Associations of Dietary and Circulating Vitamin E Level With Metabolic Syndrome. A Meta-Analysis of Observational Studies
- 1Department of Orthopaedics, Xiangya Hospital, Central South University, Changsha, China
- 2National Clinical Research Center for Geriatric Disorders, Xiangya Hospital, Central South University, Changsha, China
- 3Changsha Social Work College, Changsha, China
- 4Center for Teaching and Research of Advanced Mathematics, School of Mathematics and Statistics, Central South University, Changsha, China
Objective: The associations of dietary and circulating vitamin E level with metabolic syndrome (MetS) remains conflicting. This meta-analysis of observational study was therefore employed to investigate the issue above.
Methods: The PubMed, Web of Science and Embase database were searched up to April 2021. The observational studies on the associations of dietary and circulating vitamin E level with MetS were specified. The pooled relative risk (RR) of MetS for the highest vs. lowest dietary and circulating vitamin E level, and the standard mean difference (SMD) of dietary and circulating vitamin E level for MetS vs. control subjects, were calculated.
Results: A total of 25 observational studies with 51,276 participants, were included in this meta-analysis. The overall multi-variable adjusted RR demonstrated that the dietary vitamin E level was inversely associated with MetS (RR = 0.92, 95%CI: 0.85–1.00; P = 0.044). In addition, the dietary vitamin E level in MetS was also lower than that in control subjects according to the overall combined SMD (SMD = −0.08, 95%CI: −0.14 to −0.02; P = 0.024). On the other hand, the overall multi-variable adjusted RR showed no significant relationship between the circulating vitamin E level and MetS (RR = 1.46, 95%CI: 0.85–2.48; P = 0.17). However, the circulating vitamin E level in MetS was lower than that in control subjects according to the overall combined SMD (SMD = −0.58, 95%CI: −1.04 to −0.13; P = 0.013).
Conclusions: The results of this meta-analysis suggest that the dietary vitamin E level is inversely associated with MetS. On the other hand, current evidence is still insufficient to conclude a relationship between the circulating vitamin E level and MetS. More well-designed prospective cohort studies are needed to address the issues further.
Introduction
Metabolic syndrome (MetS) is a pathological state characterized by the following clinical features: elevated waist circumference, blood pressure, fasting blood glucose, triglycerides and reduced high-density lipoprotein cholesterol (1). As a common risk factor for cardiovascular disease, diabetes and death, MetS has gradually become a major global public health issue (2). With the deepening of our knowledge, nutritional factors are considered to be involved in MetS (3–7).
As a fat-soluble vitamin with antioxidant properties, vitamin E is considered to be involved in signal transduction, gene expression and immunomodulatory capabilities (8). Higher vitamin E level was reported to be inversely associated with hypertension and diabetes (9–11). Moreover, a meta-analysis of randomized controlled trials demonstrated that vitamin E supplementation was beneficial for subclinical inflammation in adults (12). Experimental evidence also indicated that vitamin E supplementation could ameliorate hypertension and diabetes (13–15), and decrease the total serum cholesterol and lipid peroxides level (16) in animal model.
A number of observational studies have examined the associations of dietary and circulating vitamin E level with MetS. However, their results are still conflicting (17–41). The present meta-analysis of observational studies was therefore employed to address the issues. It was hypothesized that both dietary and circulating vitamin E was inversely associated with MetS.
Materials and Methods
Search Strategy
This meta-analysis was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines (42). The PubMed, Web of Science and Embase electronic database were searched during April 2021 by using a combination of keywords and in-text words related to metabolic syndrome (“metabolic syndrome”) and vitamin E (“vitamin E”, “tocopherol”) (43). No language restrictions were set in the search strategy. The titles and abstracts of all articles were screened firstly, and then the full articles were read to include the eligible studies. To identify the additional studies, the reference lists for the retrieved articles were also reviewed.
