Corrigendum: Problematic Use of Alcohol and Online Gaming as Coping Strategies During the COVID-19 Pandemic: A Mini Review
- 1Medical Research Center, Hainan Cancer Hospital, Haikou, China
- 2Institute of Human Behavioral Medicine, Medical Research Center, Seoul National University, Seoul, South Korea
- 3Biomedical Research Institute, Seoul National University Hospital, Seoul, South Korea
- 4Department of Psychiatry, SMG-SNU Boramae Medical Center, Seoul, South Korea
- 5Department of Psychiatry and Behavioral Science, Seoul National University College of Medicine, Seoul, South Korea
- 6Emotion, Cognition and Behavior Research Group, Korea Brain Research Institute, Daegu, South Korea
- 7Department of Brain and Cognitive Sciences, Daegu Gyeongbuk Institute of Science and Technology, Daegu, South Korea
The COVID-19 (coronavirus disease 2019) pandemic has dramatically changed our daily lives and activities, including those originally intended to serve for leisure and pleasure. Drinking and online gaming became coping behaviors used to rescue ourselves from the stress and restricted lifestyle during the COVID-19 pandemic. However, frequent drinking and gaming can result in the pathological consequences of addiction. Those affected use the stimuli not to obtain pleasure, but rather to avoid the displeasure induced by stress and previous use, often unsuccessfully. This review aims to provide an overview of recent longitudinal cohort studies on alcohol and gaming use during the COVID-19 pandemic, as well as to analyze how the pandemic has affected alcohol and gaming use. There was a substantial risk of alcohol and online gaming overuse during the lockdown, which may depend on the pandemic's duration or overuse patterns. Previous studies have shown that increased alcohol consumption and online gaming are associated with heightened stress and anxiety levels caused by social isolation/quarantine. Over time, frequent or excessive alcohol consumption and gaming could lead to an increased risk of more serious mental health problems. Every effort should be made to mitigate mental health problems and ensure adequate adaptation to these exceptional circumstances. Therefore, it would be helpful to encourage physical activity, social interaction, and collaboration to facilitate psychological and physical health.
Introduction
The coronavirus (COVID-19) pandemic has caused unprecedented disruptions in the 21st century. Since this pandemic outbreak in 2019, our lives have radically changed, with serious consequences in terms of health, economy, and psychosocial perspectives. In response to the problems posed by the pandemic, governments have taken some emergency measures, including lockdown, restricting traffic, and closing down guilds and shops, which resulted in widespread depression, anxiety, and other adverse psychological reactions (1–5). Isolated and quarantined people frequently turn to substances (e.g., alcohol consumption) or rewarded behaviors (e.g., online gaming) to cope with their negative feelings (5, 6). Previous studies have reported that the impact of disasters, such as traumatic events (i.e., terrorism as 9/11), epidemic outbreaks (i.e., severe acute respiratory syndrome [SARS] in 2003), economic crises (2008's Great Recession), have resulted in increased rates of addictive behaviors, including alcohol drinking and problematic Internet use (7–9).
The pandemic is stressful in multiple aspects, and this stress may trigger increased alcohol intake in susceptible individuals (10, 11), leading to harmful neuroadaptations that further exacerbate alcohol craving. The use of rewarded behaviors/actions (e.g., online gaming) as putative coping strategies can also increase considerably in crises like the COVID-19 pandemic, and can develop into habits that are difficult to break (12).
Thus, the possible adverse effects of the COVID-19 pandemic on substance use and addictive behavior need to be carefully monitored. However, longitudinal research about alcohol/game use before and during the COVID-19 pandemic remain too scarce to elucidate risk factors associated with alcohol-/gaming-related problems observed over time. This narrative review discusses how the lockdown and quarantine by the COVID-19 pandemic affects addictive behaviors and associates negative consequences, focusing on up-to-date longitudinal cohort studies. This investigation would serve as a preliminary step for preventive measures against the mental health problems posed by COVID-19.
