Functional Outcomes in Survivors of Pediatric Sepsis: A Scoping Review and Discussion of Implications for Low- and Middle-Income Countries
- 1Division of Pediatric Pulmonology and Critical Care, Department of Pediatrics, All India Institute of Medical Sciences, New Delhi, India
- 2Department of Pediatrics, All India Institute of Medical Sciences, Bhubaneswar, India
Background: Pediatric sepsis is an important cause of mortality and morbidity in low- and middle-income countries (LMIC), where there is a huge burden of infectious diseases. Despite shortage of resources, adapting protocol-based care has reduced sepsis-related deaths but survivors of pediatric sepsis are at risk of poor functional outcomes.
Objectives: To perform a scoping review of the literature on functional outcomes of pediatric sepsis survivors after discharge from the intensive care unit (ICU) and discuss the implications for patients in LMICs. The outcomes include prevalence of survival with reduced functional outcomes or quality of life (QoL) and changes over time during follow-up or recovery, and these outcomes were compared with other groups of children.
Methods: We searched major medical electronic databases for relevant literature from January 2005 until November 2021, including Medline (via PubMed), Embase, CINAHL, and Google Scholar databases. We included observational studies and follow-up data from clinical trials involving children/adolescents (≤18 years) who were admitted to pediatric intensive care unit (PICU) and got discharged finally. Major focus was on survivors of sepsis in LMIC. We followed PRISMA guidelines for scoping reviews (PRISM-ScR).
Results: We included eight papers reporting data of functional outcomes in 2,915 children (males = 53%, and comorbidity present in 56.6%). All included studies were either a prospective or retrospective cohort study. Studies were classified as Level II evidence. Disabilities affecting physical, cognitive, psychological, and social function were reported in children following discharge. Overall disability reported ranged between 23 and 50% at hospital discharge or 28 days. Residual disability was reported at 1, 3, 6, and 12 months of follow-up with an overall improving trend. Failure to recover from a baseline HRQL on follow-up was seen in one-third of survivors. Organ dysfunction scores such as pSOFA, PeLOD, vasoactive inotrope score, neurological events, immunocompromised status, need for CPR, and ECMO were associated with poor functional outcome.
Conclusions: The research on functional outcomes in pediatric sepsis survivors is scarce in LMIC. Measuring baseline and follow-up functional status, low-cost interventions to improve management of sepsis, and multidisciplinary teams to identify and treat disabilities may improve functional outcomes.
Introduction
Sepsis is a state of dysregulated host response to infection and a major cause of mortality and morbidity. Although infectious diseases and sepsis-related mortality have decreased globally, the burden remains high in low-middle income countries (LMIC) (1). Pediatric severe sepsis accounts for >8% of critically ill children with in-hospital mortality around 25%. One-third of children develop progressive organ dysfunction, and nearly one in five survivors show new functional disability (2). Underlying malnutrition, chronic illness, and immunosuppressed state further increase the risk of mortality (3). With Surviving Sepsis Campaign (SSC) and advances in critical care, mortality due to sepsis has decreased (4). However, survivors of sepsis are increasing and continue to require long-term care. Patients recovering from sepsis develop 1-2 new functional limitations with 10–40% cognitive dysfunction (5). Children who recover from sepsis also have a chance of reinfection likely due to loss of adaptive immunity and reduction in lymphocytes (6). Sepsis is therefore a life-changing and disability-inducing event. Characteristics associated with complications after hospital discharge include pre-sepsis health status, acute septic episode determinants, and quality of hospital treatment (7).
Childhood infections like pneumonia, diarrhea, and malaria account for the leading causes of mortality in children under 5 years of age globally as per the WHO fact sheet of 2019 (8). Integrated Management of Neonatal and Childhood Illness (IMNCI) programs to assess, manage, and refer sick neonates and children at primary and community healthcare levels have resulted in substantial reduction of mortality (9). The SSC guidelines and American College of Critical Care Medicine (ACCM) Clinical Practice Parameters for Hemodynamic Support of Pediatric and Neonatal Septic Shock provide evidence-based guidelines, sepsis bundles, and checklists to guide management based on the availability of resources (10, 11). Apart from these strategies, antibiotic prophylaxis, immunization, and quality improvement initiatives may reduce the morbidity and mortality by prevention of sepsis (12).
Based on the availability of resources, there is a great disparity in the levels of care provided in different regions around the world (13, 14). Critical care includes treatment of children with a life-threatening illness or injury in its broadest sense, without regard for the location and including pre-hospital and emergency and intensive care (15). This is in comparison to intensive care which is provided in the intensive care unit (ICU) with advanced monitoring necessitating sophisticated equipment. In the LMIC, many hospitals lack designated ICUs, adequate number of trained healthcare staff, and access to necessary medications and equipment (16). The focus in these low-resource settings is on developing low-cost, high-yield interventions and aims for improving short-term outcomes (17). Even within each of the LMICs, links between various levels in the pyramid of healthcare are often missing and vary between rural and urban areas (16). Transport of sick patients, emergency stabilization, and tertiary critical care are often suboptimal or lacking. In such areas with limited access to healthcare, follow-up and post-critical care rehabilitation often take a back seat. Consequently, there is substantially high chance of short-term post-discharge mortality as well as poor long-term outcomes (18). Although long-term outcomes among sepsis survivors in developing countries are hardly reported, follow-up in African children showed a post-discharge mortality of 10% within 2 years of pneumonia and 1.5% within 20 days following malaria (19, 20).
Objectives
The objectives of this review are to perform a scoping review of the literature on the functional outcomes of pediatric sepsis survivors after discharge from the ICU and discuss the implications for patients in LMICs. The outcomes include prevalence of survival with reduced functional outcomes or quality of life (QoL) and changes over time during follow-up or recovery, and these outcomes are compared with other groups of children (if data are available).
Methods
This scoping review was conducted to map the existing knowledge on the functional outcomes of pediatric patients admitted to the ICU with sepsis. In general, the aim of a scoping review is to collect, analyze, and present a comprehensive map of existing evidence on an important topic (21). We used frameworks and recommendations while conducting this scoping review (22, 23). The stages were (1) research question identification, (2) searching of databases to get relevant studies, (3) study selection, (4) presentation of the data, (5) reporting of the result, and (6) consultation with stakeholders (optional stage). Therefore, our review team consisted of a pediatric intensivist, a general pediatrician, and an information specialist. The PRISMA Extension for Scoping Reviews (PRISMA-ScR) was followed while preparing and reporting the findings of this review (24).