Study Selection
The titles, abstracts and full texts of all retrieved studies were reviewed by two researchers (YZ and DZZ) independently. Disagreements were resolved by discussions. The included studies were required to meet the following criteria: (1) observational studies; (2) the associations of dietary and circulating vitamin E level with MetS were reported; (3) relative risk (RR), odds ratio (OR) or standard mean difference (SMD) with 95% confidence interval (CI) were reported. The exclusion criteria were listed as follows: (1) duplicated or irrelevant articles; (2) reviews, letters or case reports; (3) randomized controlled trials; and (4) non-human studies.
Data Extraction
The data were extracted by two researchers (YZ and DZZ) independently, and disagreements were resolved by discussions. The information about first author, year of publication, location, age, gender, sample size, study design, adjustments, exposure, category of exposure, effect estimates and diagnostic criteria of MetS, was collected respectively. The corresponding effect estimates adjusted for the maximum number of confounding variables with 95% CIs for the highest vs. lowest dietary and circulating vitamin E level were extracted. Moreover, the dietary and circulating vitamin E level (mean ± SD) was also extracted to calculate the SMD (MetS vs. control).
Quality Assessment
Quality assessment was conducted according to the Newcastle-Ottawa (NOS) criteria for non-randomized studies, which was based on three broad perspectives: the selection process of study cohorts, the comparability among different cohorts and the identification of exposure or outcome of study cohorts. Disagreements with respect to the methodological quality were resolved by discussion and mutual-consultation. A study awarded seven or more stars was considered as a high-quality study (44).
Statistical Analyses
The RR for MetS and SMD for both dietary and circulating vitamin E level were the outcome measures in our study. The I2 statistic, which measures the percentage of total variation across studies due to heterogeneity, was examined (I2 > 50% was considered heterogeneity). If significant heterogeneity was observed among the studies, the random-effects model was used; otherwise, the fixed effects model was utilized. Begg's test was employed to assess the publication bias (45). A p-value < 0.05 was considered as statistically significant. Moreover, subgroup analysis was employed for both dietary and circulating vitamin E level, respectively.
Results
Study Identification and Selection
The detailed flow diagram of the study identification and selection was presented in Figure 1. A total of 873 potentially relevant articles (244 for PubMed, 327 for Embase and 302 for Web of Science) were retrieved during the initial literature search. After eliminating 331 duplicated articles, 542 articles were screened. 351 irrelevant studies were excluded according to the titles and abstracts. Then, 94 reviews, case reports or letters, 51 non-human studies, 27 randomized control trials studies were removed. Thereafter, 6 additional studies were acquired from the reference lists for the retrieved articles. Eventually, a total of 25 studies were selected for this meta-analysis (17–41).
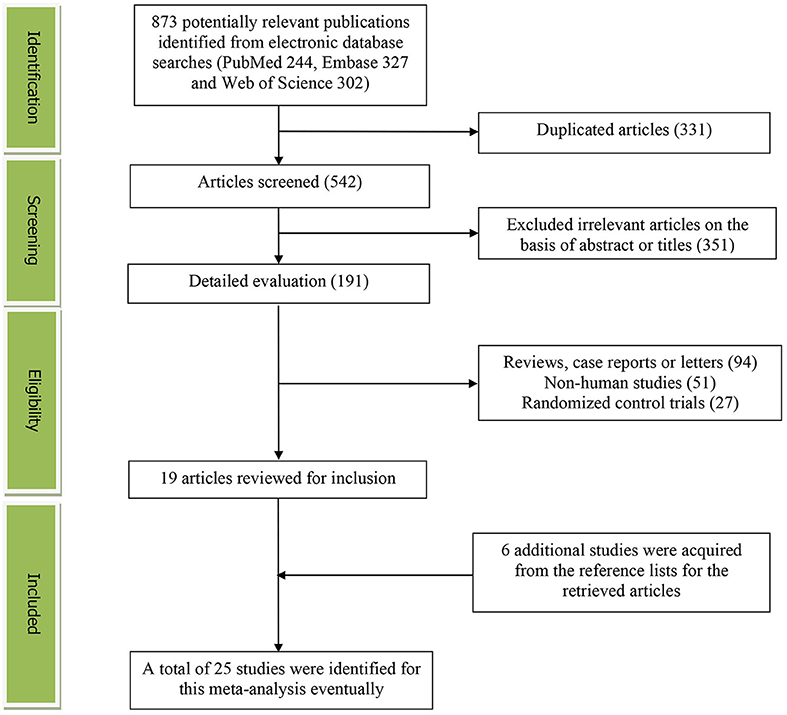
Figure 1. The detailed flow diagram of the study identification and selection in this meta-analysis.