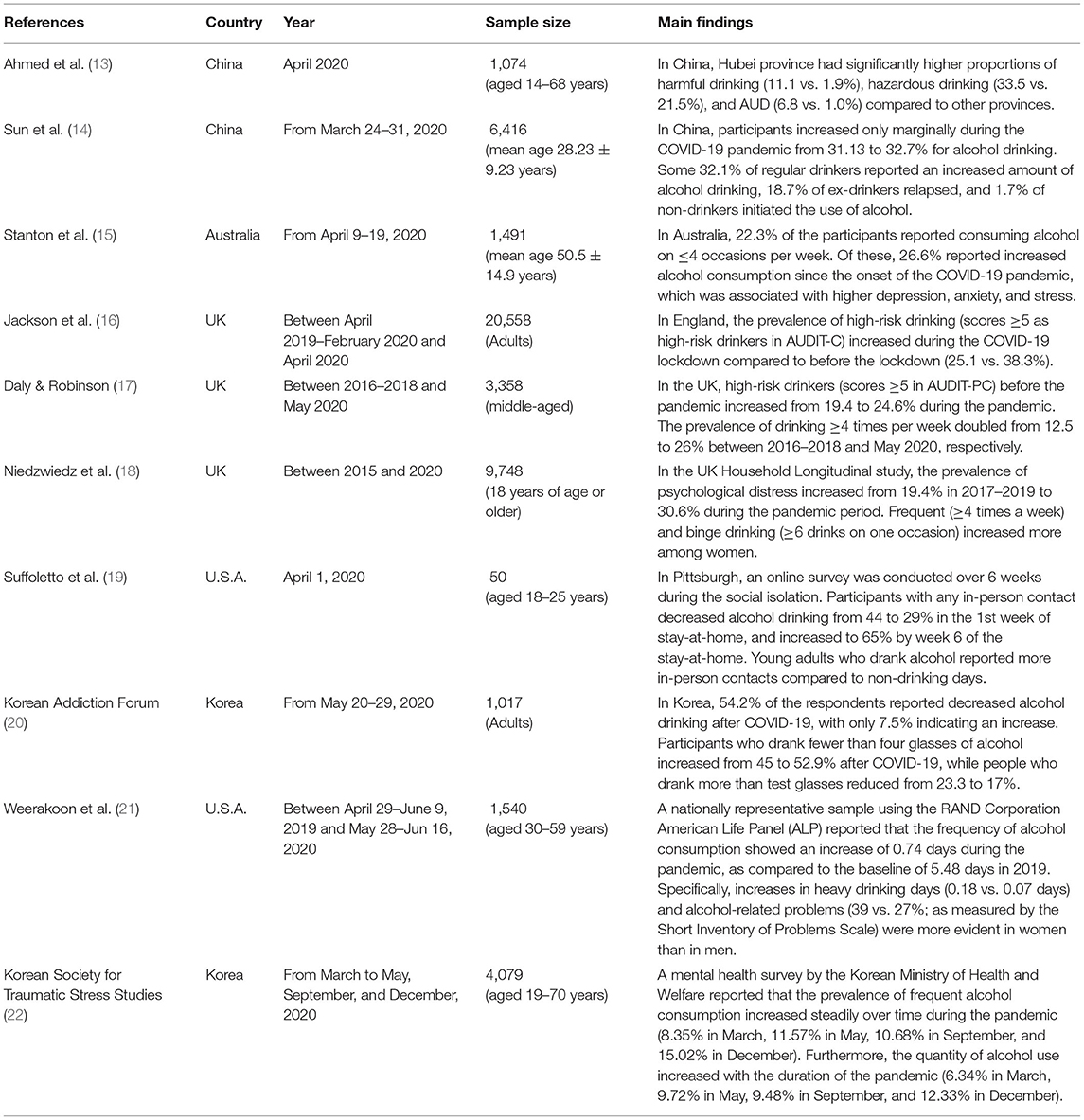
Problematic Alcohol Consumption During the COVID-19 Pandemic
Several studies conducted using self-report measures during the early period of the COVID-19 pandemic have reported increased alcohol consumption during the COVID-19 pandemic, as summarized in Table 1. In an online survey of 1,074 Chinese participants, people in Hubei province (initial epicenter of the COVID-19 pandemic) showed an increased risk of harmful (11.1 vs. 1.9%) and hazardous alcohol use (33.5 vs. 21.5%), compared to people in other provinces after the COVID-19 outbreak (13), as measured by the Alcohol Use Disorders Identification Test (AUDIT) (23). In an online survey of 6,416 Chinese participants, almost one in five ex-drinkers relapsed, and 1.6% initiated alcohol abuse (14). Consistently, another online survey of 1,491 participants in Australia found that 26.6% of the respondents reported an increase in their alcohol consumption, which was mainly associated with higher levels of stress, anxiety, and depression symptoms (15). Although difficult to generalize (24), the findings of these online surveys with self-selected samples suggest that pandemic-related restrictions can be associated with higher drinking behavior.
More recent studies using cross-sectional analyses with longitudinal cohorts have corroborated the adverse effects of the COVID-19 pandemic on alcohol drinking in the general population (see summary in Table 1). Monthly cross-sectional surveys of a representative sample of adult population in the UK (20,558 participants aged 16 years and above) found that the prevalence of high-risk drinking (AUDIT score ≥5) increased from 25.1% before the lockdown (April 2019–February 2020) to 38.3% during the lockdown (April 2020) (16). Another UK study, using data from the 1970 British Cohort Study (3,358 participants), a prospective cohort study of 17,000 children born in Britain in 1970, showed increases in high-risk drinking from 19.4 to 24.6% (in primary care settings, AUDIT score ≥5) and frequent drinking from 12.5 to 26% (prevalence of drinking ≥4 times a week) among middle-aged adults between 2016–2018 and May 2020 (17).
These detrimental effects of the COVID-19 crisis and its associated lockdown restrictions on drinking patterns (e.g., high-risk drinking, binge drinking, frequent drinking, etc.) are likely to be more pronounced among women. A study in the US with 1,540 members of the RAND Corporation American Life Panel (ALP), a nationally representative, probability-sampled panel of 6,000 participants (aged 18 years and above) found that increased heavy drinking, defined as having more than five (man) or four (woman) alcoholic drinks within a couple of hours, was more pronounced among women than men in May–June 2020 compared to April–June 2019. Consistently, women were more likely than men to have increased alcohol-related problems as measured by the Short Inventory of Problems scale (25). Furthermore, analyses of data between 2015 and 2020 from the UK Household Longitudinal Study, a nationally representative longitudinal panel study based on a clustered-stratified probability sample of UK households (9,748 participants aged 18 years and above), revealed that the COVID-19 lockdown (April 2020) increased frequent (≥4 times a week) and binge drinking (≥6 drinks on one occasion) particularly among women (18). The gender difference in alcohol consumption can be associated with the lifestyle and stress management during the pandemic. Life stressors, such as quarantine and social isolation, which are associated with anxiety and depression (26, 27), lead to an unhealthy lifestyle such as unhealthy diet, high-risk drinking, etc. (26, 28). Reportedly, quarantine led to weight gain and an increased incidence of depression and stress among women more than men (29). Additionally, the aforementioned UK household analysis showed that psychological distress, as assessed by the General Health Questionnaire-12 after the 1st month of lockdown, together with adverse alcohol use increased significantly among women (18). These gender differences may be explained by biophysiological mechanisms that enhance women's vulnerability to negative emotions and stress responses (30). Consequently, women tend to experience higher alcohol-related health problems than men, especially when women are heavy drinkers (31, 32). This reflects international trends indicating that the prevalence of alcohol-related harms is escalating among women (33).