Types of Studies
Inclusion Criteria
Observational studies that report about functional outcomes or QoL in children at discharge as well as during subsequent follow-ups (at 1, 3, 6, and 12 months) were included. The study should have included only children (>1-month to <18-year-age groups) or have outcomes reported separately for children (if both adults and children are the study population).
Exclusion Criteria
Studies reporting only mortality, unpublished data, and those not published in English language were excluded.
Types of Participants
Children of the >1-month to <18-year age groups and both sexes were included.
Types of Exposure
The type of exposure in this review includes children diagnosed with sepsis or septic shock and admitted to an ICU or pediatric intensive care unit (PICU). Sepsis, severe sepsis, and septic shock are defined as per published guidelines (25).
Types of Outcome Measures
The outcomes reported include cognitive, physical, psychosocial, and function deficits in activities of daily living that have been assessed on any standard scale within the post-ICU care syndrome (PICS) framework.
Search Methodology and Study Selection
We searched major medical electronic databases for relevant literature until November 15, 2021, including Medline (via PubMed), Embase, CINAHL, and Cochrane CENTRAL. We included observational studies and follow-up data from clinical trials involving children/adolescents (≤18 years) who were admitted to PICUs and got discharged finally. Major focus was on survivors of sepsis in LMIC. The following search terms were used to search PubMed database: (“functional”[All Fields] OR “functionally”[All Fields] OR “functionals”[All Fields] OR “functioned”[All Fields] OR “functioning”[All Fields] OR “functions”[All Fields] OR “physiology”[MeSH Subheading] OR “physiology”[All Fields] OR “function”[All Fields] OR “physiology”[MeSH Terms]) AND (“outcome”[All Fields] OR “outcomes”[All Fields]) AND (“sepsis”[MeSH Terms] OR “sepsis”[All Fields]) AND (“pediatrics”[All Fields] OR “pediatrics”[MeSH Terms] OR “pediatrics”[All Fields] OR “pediatric”[All Fields] OR “pediatric”[All Fields]) AND (“critical care”[MeSH Terms] OR (“critical”[All Fields] AND “care”[All Fields]) OR “critical care”[All Fields]) AND (“patient s”[All Fields] OR “patients”[MeSH Terms] OR “patients”[All Fields] OR “patient”[All Fields] OR “patients s”[All Fields]). Two reviewers (JS and NR) applied the study selection criteria for titles and abstracts and then full texts. Any conflicts regarding inclusion of articles were discussed with the third author (RRD).
Data Extraction
Data extraction was done using a data extraction form that was designed and pilot tested a priori. Two authors (NR, JS) independently extracted the following information from each study: author, year, location (country), study design, details of participants (age, sex, sample size, disease severity, and comorbidity), exposure/intervention details, outcomes (outcome definition, valid unit of measurement, time points of collection and reporting), loss to follow-up, and miscellaneous data (key conclusions, references to other studies, and additional data required).
Data Synthesis and Presentation of Results
This was done in the following 3 steps: (a) data analysis, (b) reporting of the findings, and (c) discussion of the implications. A narrative synthesis of data was done to analyze and report the findings.
Results
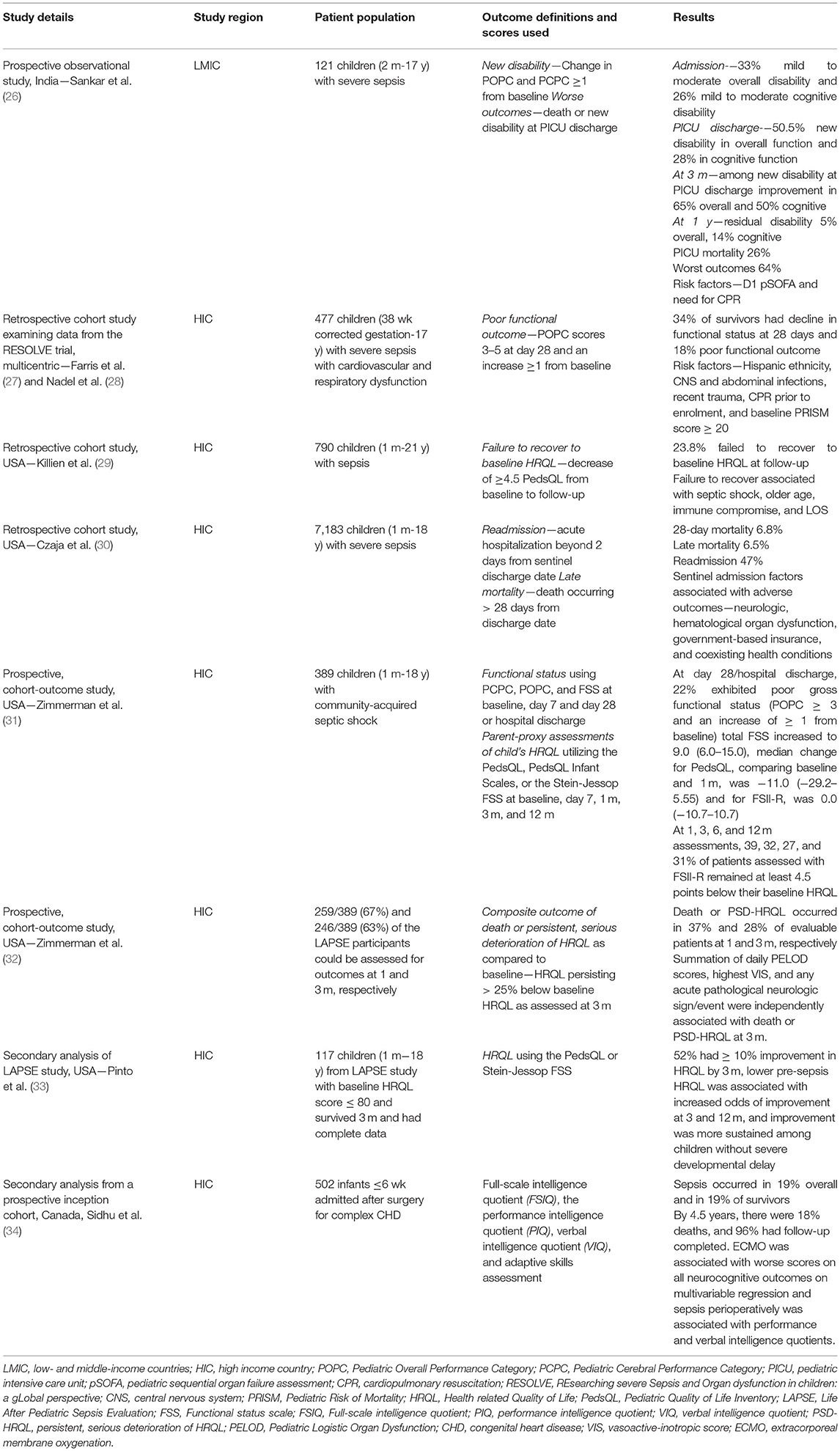
Of 382 total citations retrieved, the full text of 17 papers was assessed for eligibility (Figure 1). Finally, 8 papers including 10,209 children were included (Table 1). Of the 10,209 children, data on functional outcomes were reported for 2,915 children. The age range of the included children was 1 month to 18 years, and 53% were male. Comorbidity was present in 56.6% children. The studies were conducted in the following countries: USA (n = 6), Canada (n = 1), and India (n = 1). Included studies were published from 2013 onward. All studies were cohort studies, both prospective (n = 5), and retrospective (n = 3). Studies were classified as Level II evidence. Table 1 summarizes the studies on functional outcomes in pediatric sepsis.
