhang S, et al. Association of emotional and behavioral problems with single and multiple suicide attempts among Chinese adolescents: modulated by academic performance. J Affect Disord. (2019) 258:25–32. doi: 10.1016/j.jad.2019.07.085
42. Loades ME, Chatburn E, Higson-Sweeney N, Reynolds S, Shafran R, Brigden A, et al. Rapid systematic review: the impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J Am Acad Child Adolesc Psychiatry. (2020) 59:1218–39.e3. doi: 10.1016/j.jaac.2020.05.009
43. Wang LC, Li X, Chung KKH. Relationships between test anxiety and metacognition in Chinese young adults with and without specific learning disabilities. Ann Dyslexia. (2021) 71:103–26. doi: 10.1007/s11881-021-00218-0
44. Wang C, Zhao H. The impact of COVID-19 on anxiety in Chinese university students. Front Psychol. (2020) 11:1168. doi: 10.3389/fpsyg.2020.01168
45. Khan AH, Sultana MS, Hossain S, Hasan MT, Ahmed HU, Sikder MT. The impact of COVID-19 pandemic on mental health & wellbeing among home-quarantined Bangladeshi students: a cross-sectional pilot study. J Affect Disord. (2020) 277:121–8. doi: 10.1016/j.jad.2020.07.135
46. Alt D, Naamati-Schneider L. Health management students' self-regulation and digital concept mapping in online learning environments. BMC Med Educ. (2021) 21:110. doi: 10.1186/s12909-021-02542-w
47. Xu ZY, Li MJ. Influencing factors of undergraduate nursing students' autonomous learning ability. J Nurs Sci. (2019) 34:12–5. doi: 10.1186/s12913-016-1423-5
48. Yu L, Huang L, Tang HR, Li N, Rao TT, Hu D, et al. Analysis of factors influencing the network teaching effect of college students in a medical school during the COVID-19 epidemic. BMC Med Educ. (2021) 21:397. doi: 10.1186/s12909-021-02825-2
49. Khoshhal KI, Khairy GA, Guraya SY, Guraya SS. Exam anxiety in the undergraduate medical students of Taibah University. Med Teach. (2017) 39:S22–6. doi: 10.1080/0142159X.2016.1254749
50. Wang J, Liu W, Zhang Y, Xie S, Yang B. Perceived stress among Chinese medical students engaging in online learning in light of COVID-19. Psychol Res Behav Manag. (2021) 14:549–62. doi: 10.2147/PRBM.S308497
51. Abdulghani HM, Sattar K, Ahmad T, Akram A. Association of COVID-19 pandemic with undergraduate medical students' perceived stress and coping. Psychol Res Behav Manag. (2020) 13:871–81. doi: 10.2147/PRBM.S276938
52. Bryant RA, Edwards B, Creamer M, O'Donnell M, Forbes D, Felmingham KL, et al. The effect of post-traumatic stress disorder on refugees' parenting and their children's mental health: a cohort study. Lancet Public Health. (2018) 3:e249–58. doi: 10.1016/S2468-2667(18)30051-3
53. Tang S, Xiang M, Cheung T, Xiang YT. Mental health and its correlates among children and adolescents during COVID-19 school closure: the importance of parent-child discussion. J Affect Disord. (2021) 279:353–60. doi: 10.1016/j.jad.2020.10.016
54. Hong W, Liu RD, Ding Y, Oei TP, Zhen R, et al. Parents' phubbing and problematic mobile phone use: the roles of the parent-child relationship and children's self-esteem. Cyberpsychol Behav Soc Netw. (2019) 22:779–86. doi: 10.1089/cyber.2019.0179
55. Leadbitter K Macdonald W Taylor C Buckle KL; the PACT Consortium*. Parent perceptions of participation in a parent-mediated communication-focussed intervention with their young child with autism spectrum disorder. Autism. (2020) 24:2129–41. doi: 10.1177/1362361320936394
56. Elmer T, Mepham K, Stadtfeld C. Students under lockdown: comparisons of students' social networks and mental health before and during the COVID-19 crisis in Switzerland. PLoS ONE. (2020) 15:e0236337. doi: 10.1371/journal.pone.0236337
57. Beniczky S, Blümcke I, Rampp S, Shisler P, Biesel E, Wiebe S. e-learning comes of age: web-based education provided by the international league against epilepsy. Epileptic Disord. (2020) 22:237–44. doi: 10.1684/epd.2020.1157
58. Yusoff MSB, Hadie SNH, Mohamad I, Draman N, Muhd Al-Aarifin I, Wan Abdul Rahman WF, et al. Sustainable medical teaching and learning during the COVID-19 pandemic: surviving the new normal. Malays J Med Sci. (2020) 27:137–42. doi: 10.21315/mjms2020.27.3.14
59. Alsoufi A, Alsuyihili A, Msherghi A, Elhadi A, Atiyah H, Ashini A, et al. Impact of the COVID-19 pandemic on medical education: medical students' knowledge, attitudes, and practices regarding electronic learning. PLoS ONE. (2020) 15:e0242905. doi: 10.1371/journal.pone.0242905
60. Wang C, Xie A, Wang W, Wu H. Association between medical students' prior experiences and perceptions of formal online education developed in response to COVID-19: a cross-sectional study in China. BMJ Open. (2020) 10:e041886. doi: 10.1136/bmjopen-2020-041886
Keywords: COVID-19, depression, anxiety, stress, online learning, medical students
Citation: Chang W-w, Shi L-x, Zhang L, Jin Y-l and Yu J-g (2021) The Mental Health Status and Associated Factors Among Medical Students Engaged in Online Learning at Home During the Pandemic: A Cross-Sectional Study From China. Front. Psychiatry 12:755503. doi: 10.3389/fpsyt.2021.755503
Received: 09 August 2021; Accepted: 06 December 2021;
Published: 23 December 2021.
Edited by:
Khalid Hussain, University of the Punjab, PakistanReviewed by:
Mochammad Fahlevi, Binus University, IndonesiaCopyright © 2021 Chang, Shi, Zhang, Jin and Yu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jie-gen Yu, whyujg@163.com; Yue-long Jin, jinyl0803@wnmc.edu.cn
†These authors have contributed equally to this work
 Wei-wei Chang
Wei-wei Chang Liu-xia Shi2†
Liu-xia Shi2† Yue-long Jin
Yue-long Jin