Besides social isolation, other environmental factors have also been associated with distress and alcohol use during the COVID-19 pandemic. For instance, boredom and monotony are a hotbed for numerous psychological challenges. Struk et al. (34) found that feeling bored is a motive behind rule-breaking behaviors that can affect compliance with social distancing policies. A preliminary study in the US showed that young adults' (aged 18–25 years) non-adherence to social distancing policies is associated with hazardous alcohol drinking (19). On the other hand, most people following strict restriction policies and lockdowns have suffered from the disruption of their daily routines. In the absence of external cues such as office hours, they have difficulties in discriminating the periods that should be dedicated for work, leisure, or household tasks. Their circadian rhythm gets disrupted, leading to negative affect and stress (35, 36), which can induce significant alcohol use and craving (37). Furthermore, alcohol works as a self-medication for depression (38). However, the positive affect induced by alcohol use does not last long, while the negative consequences become prominent, including various drinking-related problems and exacerbated depression (39–41). Following a daily routine, engaging in regular physical activity, and improving coping skills are some protective factors for drinking behavior (42).
In South Korea, a preliminary survey of 1,017 participants showed that a majority (61.9%) of pre-pandemic heavy/frequent drinkers (≥4 times a week) showed increased alcohol consumption during the outbreak, while a majority of former moderate (64.7%), light (70.9%), or non-drinkers (55.8%) (≤3 times a week) showed decreased alcohol consumption (20). Similarly, an online survey conducted by the Norwegian Directorate of Health in June–July 2020 with 1,328 respondents (aged 18 years and above) selected randomly from a national web panel reported that the upper 5–10% of heavy drinkers (≥~8.8 drinks a week) during the COVID pandemic increased their alcohol consumption, thereby increasing the prevalence of heavy drinkers (43). Additionally, a European online survey (40,064 participants aged 18 years and older) in 21 European countries showed an increase of harmful alcohol consumption (AUDIT-C score ≥8), but not in low harmful alcohol consumption (AUDIT-C score ≤7) (44). Alcohol cravings among heavy/frequent drinkers can be further exacerbated over time during the quarantine. A study in the US with 5,931 participants recruited via an online crowdsourcing platform (45) showed notable increase in harmful alcohol use (AUDIT-C score ≥8) among those under lockdown over the 6 months of the 2020 COVID-19 pandemic. However, it was essentially unchanged for those not under restrictions (46). Noticeably, an online survey of 1,982 participants in the US reported that the duration spent at home during the COVID-19 pandemic was associated with odds of binge drinking (21), defined as having more than five (man) or four (woman) drinks on one occasion (47). Similarly, a mental health survey by the Korean Ministry of Health and Welfare recently reported that the frequency of alcohol use by heavy/frequent drinkers increased over time during the lockdown (22). These preliminary data should be treated with caution; however, they suggest detrimental effects of prolonged quarantine on alcohol use. It is crucial to monitor potential long-term changes in drinking habits over time during the COVID-19 pandemic.
Problematic Online Gaming Use During the COVID-19 Pandemic
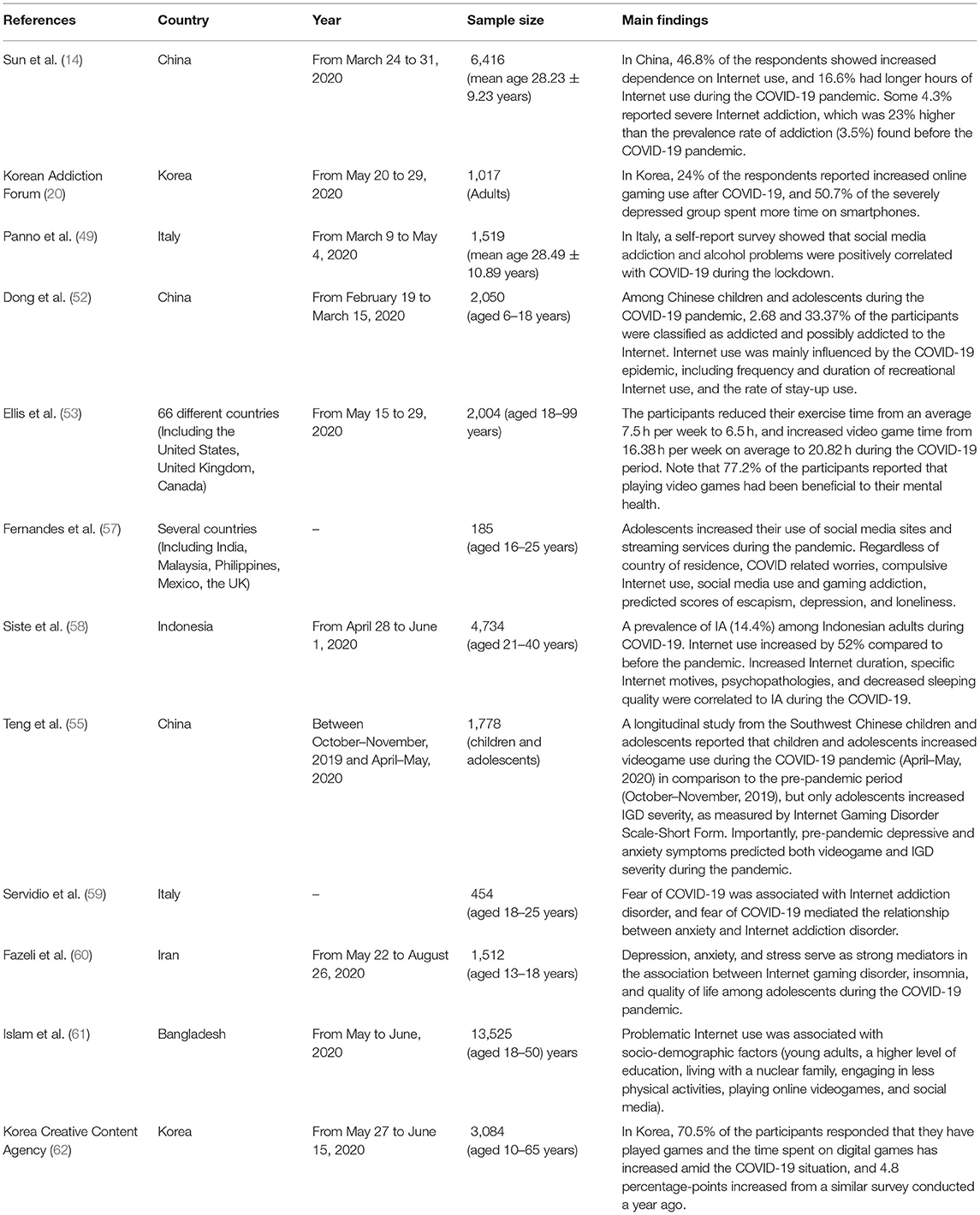
Online gaming and Internet use are also frequently employed as putative coping strategies to reduce the adverse effects of prolonged isolation and loneliness (48–50). Adequate online gaming activities to reduce negative feelings and communicate with others can benefit an individual's mental health (51, 52). According to an Australian survey, only 2.1% of the 2,004 participants reported negative consequences of video games, while 77.2% of the participants indicated that video games had a positive mental health impact, and that games have the potential to promote mental health and provide opportunities to interact with friends through online platforms (53).