Study Characteristics
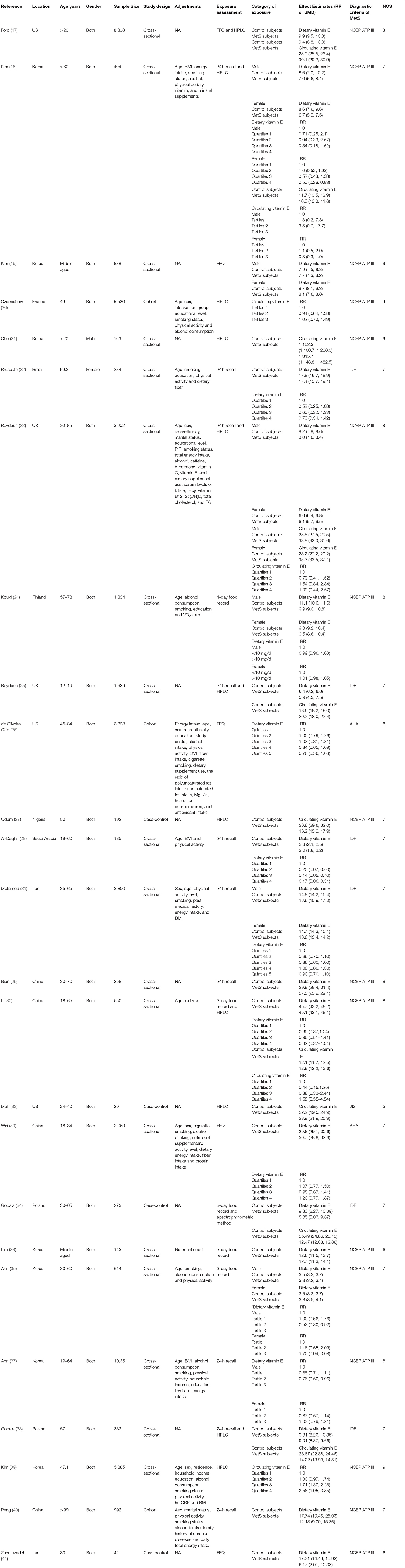
Table 1 showed the main characteristics of the included studies. These studies were published between 2003 and 2021. Among which, 14 studies were performed in Asian countries [Korea (18, 19, 21, 35–39), China (29, 30, 33, 40), Iran (31, 41) and Saudi Arabia (28)], and 4 ones were conducted in European countries [Poland (34, 38), France (20) and Finland (24)]. The other 7 studies were from US (17, 23, 25, 26, 32), Brazil (22) and Nigeria (27). Both male and female participants were considered in all included studies, except for Bruscate's and Cho's study (21, 22). The sample size ranged from 20 to 10,351 for a total number of 51,276. The dietary vitamin E level was assessed by food-frequency questionnaire (FFQ) in 5 studies (17, 19, 26, 33, 41), and 24 h or 3-day recall method in 18 studies (18, 20, 22, 23, 25, 27–32, 34–40), and 4-day record in 1 study (24). The circulating vitamin E level was assessed by high performance liquid chromatography (HPLC) in 11 studies (17, 18, 20, 21, 23, 25, 27, 30, 32, 38, 39), and spectrophotometric method in 1 study (34). The criteria for MetS were National Cholesterol Education Program-Adult Treatment Panel III (NCEP ATP III) in 16 (17–21, 23, 24, 27, 29, 30, 35–37, 39–41) and International Diabetes Federation (IDF) in 6 studies (22, 25, 28, 31, 34, 38). The others utilized American Heart Association (AHA) (26, 33) or Joint Interim Statement (JIS) (32), respectively.