The most common scales used in the pediatric sepsis studies reporting functional outcome were POPC (Pediatric Overall Performance Category), PCPC (Pediatric Cerebral Performance Category), HRQL (Health-related Quality of Life) using PedsQL (Pediatric Quality of Life Inventory), and Functional status scales. Late mortality and readmission were also reported as long-term outcomes. Overall disability reported in PICU survivors ranged between 23 and 50% at hospital discharge or 28 days. Residual disability was measured at various periods of follow-up such as 1, 3, 6, and 12 months from discharge with an overall improving trend with time. Failure to recover from a baseline HRQL from baseline was done at similar time intervals of follow-up, and about one-third of survivors remained 4.5 points below baseline at follow-up. Organ dysfunction scores such as Pediatric Sequential Organ Failure Assessment (pSOFA), Pediatric Logistic Organ Dysfunction (PeLOD), vasoactive inotrope score (VIS), neurological events, immunocompromised status, need for cardiopulmonary resuscitation (CPR), and extracorporeal membrane oxygenation (ECMO) were the common factors associated with poor functional outcome.
In the study by Sankar et al. from India, 121 children aged 2 months to 17 years with severe sepsis were included. Of 82 children who did not have “any disability” at admission in overall function, 39 were found to have “new disability” at PICU discharge (mild = 26, moderate = 11, and severe = 2). Of 36 children with “mild disability” at admission, 6 had “new moderate disability” at PICU discharge. This means that a total of 45 out of 89 children (50.5%) had “new disability” in overall function at PICU discharge. Similarly, a total of 25 out of 89 children (28%) had “new disability” in cognitive function at PICU discharge. At 3 months, 28 (65%) showed improvement in overall function, and 12 (50%) in cognitive function. At 1 year, these numbers increased to 41 (95%) in overall, and 18 (86%) in cognitive function. This means that 5% were left with disability in overall function, and 14% in cognitive function.
In a retrospective cohort study examining data from the RESOLVE (REsearching severe Sepsis and Organ dysfunction in children) trial, Farris et al. included 477 children (term neonates to 17 years old) with severe sepsis and cardiovascular plus respiratory dysfunction. The authors found that 38% of survivors had decline in functional status at 28 days, and 18% had poor functional outcomes.
In another retrospective cohort study by Killien et al., 790 children (1 month to 21 years; term neonates to 17 years old) with sepsis were included. The authors found that 23.8% of survivors failed to recover to their baseline HRQL during follow-up.
In a population-based retrospective cohort study by Czaja et al., 7,183 children (1 month to 18 years) with severe sepsis were included. The authors found that 47% of survivors had emergency readmissions during a median follow-up period of 3 months.
Sidhu et al. carried out a secondary analysis of a prospective cohort study including 97 children with sepsis after congenital heart disease surgery. Of the 76 survivors of sepsis, all had decreased intelligent quotient (IQ) on various scales at 4.5 years.
Zimmerman et al. in their prospective cohort study [LAPSE (Life After Pediatric Sepsis Evaluation) study] included 389 children (1 month to 18 years) with community-acquired septic shock. At 1 month, death or HRQL deterioration was noted in 37%, and the same was 28% at 3 months.
Pinto et al. carried out a secondary analysis of the LAPSE study including 117 children (1 month to 18 years) and found 61 (52%) to have ≥10% improvement in HRQL at 3 months.
While there is scarcity of data on functional outcomes in survivors of pediatric sepsis from LMIC, the overall and cognitive disability rates were comparable to those found in studies from HIC. The important risk factors for poor outcome were also similar. This was based on the authors' assessment of POPC and PCPC scores at admission, discharge, and follow-up. However, most studies in HIC also looked at HRQL with parent questionnaires.
Discussion
Survivors of pediatric sepsis were reported to have poor functional outcomes in LMIC as well as HIC. POPC, PCPC, and HRQL were the commonly used scales for measuring outcomes. The usual follow-up intervals used to document trend over time were 1, 3, 6, and 12 months from discharge. Common factors associated with poor functional outcome were pSOFA, PeLOD, vasoactive inotrope score, neurological events, immunocompromised status, need for CPR, and ECMO.
Importance of Measuring Functional Outcomes in LMICs
Despite a huge burden of sepsis in LMIC, there is heterogeneity in patient population and level of care accessible, as well as differences in disease characteristics including type of infections based on the locality. The variation in mortality reported in studies may be contributed by many of these factors. Sepsis-related mortality has reduced overall and may no longer be the sole meaningful outcome. The effects of sepsis extend beyond the hospitalization and include long-term disability, hospital readmission, and late mortality. As survivors from sepsis increase, their long-term outcomes in terms of disability, their need for prolonged care, the QoL of children as well as their caregivers, psychosocial impact, and other such outcomes need to be studied.