However, excessive and uncontrollable online gaming may lead to serious psychological and neurophysiological functions (54). Studies related to problematic Internet use and online gaming use during COVID-19 have been reported (51, 55, 56), which were summarized in Table 2. In China, one survey reported that 46.8% of the 6,416 participants [aged 28.2 ± 9.2 (mean ± SD) years] showed increased scores on the Internet Addiction Test (IAT) (14, 63). Of the participants, 4.3% showed severe internet dependence (80 ≤ IAT score ≤ 100), which is 23% of increase in the prevalence compared to the pre-pandemic period (October 2019). Another survey with 2,050 Chinese adolescents (aged 12.3 ± 4.7 years) during the COVID-19 showed that 2.7 and 33.4% of them were classified as addictive Internet users (IAT score ≥70) and problematic Internet users (40 ≤ IAT score ≤ 69), respectively. Notably, the IAT scores were significantly associated with depression and stress (52). Fernandes et al. (57) reported that 185 adolescents (aged 21.6 ± 2.6 years) from several countries (e.g., India, Malaysia, Mexico, and the UK) have shown increased Internet use and high scores of gaming addiction, which is contributed to loneliness and depression. Indonesia's nationwide web-based study with 4,734 adults (aged 31.8 ± 7.7 years) found that the prevalence of Internet addiction during the COVID-19 crisis was 14.4% in adults, higher than before the pandemic. This study also identified that duration of Internet use, psychopathologies, and decreased sleep quality were predictable factors of Internet addiction during self-quarantine, especially in individuals with confirmed/suspected COVID-19 cases within households (58). Most recent longitudinal study with 1,778 members the Project of School Mental Health in Southwest corroborated that videogame use and Internet Gaming Disorder (IGD) were significantly increased during the COVID-19 (April–May 2020) compared to before the pandemic (October–November 2019). Notably, the results from this study suggested that depressive and anxiety symptoms at pre-pandemic period positively predicted videogame use and IGD during the COVID-19 (55).
A number of studies have confirmed the association between behavioral disorders (i.e., IGD, Internet addiction, and gambling disorder) and psychological factors such as depression, anxiety, and stress (56, 64). An Italian study revealed that fear of COVID-19 was associated with Internet addiction disorder, and fear of COVID-19 mediated the relationship between anxiety and Internet addiction disorder (59). A Chinese study reported that the levels of depression and stress were associated with severity of Internet addiction measured by IAT scores in children and adolescents during COVID-19 (52). An Iranian study demonstrated that psychological factors such as depression, anxiety, and stress significantly mediated the association between Internet gaming disorder and outcomes of insomnia and quality of life among adolescents (60). In addition, a large-scale study in Bangladesh reported that problematic Internet use during COVID-19 was associated with socio-demographic factors (age, educational qualifications, marital status, socioeconomic status) and lifestyle factors (smoking status and sleeping hours) (61).
Additionally, a preliminary nationwide survey of 1,017 participants by the Korean Addiction Forum (KAF) in South Korea, which was conducted between May 20 and 29, 2020, reported that ~24.4% of the respondents said they spent more time on online games after the COVID-19 pandemic (compared to 16.3% who spent less time on online games) (20). Of the respondents, 44.3% said that their smartphone use also increased. They normally use smartphones for communication and social networking. Furthermore, a later online survey (May–June 2020), conducted on 3,084 people aged from 10 to 65 by the Korea Creative Content Agency, showed that 70.5% of the respondents had played digital games since June 2019, with a 4.8% increase compared to the previous survey conducted a year ago (62). In terms of platform, gaming on mobile devices was the most popular means of gaming, accounting for 91.1%, followed by PC games (59.1%), and video game consoles (20.8%).