RR of MetS for the Highest vs. Lowest Dietary Vitamin E Level
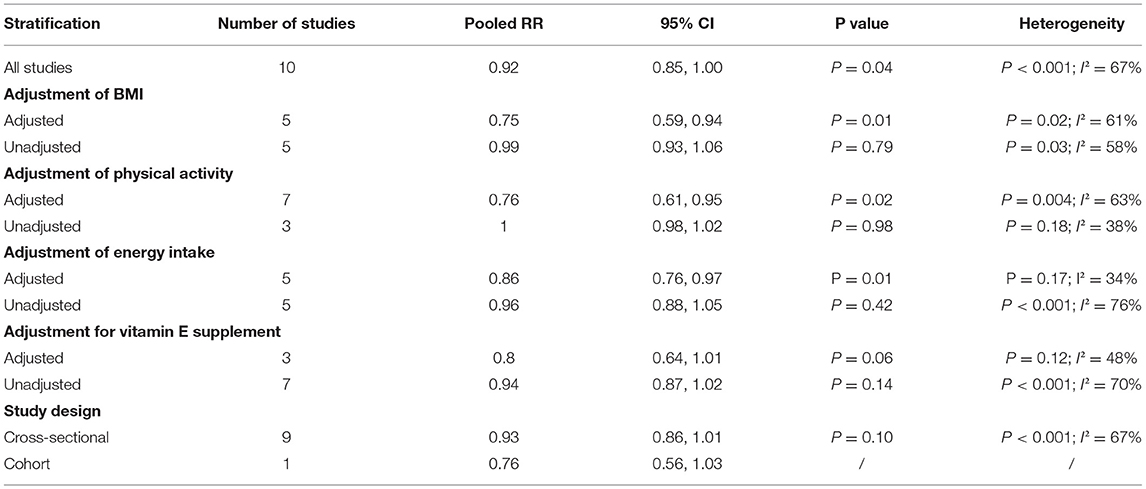
The overall multi-variable adjusted RR demonstrated that the dietary vitamin E level was negatively associated with MetS (RR = 0.92, 95%CI: 0.85–1.00; P = 0.044) (Figure 2). A substantial level of heterogeneity among various studies was obtained (P < 0.001, I2 = 67.1%). The Begg's rank-correlation test showed no evidence of publication bias (P = 0.189). The results of subgroup analysis were presented in Table 2. The aforementioned results only existed in studies with the adjustment of BMI (RR = 0.75, 95%CI: 0.59 to 0.94; P = 0.01), physical activity (RR = 0.76, 95%CI: 0.61–0.95; P = 0.02), and energy intake (RR = 0.86, 95%CI: 0.76–0.97; P = 0.01), respectively.
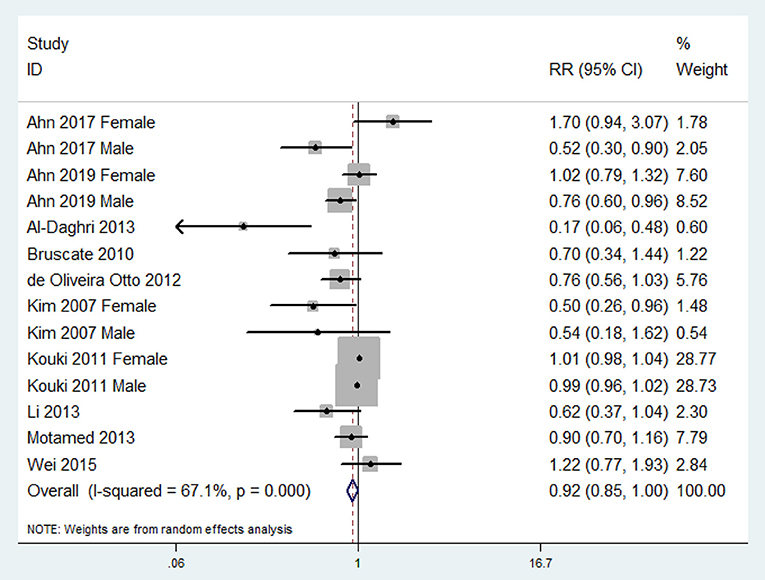
Figure 2. Forest plot of meta-analysis: Overall multi-variable adjusted RR of MetS for the highest vs. lowest category of dietary vitamin E level.