A systematic review by Menon et al. found mortality, shock, and organ dysfunction as the commonly reported primary outcome measures in pediatric septic shock trials (35). About one-third of sepsis survivors have mild to moderate disability and poor functional outcome (27). Children with multiorgan dysfunction syndrome (MODS) at PICU admission were more likely to have a discharge POPC score >3 (36.3 vs. 17.4%, p < 0.0001) as well as a discharge PCPC score >3 (29.3 vs. 12.2%, p < 0.0001), indicating at least moderate impairment in functional status at the time of PICU discharge. Among children discharged in a vegetative or comatose state, 64% had MODS at admission to the PICU (36).
There is limited research on long-term outcomes following critical illness in children. In LMIC, post-discharge mortality may exceed the in-hospital deaths and often go unreported (37). Loss of cases to follow-up adds to this problem. Choosing an appropriate outcome measure is extremely important to assess utility of an intervention in a given setting (38). Core outcome sets designed specifically for LMICs may be needed to overcome the inconsistency in the reported outcomes and improve the quality and relevance for the local region (39, 40).
Post-ICU Care Syndrome—Pediatrics
PICS is a group of cognitive, physical, and mental health impairments that commonly occur in patients after ICU discharge (41). It may occur as a part of long-term effects of sepsis in PICU survivors (42). Therapeutic interventions like sedation and prolonged mechanical ventilation may contribute to PICS (43). Functional and cognitive impairments may affect growth and development, school performance, and social interactions. However, the child's capacity for growth may be a source of resilience that provides a platform for recovery after critical illness (42).
Domains of Function
Functional status comprises the ability to perform daily activities of living to meet the basic needs and maintain health (44). It includes mainly the physical, cognitive, psychological, and social function (42).
Physical Function
Sepsis through its effects on various organ systems as well as the interventions and medications for organ support may cause various physical impairments. Respiratory dysfunction, difficulty in mobilization, pain, and sensory dysfunction may all lead to inability to take care of oneself (45). ICU-acquired weakness may also contribute to physical limitation due to neuropathy or myopathy. Swallowing difficulty may lead to risk of recurrent aspirations (7). POPC score is widely used to categorize the degree of overall functional impairment (46). Among PICU admissions, physical sequelae were reported in 69% of children, with 30% of them secondary to previous illness and 39% due to acquired morbidity. In 8% of children, the acquired morbidity was related to complications from PICU procedures (47).
Cognitive Function
Neurological damage secondary to shock-related ischemia, sepsis-associated inflammation, and metabolic derangements may result in cognitive dysfunction. Prolonged sedation, pain, awareness during ICU stay, delirium, invasive mechanical ventilation, and prolonged length of stay (LOS) in the ICU may also contribute. It may manifest as deficits in memory, attention, and speech. Poor scholastic performance can be seen even in those without obvious cognitive dysfunction. Sepsis increases the prevalence of moderate to severe cognitive dysfunction by almost 10% in relation to non-septic adult patients (48). A Dutch study in children with septic shock reported over 40% cognitive dysfunction in their cohort (49). The PCPC score has been used to estimate global baseline cognitive function and change over the ICU stay (46). These scores may evolve with time with either gradual improvement on follow-up or a few showing further decline (47).
Psychosocial Function
Irritability, hyperactivity, anxiety, and emotional and conduct problems are encountered in children discharged following critical illness (50). Psychiatric disorders like depression, hallucinations, delusions, and post-traumatic stress disorder (PTSD) have been reported (51). Higher severity of illness, sepsis, invasive procedures, use of sedative, and paralytic agents have been found to be the risk factors (42). Following discharge, children may have behavioral and social difficulties. Age-appropriate self-report tools have been used for reporting and measuring psychosocial impact on children.
Parents and siblings of children may also experience psychological issues like anxiety, depression, and PTSD. Addressing parental issues is very important as the child and parents form an inseparable dyad and their emotional state has an impact on the child's mental state. Unexpected PICU admissions and more invasive procedures are common risks associated, which are often the case in children with sepsis. In developing countries, parents' level of understanding based on educational status, poverty, and lack of appropriate counseling may add to these issues.
Health-Related Quality of Life
Health-related quality of life (HRQL) encompasses the impact of health status on physical, mental, emotional, and social functioning. An important measure of health outcomes in children post-critical illness has been proposed (52). Sepsis and many of the treatment modalities used are some of the determinants of poor HRQL, with low socioeconomic status and parental education further contributing to it in developing countries (53). There are over 20 HRQL tools used in pediatric critical care studies. In this review, we have briefly discussed a Pediatric Quality of Life Inventory and a few child health questionnaires. The best tools include both self and proxy reports, cover a wide age range of children, are brief with a low response burden, are multidimensional, and should have internal consistency and test–retest reliability, sensitivity to change over time, and valid content and construct.
Indicators and Scores
The functional outcomes and HRQL in sepsis survivors largely remain unknown due to lack of valid uniform tools and criteria for assessment in children. Assessment may be time consuming and not practical for large sample sizes. Pediatric functional status assessment tools must also incorporate the rapidly changing norms of growth and development.
POPC and PCPC
Fiser developed and validated the POPC and PCPC scales to describe the short-term outcomes after critical illness or injury to quantify overall functional morbidity and cognitive impairment, respectively (46). The POPC includes 6 categories of function (normal, mild, moderate, severe disability, comatose, dead). PCPC includes the same 6 categories with mild, moderate, and severe “cognitive” disability. POPC scoring has been validated against and shown to be associated with measures obtained using the Bayley Psychomotor Developmental Index and the Vineland Adaptive Behavior Scales scores. Stanford–Binet Intelligence Quotients and Bayley Mental Developmental Index scores were significantly different across PCPC categories (54).