Discussion
Preliminary studies indicated that increased alcohol consumption as a coping strategy could be associated with social isolation, boredom, and lack of a routine. However, heavy/frequent drinking was not associated with coping motives, but it was associated with greater alcohol problems (65, 66), underscoring the importance of monitoring solitary drinkers as they may be more vulnerable to negative consequences.
Nonetheless, some limitations in the present study regarding alcohol consumption, alcohol-related problems, and Internet gaming disorders should be considered. A majority of the literature we reviewed may lack superior quality because a pandemic encourages a rapid rather than a meticulous spread of information. Many studies utilized non-standardized self-selected samples. It has been more than a year since the outbreak of the pandemic. During this period, numerous papers pertaining to the psychological and behavioral effects of the pandemic have been produced hurriedly. The academic society has had insufficient time to perform systematized and comprehensive researches. However, it is time to summarize these results to obtain a comprehensive view on this subject.
A further concern is that if some individuals may develop, increase, or relapse into unhealthy patterns of gaming to relieve pandemic-related stress, self-isolation restrictions may inhibit help-seeking, while also presenting barriers for those in treatment. For this reason, we encourage the exploration of online/telehealth options, including those that promote social connections (67). It may also be important to make recommendations about the types of videogames that may better facilitate psychological and physical health, including those that encourage physical activity, social interaction, and collaboration.
In response to the COVID-19 pandemic, experts in the field of addictive disorders worldwide have published consensus guidelines for preventing problematic Internet use (48). Although Internet and online gaming use can be an adaptive coping strategy to reduce pandemic-related psychological problems for the majority, it can pose a potential risk to vulnerable people who are at high risk of developing problematic usage patterns (68). Excessive engagement in online gaming and Internet activities may contribute to serious functional impairment and a higher risk of developing addictive disorders during prolonged quarantine periods. Therefore, it is essential to maintain a moderate and controlled level of these behaviors through a well-balanced daily routine, especially during the COVID-19 crisis (69). Several studies have pointed out that various factors, including high levels of stress, depression, anxiety, and fear of COVID-19, are associated with problematic online game use, and coping strategies for vulnerable individuals and distressed mental health professionals during the COVID-19 pandemic are necessary. Vulnerable populations require mental health care to minimize the potential negative consequences of the pandemic. Children and adolescents are vulnerable during the COVID-19 crisis. In particular, adolescents with psychiatric disorders are at higher risk of developing addictive disorders due to COVID-19-related problems and difficulties in adjusting to the pandemic. Therefore, government, educational and health care professionals, as well as parents should monitor and guide children and adolescents to stabilize their mood and reduce negative mental health effects of the COVID-19 crisis (70).
So far, most studies during COVID-19 indicate an increase in alcohol consumption and online gaming behavior. Further studies are needed to develop an approach for follow-up to better identify individual vulnerabilities and long-term impacts of the current pandemic on addictive behaviors.
Author Contributions
All authors conceptualized the manuscript. SX, MP, and JK reviewed the literature, edited and critically reviewed the manuscript, and approved the final version. UK and J-SC edited and critically reviewed the manuscript, and approved the final version. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the KBRI basic research program (21-BR-03-08 to JK and 21-BR-03-03 to UK and J-SC).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Hiremath P, Kowshik CS, Manjunath M, Shettar M. COVID 19: impact of lock-down on mental health and tips to overcome. Asian J Psychiatr. (2020) 51:102088. doi: 10.1016/j.ajp.2020.102088
2. Mukhtar S. Psychological health during the coronavirus disease 2019 pandemic outbreak. Int J Soc Psychiatr. (2020) 66:512–6. doi: 10.1177/0020764020925835
3. Mackolil J. Addressing psychosocial problems associated with the COVID-19 lockdown. Asian J Psychiatr. (2020) 51:102156. doi: 10.1016/j.ajp.2020.102156
4. Torjesen I. Covid-19: mental health services must be boosted to deal with “tsunami” of cases after lockdown. BMJ. (2020) 369:m1994. doi: 10.1136/bmj.m1994
5. Lippi G, Henry BM, Bovo C, Sanchis-Gomar F. Health risks and potential remedies during prolonged lockdowns for coronavirus disease 2019 (COVID- 19). Diagnosis (Berl). (2020) 7:85–90. doi: 10.1515/dx-2020-0041