SMD of Dietary Vitamin E Level for MetS vs. Control Subjects
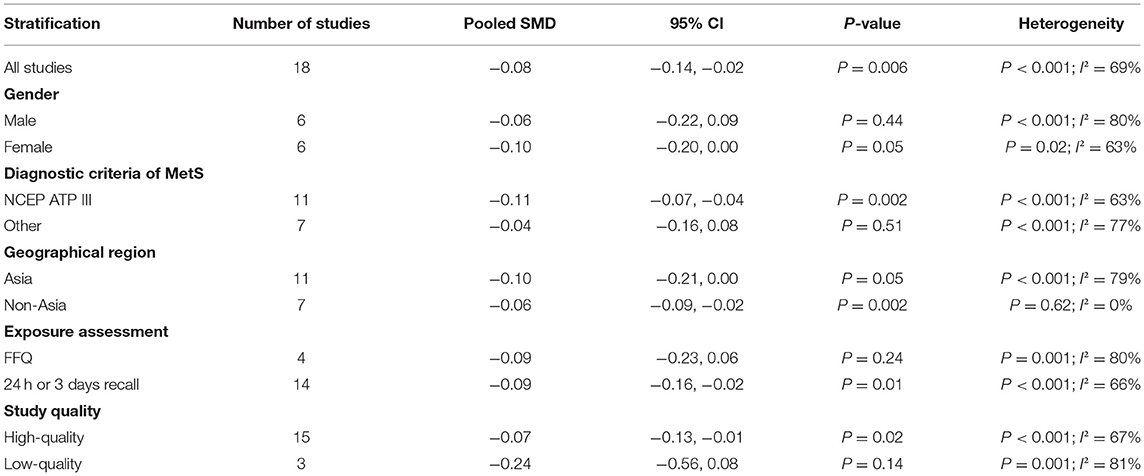
The overall combined SMD showed that the dietary vitamin E level in MetS was lower than that in control subjects (SMD = −0.08, 95%CI: −0.14 to −0.02; P = 0.006) (Figure 3). A substantial level of heterogeneity was obtained among the various studies (P < 0.001, I2 = 69.2%). The Begg's rank-correlation test showed no evidence of publication bias (P = 0.07). The results of subgroup analysis were presented in Table 3. The aforementioned results only existed in female (SMD = −0.10, 95%CI: −0.20 to 0.00; P = 0.05), NCEP ATP III (SMD = −0.11, 95%CI: −0.07 to −0.04; P = 0.002), 24 h or 3 days recall (SMD = −0.09, 95%CI: −0.16 to −0.02; P = 0.01) and high-quality (SMD = −0.07, 95%CI: −0.13 to −0.01; P = 0.02) studies, respectively.