Functional Status Scale
The Functional Status Scale (FSS) was developed to provide the assessment of functional status suitable for large studies and applicable from full-term newborns to adolescents. It is composed of 6 domains (mental status, sensory, communication, motor function, feeding, respiratory) with domain scores ranging from 1 (normal) to 5 (very severe dysfunction). Total scores range from 6 to 30 with lower scores indicating better function (55). The FSS adds objectivity, increases granularity, and improves quantification of morbidities (54). The Collaborative Pediatric Critical Care Research Network (CPCCRN) conducted a prospective multicentre study in medical and cardiac PICUs assessing functional status at hospital discharge using FSS scores. New morbidity defined as an increase in the FSS of ≥3 was seen in 4.8% with highest among neurological diagnoses (7.3%) followed by acquired cardiovascular disease (5.9%) and cancer (5.3%) (56). New morbidities involved all FSS domains with the highest proportions involving respiratory, motor, and feeding dysfunction.
PedsQL 4.0
This scale consists of 4 subscales including physical, emotional, social, and school functioning (57). It is scored from 0 to 100 with physical and psychosocial subscales each scored from 0 to 100. A change of ≥4.5 points between two scores represents the minimum clinically significant difference (29). Conlon et al. studied the long-term HRQL outcomes in children with prolonged PICU stay using the Pediatric Quality of Life Inventory Version 4.0 (PedsQL 4.0) (52).
Royal Alexandra Hospital for Children Measure of Function
It is a modification of Children's Global Assessment Scale (CGAS) used in child psychiatry. There are two versions: the Clinical Rating Scale used by clinicians and the Family Rating Scale used by parents and children aged over 10 years (58). The total score of 100 is given with a score between 1 and 30 indicating a poor QoL, 31 and 70 a fair QoL, and a score between 71 and 100 a good QoL. Polic et al. compared QOL in children at 6 and 24 months of PICU discharge using this generic scoring system (59).
Questionnaires
For younger children (ages 0–3 years), the Infant–Toddler Quality of Life Questionnaire (ITQOL), Child Health Questionnaire-Parent Form 50 (CHQ-PF50) for 4–18 years filled by parents, and Short Form Health Survey (SF-12) for parents' HRQL have been used (60).
Studies on Functional Outcomes in Pediatric Sepsis
The European Childhood Life-threatening Infectious Disease Study (EUCLIDS) was a large prospective multicenter cohort study including 795 children admitted with sepsis to 52 European PICUs. The mortality in this study was 6%, and disability at discharge was 31% among the survivors (61).
The studies from LMIC on functional outcome in pediatric sepsis are scarce. In the study by Sankar et al. (26), the common infection sources were respiratory (35%), gastrointestinal (31%), and neurologic (21%) with 37% having comorbidities at admission. The difference in the proportion of children with new disability from the baseline using POPC and PCPC scores was significant (p < 0.0001). With increasing duration of follow-up, there was a decrease in the proportion of children with disability with more overall improvement than cognitive.
The analysis of pediatric sepsis survivors of the RESOLVE trial, a multicentric study by Farris et al. (27) for poor functional outcomes, included mostly high-income countries and only one center from middle income countries. POPC scores were used to detect moderate to severe disability at 28 days and no further follow-up for long-term outcomes.
In the HRQL study in survivors of pediatric sepsis by Killien et al. (29), the average parent–child scores of PedsQL 4.0 were obtained for baseline (status during the month prior to admission) and admission and followed up telephonically or electronically 2–12 weeks post-discharge. When controlled for immunocompromised status, the remaining chronic health conditions did not confer excess risk for decline in HRQL. Although illness severity scores did not correlate with poor outcomes, severity of sepsis was associated with failure to recover to baseline.
Czaja et al. (30) looked at the readmission and late mortality among sepsis survivors. Half of the cohort had comorbidities like respiratory disorders, neuromuscular, cardiovascular, and oncologic diseases, and one-fifth were surgical patients. Respiratory infections were the commonest source, and only 15% had multiorgan dysfunction. Late mortality rate was almost equal to 28-day mortality with the highest rate in the first 2 years of discharge. The primary diagnosis for the first readmission was respiratory related, particularly infections, for both with and without chronic illnesses (29 and 36%, respectively). This study shows the long-term effects of sepsis even though functional outcomes were not studied.
High- vs. Low-Middle Income Countries
Various factors contribute to differences in mortality and morbidity among the high- and middle-income countries. Apart from economic differences, social, and political barriers also play a part (62). Low economic status and lack of education also contribute to poor health seeking behavior. A comparison of outcomes in 2 PICUs with different resources showed higher mortality and poor functional outcomes in the Egyptian center compared to the PICU at Japan (63). There was wide variation in PICU structure in terms of staff number, trained pediatric critical care specialists, and availability of allied healthcare workers. Equipment and utilization of advanced technology was far more in the Tokyo center. The patient characteristics also differed with the PICU in the low-resource setup catering more to medical conditions but with an equal number of post-operative and medical patients in the PICU of HIC. The severity of illness was higher, mortality was more among infants with sepsis and congenital heart disease, and among the survivors, a higher percentage of children had poor cerebral function scores in Egypt. However, this study failed to compare treatment protocols of the 2 units.
Post-discharge Priorities
Following hospital discharge for sepsis, management should focus on (i) identifying new physical, mental, and cognitive problems and appropriate referral, (ii) reviewing and managing long-term illness and treatment, and (iii) identifying treatable conditions requiring admission. Ongoing evaluation and treatment on an outpatient basis for all survivors of pediatric sepsis for at least the first 3 months after hospital discharge, with particular attention to teenagers, those hospitalized for more than a week, immunocompromised patients, and those with septic shock are recommended (29). In a small subset with chronic illnesses prior to sepsis who experience further deterioration, palliation and symptomatic management may be considered (7).
Implications in LMIC
The commonly used tools for measuring functional outcome are easily available in LMIC and can be used for monitoring during PICU admission and follow-up. To ensure the application of these, adequate staff training and motivation are the key barriers due to shortage of manpower and high patient load. Training ancillary staff or employing research staff by prioritizing studies on quality improvement could be a first step.
Recommendations for Improving Functional Outcomes
Early Sepsis Care
Favourable functional outcomes could be achieved by early management of sepsis, ICU care and monitoring and rehabilitation (7). Appropriate timely antibiotics, adequate fluid resuscitation, vasoactive support, and source control improve not only mortality but reduce long-term sequelae by decreasing pathogen invasion, better host response, optimizing host–pathogen interaction, and limiting the opportunity for adverse events.
Pain, Sedation, and ICU Monitoring
Assessment of pain and requirement of sedation, sedation window when feasible, and monitoring for depth of sedation and delirium would reduce PTSD and cognitive impairment.