6. Volkow ND. Collision of the COVID-19 and addiction epidemics. Ann Intern Med. (2020) 173:61–2. doi: 10.7326/M20-1212
7. DiMaggio C, Galea S, Li G. Substance use and misuse in the aftermath of terrorism. A Bayesian meta-analysis. Addiction. (2009) 104:894–904. doi: 10.1111/j.1360-0443.2009.02526.x
8. Lee JY, Kim SW, Kang HJ, Kim SY, Bae KY, Kim JM, et al. Relationship between problematic internet use and post-traumatic stress disorder symptoms among students following the Sewol ferry disaster in South Korea. Psychiat Invest. (2017) 14:871–5. doi: 10.4306/pi.2017.14.6.871
9. Gonçalves PD, Moura HF, do Amaral RA, Castaldelli-Maia JM, Malbergier, A. Alcohol use and COVID-19: can we predict the impact of the pandemic on alcohol use based on the previous crises in the 21st century? A brief review. Front Psychiatry. (2020) 11:1456. doi: 10.3389/fpsyt.2020.581113
10. Koob G, Kreek MJ. Stress, dysregulation of drug reward pathways, and the transition to drug dependence. Am J Psychiatry. (2007) 164:1149–59. doi: 10.1176/appi.ajp.2007.05030503
11. Clay JM, Parker MO. Alcohol use and misuse during the COVID-19 pandemic: a potential public health crisis? Lancet Public Health. (2020) 5:e259. doi: 10.1016/S2468-2667(20)30088-8
12. Montag C, Elhai JD. Discussing digital technology overuse in children and adolescents during the COVID-19 pandemic and beyond: on the importance of considering Affective Neuroscience Theory. Addict Behav Rep. (2020) 12:100313. doi: 10.1016/j.abrep.2020.100313
13. Ahmed MZ, Ahmed O, Aibao Z, Hanbin S, Siyu L, Ahmad A. Epidemic of COVID-19 in China and associated Psychological Problems. Asian Psychiatr J. (2020) 51:102092. doi: 10.1016/j.ajp.2020.102092
14. Sun Y, Li Y, Bao Y, Meng S, Sun Y, Schumann G, et al. Brief report: increased addictive internet and substance use behavior during the COVID-19 pandemic in China. Am J Addict. (2020) 29:268–70. doi: 10.1111/ajad.13066
15. Stanton R, To QG, Khalesi S, Williams SL, Alley SJ, Thwaite TL, et al. Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int J Environ Res Public Health. (2020) 17:4065. doi: 10.3390/ijerph17114065
16. Jackson SE, Garnett C, Shahab L, Oldham M, Brown J. Association of the COVID-19 lockdown with smoking, drinking and attempts to quit in England: an analysis of 2019–20 data. Addiction. (2021) 116:1233–44. doi: 10.1111/add.15295
17. Daly M, Robinson E. High-risk drinking in midlife before versus during the COVID-19 crisis: longitudinal evidence from the United Kingdom. Am J Prev Med. (2021) 60:294–7. doi: 10.1016/j.amepre.2020.09.004
18. Niedzwiedz CL, Green MJ, Benzeva, M, Campbell D, Craig P, et al. Mental health and health behaviours before and during the initial phase of the COVID-19 lockdown: longitudinal analyses of the UK Household Longitudinal Study. J Epidemiol Commun Health. (2021) 75:224–31. doi: 10.1101/2020.06.21.20136820
19. Suffoletto B, Ram N, Chung T. In-person contacts and their relationship with alcohol consumption among young adults with hazardous drinking during a pandemic. J Adolesc Health. (2020) 67:671–6. doi: 10.1016/j.jadohealth.2020.08.007
20. Korean Addiction Forum (KAF). Republic of Korea: COVID-19 Pandemic & Change in Addictive Behaviors (2020). Available online at: http://www.addictionfr.org/2020/bbs/board.php?bo_table=sub06_1&wr_id=33&page=1 (accessed May 30, 2021).
21. Weerakoon SM, Jetelina KK, Knell G. Longer time spent at home during COVID-19 pandemic is associated with binge drinking among US adults. Am J Drug Alcohol Abuse. (2020) 47:98–106. doi: 10.1080/00952990.2020.1832508
22. KSTSS. The fourth national mental health survey (2021). Korean Society for Traumatic Stress Studies. Available online at: http://kstss.kr/?p=2065 (accessed May 30, 2021).
23. Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA, Ambulatory Care Quality Improvement Project (ACQUIP). The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Arch Intern Med. (1998) 158:1789–95. doi: 10.1001/archinte.158.16.1789
24. Khazaal Y, Van Singer M, Chatton A, Achab S, Zullino D, Rothen S, et al. Does self-selection affect samples' representativeness in online surveys? An investigation in online video game research. J Med Internet Res. (2014) 16:e164. doi: 10.2196/jmir.2759
25. Pollard MS, Tucker JS, Green HD. Changes in adult alcohol use and consequences during the COVID-19 pandemic in the US. JAMA Netw Open. (2020) 3:e2022942. doi: 10.1001/jamanetworkopen.2020.22942
26. Butler TR, Karkhanis AN, Jones SR, Weiner JL. Adolescent social isolation as a model of heightened vulnerability to comorbid alcoholism and anxiety disorders. Alcohol Clin Exp Res. (2016) 40:1202–14. doi: 10.1111/acer.13075
27. Davidson RJ, McEwen BS. Social influences on neuroplasticity: stress and interventions to promote well-being. Nat Neurosci. (2012) 15:689–95. doi: 10.1038/nn.3093
28. Torres SJ, Nowson CA. Relationship between stress, eating behavior, and obesity. Nutrition. (2007) 23:887–94. doi: 10.1016/j.nut.2007.08.008