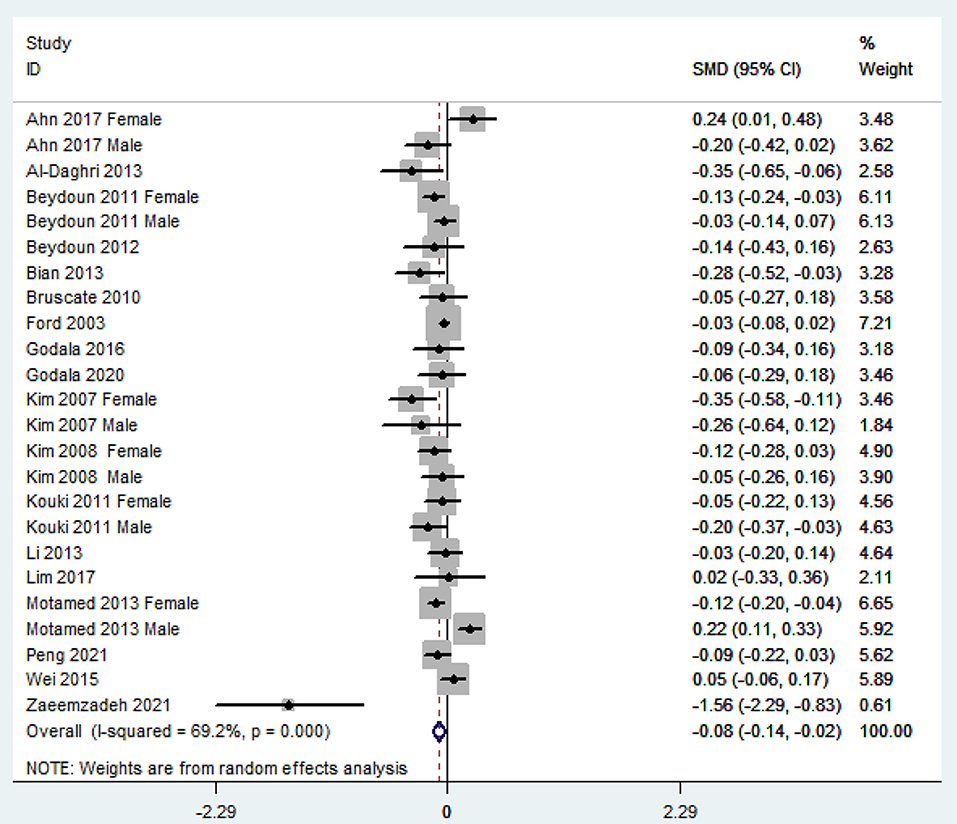
Figure 3. Forest plot of meta-analysis: SMD of dietary vitamin E level for MetS vs. control subjects.
RR of MetS for the Highest vs. Lowest Circulating Vitamin E Level
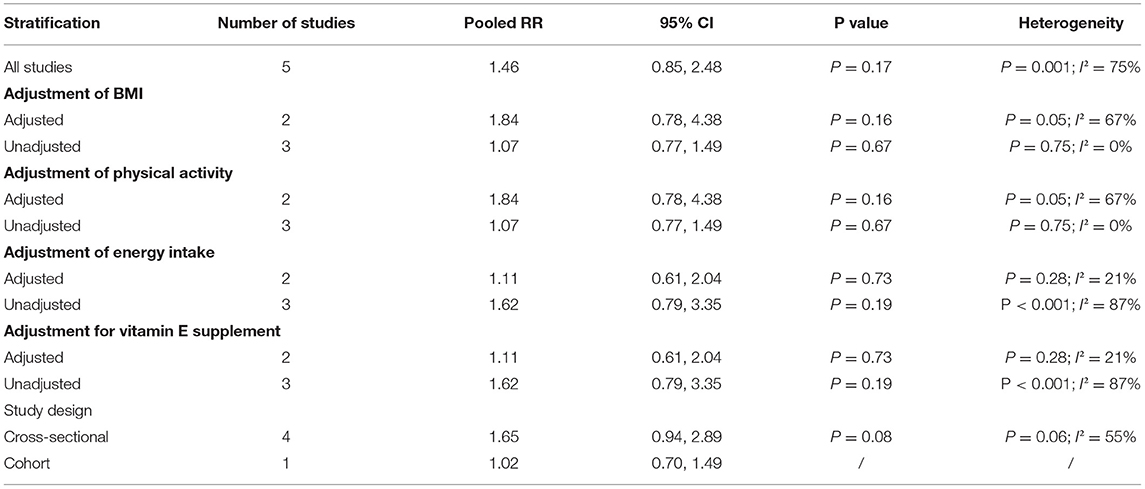
The overall multi-variable adjusted RR showed no significant relationship between circulating vitamin E level and MetS (RR = 1.46, 95%CI: 0.85–2.48; P = 0.168) (Figure 4). A substantial level of heterogeneity was obtained among various studies (P = 0.001, I2 = 75.2%). The Begg's rank-correlation test showed no evidence of publication bias (P = 0.707). The results of subgroup analysis were presented in Table 4.