Mobility and Rehabilitation
Early mobilization can help in reducing physical disabilities and also reduce the duration of ICU stay.
Most of these are low-cost interventions that can be achieved in developing countries. However, hindrances including system-related factors like doctor: patient ratios, training of nurses, improving transport, and triaging remain to be considered.
The Way Forward
Establishment of good baseline measurements of functional status and QoL is important to associate sepsis and PICU interventions with a change in functional status. A multidisciplinary team approach with the involvement of general pediatricians, physical medicine and rehabilitation, and neuropsychologists is important to identify functional impairments. Identifying risk factors for adverse functional outcomes, early therapy, acute rehabilitation, and prevention of negative impact of various therapies could help in improving functional outcomes. Building clinical infrastructures to include critical illness follow-up clinics may help address the multifaceted needs of sepsis survivors (5). Implementation of a low-cost pediatric sepsis survivorship program is possible by utilizing existing systems of care and can help identify and improve functional outcomes (64). Research in areas to include QoL of sepsis survivors and caregivers needs to be encouraged. Short-term and long-term priorities to enhance sepsis survivorship may be adapted for children from the adult guidelines (5).
Author Contributions
JS conceptualized the review, searched the literature, helped in writing, and editing the manuscript. NR drafted the manuscript and edited the final version. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Rudd KE, Johnson SC, Agesa KM, Shackelford KA, Tsoi D, Kievlan DR, et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: analysis for the Global Burden of Disease Study. Lancet. (2020) 395:200–11. doi: 10.1016/S0140-6736(19)32989-7
2. Weiss SL, Fitzgerald JC, Pappachan J, Wheeler D, Jaramillo-Bustamante JC, Salloo A, et al. Global epidemiology of pediatric severe sepsis: the sepsis prevalence, outcomes, and therapies study. Am J Respir Crit Care Med. (2015) 191:1147–57. doi: 10.1164/rccm.201412-2323OC
3. Liang L, Kotadia N, English L, Kissoon N, Ansermino JM, Kabakyenga J, et al. Predictors of mortality in neonates and infants hospitalized with sepsis or serious infections in developing countries: a systematic review. Front Pediatr. (2018) 6:277. doi: 10.3389/fped.2018.00277
4. Ruth A, McCracken CE, Fortenberry JD, Hall M, Simon HK, Hebbar KB. Pediatric severe sepsis: current trends and outcomes from the pediatric health information systems database. Pediatr Crit Care Med. (2014) 15:828–38. doi: 10.1097/PCC.0000000000000254
5. Prescott HC, Iwashyna TJ, Blackwood B, Calandra T, Chlan LL, Choong K, et al. Understanding and enhancing sepsis survivorship. Priorities for research and practice. Am J Respir Crit Care Med. (2019) 200:972–81. doi: 10.1164/rccm.201812-2383CP
6. Hotchkiss RS, Karl IE. The pathophysiology and treatment of sepsis. N Engl J Med. (2003) 348:138–50. doi: 10.1056/NEJMra021333
7. Prescott HC, Angus DC. Enhancing recovery from sepsis. JAMA. (2018) 319:62–75. doi: 10.1001/jama.2017.17687
8. Children: Improving Survival and Well-Being. Available online at: https://www.who.int/news-room/fact-sheets/detail/children-reducing-mortality (accessed May 28, 2021).
9. Bhandari N, Mazumder S, Taneja S, Sommerfelt H, Strand TA. Effect of implementation of integrated management of neonatal and childhood illness (IMNCI) programme on neonatal and infant mortality: cluster randomised controlled trial. BMJ. (2012) 344:e1634. doi: 10.1136/bmj.e1634
10. Weiss SL, Peters MJ, Alhazzani W, Agus MSD, Flori HR, Inwald DP, et al. Surviving sepsis campaign international guidelines for the management of septic shock and sepsis-associated organ dysfunction in children. Pediatric Critical Care Medicine. (2020) 21:e52. doi: 10.1097/PCC.0000000000002553
11. Davis AL, Carcillo JA, Aneja RK, Deymann AJ, Lin JC, Nguyen TC, et al. American college of critical care medicine clinical practice parameters for hemodynamic support of pediatric and neonatal septic shock. Crit Care Med. (2017) 45:1061–93. doi: 10.1097/CCM.0000000000002573
12. Riley C, Wheeler DS. Prevention of sepsis in children: a new paradigm for public policy. Crit Care Res Pract. (2011) 2012:e437139. doi: 10.1155/2012/437139
13. Baelani I, Jochberger S, Laimer T, Otieno D, Kabutu J, Wilson I, et al. Availability of critical care resources to treat patients with severe sepsis or septic shock in Africa: a self-reported, continent-wide survey of anaesthesia providers. Crit Care. (2011) 15:R10. doi: 10.1186/cc9410
14. Nwankwor OC, McKelvie B, Frizzola M, Hunter K, Kabara HS, Oduwole A, et al. A National survey of resources to address sepsis in children in tertiary care centers in Nigeria. Front Pediatr. (2019) 7:234. doi: 10.3389/fped.2019.00234
15. Kissoon N, Argent A, Devictor D, Madden MA, Singhi S, van der Voort E, et al. World federation of pediatric intensive and critical care societies-its global agenda. Pediatr Crit Care Med. (2009) 10:597–600. doi: 10.1097/PCC.0b013e3181a704c6
16. Slusher TM, Kiragu AW, Day LT, Bjorklund AR, Shirk A, Johannsen C, et al. Pediatric critical care in resource-limited settings—overview and lessons learned. Front Pediatr. (2018) 6:49 doi: 10.3389/fped.2018.00049