29. Mattioli AV, Sciomer S, Maffei S, Gallina S. Lifestyle and stress management in women during COVID-19 pandemic: impact on cardiovascular risk burden. Am J Lifestyle Med. (2020) 15:356–9. doi: 10.1177/1559827620981014
30. Peltier MR, Verplaetse TL, Mineur YS, Petrakis IL, Cosgrove KP, Picciotto MR, et al. Sex differences in stress-related alcohol use. Neurobiol Stress. (2019) 10:100149. doi: 10.1016/j.ynstr.2019.100149
31. Agabio R, Campesi I, Pisanu C, Gessa GL, Franconi F. Sex differences in substance use disorders: focus on side effects. Addict Biol. (2016) 21:1030–42. doi: 10.1111/adb.12395
32. Fox HC, Sinha R. Sex differences in drug-related stress-system changes: implications for treatment in substance-abusing women. Harv Rev Psychiatry. (2009) 17:103–19. doi: 10.1080/10673220902899680
33. Slade T, Chapman C, Swift W, Keyes K, Tonks Z, Teesson M. Birth cohort trends in the global epidemiology of alcohol use and alcohol-related harms in men and women: systematic review and metaregression. BMJ Open. (2016) 6:e011827. doi: 10.1136/bmjopen-2016-011827
34. Struk AA, Scholer AA, Danckert J, Seli P. Rich environments, dull experiences: how environment can exacerbate the effect of constraint on the experience of boredom. Cogn Emot. (2020) 34:1517–23. doi: 10.1080/02699931.2020.1763919
35. Hasler BP, Soehner AM, Clark DB. Sleep and circadian contributions to adolescent alcohol use disorder. Alcohol. (2015) 49:377–87. doi: 10.1016/j.alcohol.2014.06.010
36. Minkel JD, Banks S, Htaik O, Moreta MC, Jones CW, McGlinchey EL, et al. Sleep deprivation and stressors: evidence for elevated negative affect in response to mild stressors when sleep deprived. Emotion. (2012) 12:1015–20. doi: 10.1037/a0026871
37. Sinha R. Chronic stress, drug use, and vulnerability to addiction. Ann N Y Acad Sci. (2008) 1141:105–30. doi: 10.1196/annals.1441.030
38. Khantzian EJ. The self-medication hypothesis of addictive disorder: focus on heroin and cocaine dependence. Am J Psychiatry. (1985) 142:1259–64. doi: 10.1176/ajp.142.11.1259
39. Holahan CJ, Moos RH, Holahan CK, Cronkite RC, Randall PK. Drinking to cope, emotional distress and alcohol use and abuse: a ten-year model. J Stud Alcohol. (2001) 62:190–8. doi: 10.15288/jsa.2001.62.190
40. Koob GF, Powell P, White A. Addiction as a coping response: hyperkatifeia, deaths of despair, and COVID-19. Am J Psychiatry. (2020) 177:1031–7. doi: 10.1176/appi.ajp.2020.20091375
41. Veenstra MY, Lemmens PH, Friesema IH, Tan FE, Garretsen HF, Knottnerus JA, et al. Coping style mediates impact of stress on alcohol use: a prospective population-based study. Addiction. (2007) 102:1890–8. doi: 10.1111/j.1360-0443.2007.02026.x
42. Moos RH. Theory-based active ingredients of effective treatments for substance use disorders. Drug Alcohol Depend. (2007) 88:109–21. doi: 10.1016/j.drugalcdep.2006.10.010
43. Rossow I, Bye EK, Moan IS, Kilian C, Bramness JG. Changes in alcohol consumption during the COVID-19 pandemic—small change in total consumption, but increase in proportion of heavy drinkers. Int J Environ Res Public Health. (2021) 18:4231. doi: 10.3390/ijerph18084231
44. Manthey J, Kilian C, Schomerus G, Kraus L, Rehm J, Schulte B. Alkoholkonsum in Deutschland und Europa während der SARS-CoV-2 Pandemie. Sucht. (2020) 66:247–58. doi: 10.1024/0939-5911/a000686
45. Litman L, Robinson J, Abberbock T. TurkPrime. com: a versatile crowdsourcing data acquisition platform for the behavioral sciences. Behav Res Methods. (2017) 49:433–42. doi: 10.3758/s13428-016-0727-z
46. Killgore WD, Cloonan SA, Taylor EC, Lucas DA, Dailey NS. Alcohol dependence during COVID-19 lockdowns. Psychiatry Res. (2021) 296:113676. doi: 10.1016/j.psychres.2020.113676
47. National Institute on Alcohol Abuse and Alcoholism. NIAAA Council Approves Definition of Binge Drinking. NIAAA Newsletter. N° 3. Winter (2004).
48. Király O, Potenza MN, Stein DJ, King DL, Hodgins DC, Saunders JB, et al. Preventing problematic internet use during the COVID-19 pandemic: consensus guidance. Compr Psychiatry. (2020) 100:152180. doi: 10.1016/j.comppsych.2020.152180
49. Panno A, Carbone GA, Massullo C, Farina B, Imperatori C. COVID-19 related distress is associated with alcohol problems, social media and food addiction symptoms: insights from the Italian experience during the lockdown. Front Psychiatry. (2020) 11:577135. doi: 10.3389/fpsyt.2020.577135
50. Blasi MD, Giardina A, Giordano C, Coco GL, Tosto C, Billieux J, et al. Problematic video game use as an emotional coping strategy: evidence from a sample of MMORPG gamers. J Behav Addict. (2019) 8:25–34. doi: 10.1556/2006.8.2019.02
51. Griffiths MD. The therapeutic and health benefits of playing video games. In: Attrill-Smith A, Fullwood C, Keep M, Kuss DJ, editors. The Oxford Handbook of Cyberpsychology. Oxford: Oxford University Press (2019). p. 485–505. doi: 10.1093/oxfordhb/9780198812746.013.27
52. Dong H, Yang F, Lu X, Hao W. Internet addiction and related psychological factors among children and adolescents in China during the coronavirus disease 2019 (COVID-19) epidemic. Front Psychiatry. (2020) 11:00751. doi: 10.3389/fpsyt.2020.00751