17. Turner EL, Nielsen KR, Jamal SM, von Saint André-von Arnim A, Musa NL. A review of pediatric critical care in resource-limited settings: a look at past, present, and future directions. Front Pediatr. (2016) 4:5. doi: 10.3389/fped.2016.00005
18. Wiens MO, Kumbakumba E, Kissoon N, Ansermino JM, Ndamira A, Larson CP. Pediatric sepsis in the developing world: challenges in defining sepsis and issues in post-discharge mortality. Clin Epidemiol. (2012) 4:319–25. doi: 10.2147/CLEP.S35693
19. Villamor E, Misegades L, Fataki MR, Mbise RL, Fawzi WW. Child mortality in relation to HIV infection, nutritional status, and socio-economic background. Int J Epidemiol. (2005) 34:61–8. doi: 10.1093/ije/dyh378
20. Biai S, Rodrigues A, Gomes M, Ribeiro I, Sodemann M, Alves F, et al. Reduced in-hospital mortality after improved management of children under 5 years admitted to hospital with malaria: randomised trial. BMJ. (2007) 335:862. doi: 10.1136/bmj.39345.467813.80
21. Thomas A, Lubarsky S, Durning SJ, Young ME. Knowledge syntheses in medical education: demystifying scoping reviews. Acad Med. (2017) 92:161–6. doi: 10.1097/ACM.0000000000001452
22. Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol Theory Pract. (2005) 8:19–32. doi: 10.1080/1364557032000119616
23. Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci. (2010) 5:69. doi: 10.1186/1748-5908-5-69
24. Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. (2018) 169:467–73. doi: 10.7326/M18-0850
25. Goldstein B, Giroir B, Randolph A. International consensus conference on pediatric sepsis. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med. (2005) 6:2–8. doi: 10.1097/01.PCC.0000149131.72248.E6
26. Sankar J, Moodu S, Kumar K, Sankar MJ, Kabra SK, Lodha R. Functional outcomes at 1 year after PICU discharge in critically ill children with severe sepsis. Pediatr Crit Care Med. (2021) 22:40–9. doi: 10.1097/PCC.0000000000002592
27. Farris RWD, Weiss NS, Zimmerman JJ. Functional outcomes in pediatric severe sepsis; further analysis of the RESOLVE trial. Pediatr Crit Care Med. (2013) 14:835–42. doi: 10.1097/PCC.0b013e3182a551c8
28. Nadel S, Goldstein B, Williams MD, Dalton H, Peters M, Macias WL, et al. Drotrecogin alfa (activated) in children with severe sepsis: a multicentre phase III randomised controlled trial. Lancet. (2007) 369:836–43. doi: 10.1016/S0140-6736(07)60411-5
29. Killien EY, Farris RWD, Watson RS, Dervan LA, Zimmerman JJ. Health-related quality of life among survivors of pediatric sepsis. Pediatr Crit Care Med. (2019) 20:501–9. doi: 10.1097/PCC.0000000000001886
30. Czaja AS, Zimmerman JJ, Nathens AB. Readmission and late mortality after pediatric severe sepsis. Pediatrics. (2009) 123:849–57. doi: 10.1542/peds.2008-0856
31. Zimmerman JJ, Banks R, Berg RA, Zuppa A, Newth CJ, Wessel D, et al. Trajectory of mortality and health-related quality of life morbidity following community-acquired pediatric septic shock. Crit Care Med. (2020) 48:329–37. doi: 10.1097/CCM.0000000000004123
32. Zimmerman JJ, Banks R, Berg RA, Zuppa A, Newth CJ, Wessel D, et al. Critical illness factors associated with long-term mortality and health-related quality of life morbidity following community-acquired pediatric septic shock. Crit Care Med. (2020) 48:319–28. doi: 10.1097/CCM.0000000000004122
33. Pinto NP, Berg RA, Zuppa AF, Newth CJ, Pollack MM, Meert KL, et al. Improvement in health-related quality of life after community acquired pediatric septic shock. Front Pediatr. (2021) 9:675374. doi: 10.3389/fped.2021.675374
34. Sidhu N, Joffe AR, Doughty P, Vatanpour S, Dinu I, Alton G, et al. Robertson CMT. Sepsis after cardiac surgery early in infancy and adverse 45-year neurocognitive outcomes. J Am Heart Assoc. (2015) 4:e001954. doi: 10.1161/JAHA.115.001954
35. Menon K, McNally JD, Zimmerman JJ, Agus MSD, O'Hearn K, Watson RS, et al. Primary outcome measures in pediatric septic shock trials: a systematic review. Pediatr Crit Care Med. (2017) 18:e146–54. doi: 10.1097/PCC.0000000000001078
36. Typpo KV, Petersen NJ, Hallman DM, Markovitz BP, Mariscalco MM. Day 1 multiple organ dysfunction syndrome is associated with poor functional outcome and mortality in the pediatric intensive care unit. Pediatr Crit Care Med. (2009) 10:562–70. doi: 10.1097/PCC.0b013e3181a64be1
37. Wiens MO, Pawluk S, Kissoon N, Kumbakumba E, Ansermino JM, Singer J, et al. Pediatric post-discharge mortality in resource poor countries: a systematic review. PLoS ONE. (2013) 8:e66698. doi: 10.1371/journal.pone.0066698
38. Sinha I, Jones L, Smyth RL, Williamson PR. A systematic review of studies that aim to determine which outcomes to measure in clinical trials in children. PLoS Med. (2008) 5:e96. doi: 10.1371/journal.pmed.0050096
39. Wooldridge G, Murthy S, Kissoon N. Core outcome set in paediatric sepsis in low- and middle-income countries: a study protocol. BMJ Open. (2020) 10:e034960. doi: 10.1136/bmjopen-2019-034960
40. Fink EL, Maddux AB, Pinto N, Sorenson S, Notterman D, Dean JM, et al. A core outcome set for pediatric critical care. Crit Care Med. (2020) 48:1819–28. doi: 10.1016/j.cct.2020.105968
41. Manning JC, Pinto NP, Rennick JE, Colville G, Curley MAQ. Conceptualizing post intensive care syndrome in children-the PICS-p framework. Pediatr Crit Care Med. (2018) 19:298–300. doi: 10.1097/PCC.0000000000001476
42. Watson RS, Choong K, Colville G, Crow S, Dervan LA, Hopkins RO, et al. Life after critical illness in children—toward an understanding of pediatric post-intensive care syndrome. J Pediatr. (2018) 198:16–24. doi: 10.1016/j.jpeds.2017.12.084
43. Watkins LA. Interventions for pediatric sepsis and their impact on outcomes: a brief review. Healthcare (Basel). (2018) 7:E2. doi: 10.3390/healthcare7010002