53. Ellis LA, Lee MD, Ijaz K, Smith J, Braithwaite J, Yin K. COVID-19 as ‘Game Changer’for the physical activity and mental well-being of augmented reality game players during the pandemic: mixed methods survey study. J Med Internet Res. (2020) 22:e25117. doi: 10.2196/25117
54. Park M, Jung MH, Lee J, Choi AR, Chung SJ, Kim B, et al. Neurophysiological and cognitive correlates of error processing deficits in internet gaming disorder. Cereb Cortex. (2020) 30:4914–21. doi: 10.1093/cercor/bhaa083
55. Teng Z, Pontes HM, Nie Q, Griffiths MD, Guo C. Depression and anxiety symptoms associated with internet gaming disorder before and during the COVID-19 pandemic: a longitudinal study. J Behav Addict. (2021) 10:169–80. doi: 10.1556/2006.2021.00016
56. Ryu H, Lee JY, Choi A, Chung SJ, Park M, Bhang SY, et al. Application of diagnostic interview for internet addiction (DIA) in clinical practice for Korean adolescents. J Clin Med. (2019) 8:202. doi: 10.3390/jcm8020202
57. Fernandes B, Biswas UN, Mansukhani RT., Casarín AV, Essau CA. The impact of COVID-19 lockdown on internet use and escapism in adolescents. Rev Psicol Clín. Niños Adolesc. (2020) 7:59–65. doi: 10.21134/rpcna.2020.mon.2056
58. Siste K, Hanafi E, Lee T, Sen HC, Adrian LPS, Limawan AP, et al. The impact of physical distancing and associated factors towards internet addiction among adults in indonesia during COVID-19 pandemic: a nationwide web-based study. Front Psychiatry. (2020) 11:580977. doi: 10.3389/fpsyt.2020.580977
59. Servidio R, Bartolo MG, Palermiti AL, Costabile A. Fear of COVID-19, depression, anxiety, and their association with Internet addiction disorder in a sample of Italian students. J Affect Disord. (2021) 4:100097. doi: 10.1016/j.jadr.2021.100097
60. Fazeli S, Zeidi IM, Lin CY, Namdar P, Griffiths MD, Ahorsu DK, et al. Depression, anxiety, and stress mediate the associations between internet gaming disorder, insomnia, and quality of life during the COVID-19 outbreak. Addict Behav Rep. (2020) 12:100307. doi: 10.1016/j.abrep.2020.100307
61. Islam MS, Sujan MSH, Tasnim R, Ferdous MZ, Masud JHB, Kundu S, et al. Problematic internet use among young and adult population in Bangladesh: correlates with lifestyle and online activities during the COVID-19 pandemic. Addict Behav Rep. (2020) 12:100311. doi: 10.1016/j.abrep.2020.100311
62. KOCCA. The 7th survey report of the game users in Korea (2020). Korea Creative Content Agency. Available online at: https://www.kocca.kr/cop/bbs/view/B0000147/1842858.do?menuNo=201825 (accessed May 30, 2021).
63. Widyanto L, McMurran M. The psychometric properties of the internet addiction test. Cyberpsychol Behav. (2004) 7:443–50. doi: 10.1089/cpb.2004.7.443
64. Wong HY, Mo HY, Potenza MN, Chan MNM, Lau WM, Chui TK, et al. Relationships between severity of internet gaming disorder, severity of problematic social media use, sleep quality and psychological distress. Int J Environ Res Public Health. (2020) 17:1879. doi: 10.3390/ijerph17061879
65. Skrzynski CJ, Creswell KG. Associations between solitary drinking and increased alcohol consumption, alcohol problems, and drinking to cope motives in adolescents and young adults: a systematic review and meta-analysis. Addiction. (2020) 115:1989–2007. doi: 10.1111/add.15055
66. Creswell KG. Drinking together and drinking alone: a social-contextual framework for examining alcohol use disorder risk. Curr Dir Psychol Sci. (2020) 30:19–25. doi: 10.1177/0963721420969406
67. Addiction Policy Forum. Free smartphone app offering telehealth support for those struggling with addiction during COVID-19 (2020). Available online at: https://www.addictionpolicy.org/post/free-smartphone-app-offering-telehealth-support-for-those-struggling-with-addiction-during-covid-19 (accessed May 30, 2021).
68. King DL, Delfabbro PH, Billieux J, Potenza MN. Problematic online gaming and the COVID-19 pandemic. J Behav Addict. (2020) 9:184–6. doi: 10.1556/2006.2020.00016
69. Amin KP, Griffiths MD, Dsouza DD. Online gaming during the COVID-19 pandemic in India: strategies for work-life balance. Int J Ment Health Addict. (2020) 1–7. doi: 10.1007/s11469-020-00358-1
Keywords: alcohol, online gaming, addiction, COVID-19, pandemic, coping
Citation: Xu S, Park M, Kang UG, Choi J-S and Koo JW (2021) Problematic Use of Alcohol and Online Gaming as Coping Strategies During the COVID-19 Pandemic: A Mini Review. Front. Psychiatry 12:685964. doi: 10.3389/fpsyt.2021.685964
Received: 26 March 2021; Accepted: 17 May 2021;
Published: 14 June 2021.
Edited by:
Liana Fattore, National Research Council (CNR), ItalyReviewed by:
Anna Vittoria Mattioli, University of Modena and Reggio Emilia, ItalySeyed Ramin Radfar, Tehran University of Medical Sciences, Iran
Andreas Heinz, University of Luxembourg, Luxembourg
Copyright © 2021 Xu, Park, Kang, Choi and Koo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ung Gu Kang, kangug@snu.ac.kr; Jung-Seok Choi, choijs73@gmail.com; Ja Wook Koo, jawook.koo@kbri.re.kr
 Shijie Xu
Shijie Xu Minkyung Park
Minkyung Park Ung Gu Kang
Ung Gu Kang Jung-Seok Choi
Jung-Seok Choi Ja Wook Koo
Ja Wook Koo