44. Stein RE, Jessop DJ. Functional status II(R). A measure of child health status. Med Care. (1990) 28:1041–55. doi: 10.1097/00005650-199011000-00006
45. Ong C, Lee JH, Leow MKS, Puthucheary ZA. Functional outcomes and physical impairments in pediatric critical care survivors: a scoping review. Pediatr Crit Care Med. (2016) 17:e247–259. doi: 10.1097/PCC.0000000000000706
46. Fiser DH. Assessing the outcome of pediatric intensive care. J Pediatr. (1992) 121:68–74. doi: 10.1016/S0022-3476(05)82544-2
47. Knoester H, Bronner MB, Bos AP. Surviving pediatric intensive care: physical outcome after 3 months. Intensive Care Med. (2008) 34:1076–82. doi: 10.1007/s00134-008-1061-4
48. Iwashyna TJ, Ely EW, Smith DM, Langa KM. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. (2010) 304:1787–94. doi: 10.1001/jama.2010.1553
49. Bronner MB, Knoester H, Sol JJ, Bos AP, Heymans HSA, Grootenhuis MA. An explorative study on quality of life and psychological and cognitive function in pediatric survivors of septic shock. Pediatr Crit Care Med. (2009) 10:636–42. doi: 10.1097/PCC.0b013e3181ae5c1a
50. Rennick JE, Johnston CC, Lambert SD, Rashotte JM, Schmitz N, Earle RJ, et al. Measuring psychological outcomes following pediatric intensive care unit hospitalization: psychometric analysis of the Children's Critical Illness Impact Scale. Pediatr Crit Care Med. (2011) 12:635–42. doi: 10.1097/PCC.0b013e3182191bfa
51. Davydow DS, Richardson LP, Zatzick DF, Katon WJ. Psychiatric morbidity in pediatric critical illness survivors: a comprehensive review of the literature. Arch Pediatr Adolesc Med. (2010) 164:377–85. doi: 10.1001/archpediatrics.2010.10
52. Conlon NP, Breatnach C, O'Hare BP, Mannion DW, Lyons BJ. Health-related quality of life after prolonged pediatric intensive care unit stay. Pediatr Crit Care Med. (2009) 10:41–4. doi: 10.1097/PCC.0b013e31819371f6
53. Aspesberro F, Mangione-Smith R, Zimmerman JJ. Health-related quality of life following pediatric critical illness. Intensive Care Med. (2015) 41:1235–46. doi: 10.1007/s00134-015-3780-7
54. Fiser DH, Long N, Roberson PK, Hefley G, Zolten K, Brodie-Fowler M. Relationship of pediatric overall performance category and pediatric cerebral performance category scores at pediatric intensive care unit discharge with outcome measures collected at hospital discharge and 1- and 6-month follow-up assessments. Crit Care Med. (2000) 28:2616–20. doi: 10.1097/00003246-200007000-00072
55. Pollack MM, Holubkov R, Glass P, Dean JM, Meert KL, Zimmerman J, et al. Functional Status Scale: new pediatric outcome measure. Pediatrics. (2009) 124:e18–28. doi: 10.1542/peds.2008-1987
56. Pollack MM, Holubkov R, Funai T, Clark A, Berger JT, Meert K, et al. Pediatric intensive care outcomes: development of new morbidities during pediatric critical care. Pediatr Crit Care Med. (2014) 15:821–7. doi: 10.1097/PCC.0000000000000250
57. Varni JW, Burwinkle TM, Seid M, Skarr D. The PedsQL 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambul Pediatr. (2003) 3:329–341. doi: 10.1367/1539-4409(2003)003<0329:TPAAPP>2.0.CO;2
58. Dossetor D, Liddle J, Mellis C. Measuring health outcome in paediatrics: development of the RAHC measure of function. J Paediatr Child Health. (1996) 32:519–24. doi: 10.1111/j.1440-1754.1996.tb00966.x
59. Polic B, Mestrovic J, Markic J, Mestrovic M, Capkun V, Utrobicic I, et al. Long-term quality of life of patients treated in paediatric intensive care unit. Eur J Pediatr. (2013) 172:85–90. doi: 10.1007/s00431-012-1843-0
60. Hordijk J, Verbruggen S, Vanhorebeek I, Van den Berghe G, Utens E, Joosten K, et al. Health-related quality of life of children and their parents 6 months after children's critical illness. Qual Life Res. (2020) 29:179–89. doi: 10.1007/s11136-019-02347-x
61. Boeddha NP, Schlapbach LJ, Driessen GJ, Herberg JA, Rivero-Calle I, Cebey-López M, et al. Mortality and morbidity in community-acquired sepsis in European pediatric intensive care units: a prospective cohort study from the European Childhood Life-threatening Infectious Disease Study (EUCLIDS). Crit Care. (2018) 22:143. doi: 10.1186/s13054-018-2052-7
62. Kissoon N, Carapetis J. Pediatric sepsis in the developing world. J Infect. (2015) 71 Suppl 1:S21–26. doi: 10.1016/j.jinf.2015.04.016
63. Abdelatif RG, Mohammed MM, Mahmoud RA, Bakheet MAM, Gima M, Nakagawa S. Characterization and outcome of two pediatric intensive care units with different resources. Crit Care Res Pract. (2020) 2020:e5171790. doi: 10.1155/2020/5171790
Keywords: quality of life, sepsis, functional outcomes, Pediatric Overall Cerebral Performance (POPC), Pediatric Cerebral Performance Category (PCPC), Pediatric Quality of Life
Citation: Ravikumar N, Sankar J and Das RR (2022) Functional Outcomes in Survivors of Pediatric Sepsis: A Scoping Review and Discussion of Implications for Low- and Middle-Income Countries. Front. Pediatr. 10:762179. doi: 10.3389/fped.2022.762179
Received: 21 August 2021; Accepted: 11 January 2022;
Published: 08 March 2022.
Edited by:
L. Nelson Sanchez-Pinto, Northwestern University, United StatesReviewed by:
Bo-tao Ning, Shanghai Children's Medical Center, ChinaYing Wang, Shanghai Children's Medical Center Affiliated to Medical College of Shanghai Jiaotong University Shanghai, China
Copyright © 2022 Ravikumar, Sankar and Das. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jhuma Sankar, jhumaji@gmail.com
 Namita Ravikumar
Namita Ravikumar Jhuma Sankar
Jhuma Sankar Rashmi Ranjan Das2
Rashmi Ranjan Das2