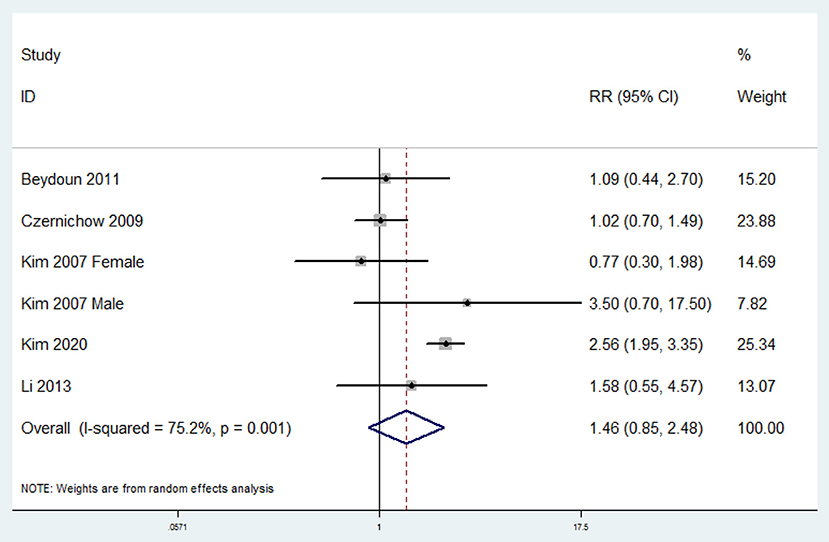
Figure 4. Forest plot of meta-analysis: Overall multi-variable adjusted RR of MetS for the highest vs. lowest category of circulating vitamin E level.
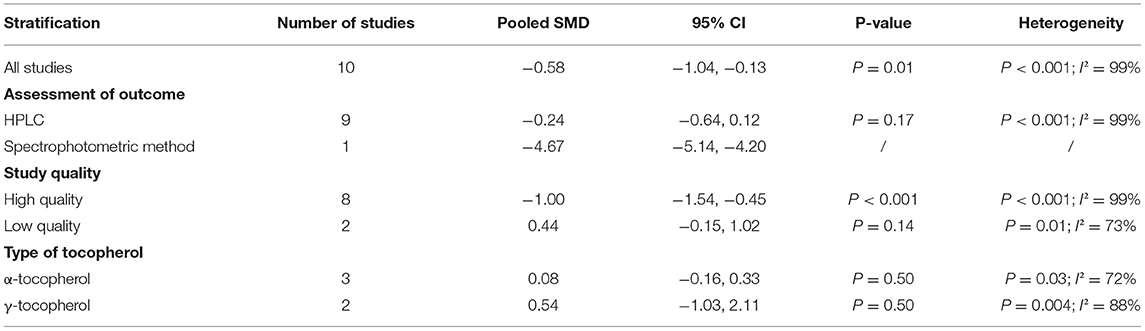
SMD of Circulating Vitamin E Level for MetS vs. Control Subjects
The overall combined SMD showed that the circulating vitamin E level in MetS was lower than that in control subjects (SMD = −0.58, 95%CI: −1.04 to −0.13; P = 0.013) (Figure 5). A substantial level of heterogeneity was obtained among the various studies (P < 0.001, I2 = 98.9%). The Begg's rank-correlation test showed no evidence of publication bias (P = 0.246). The results of subgroup analysis were presented in Table 5. The aforementioned results only existed in spectrophotometric method (SMD = −4.67, 95%CI: −5.14 to −4.20) and high-quality study (SMD = −1.00, 95%CI: −1.54 to −0.45; P < 0.001), but lost in α-tocopherol (SMD = 0.08, 95%CI: −0.16 to 0.33; P = 0.50) and γ-tocopherol (SMD = 0.54, 95%CI: −1.03 to 2.11; P = 0.50), respectively.
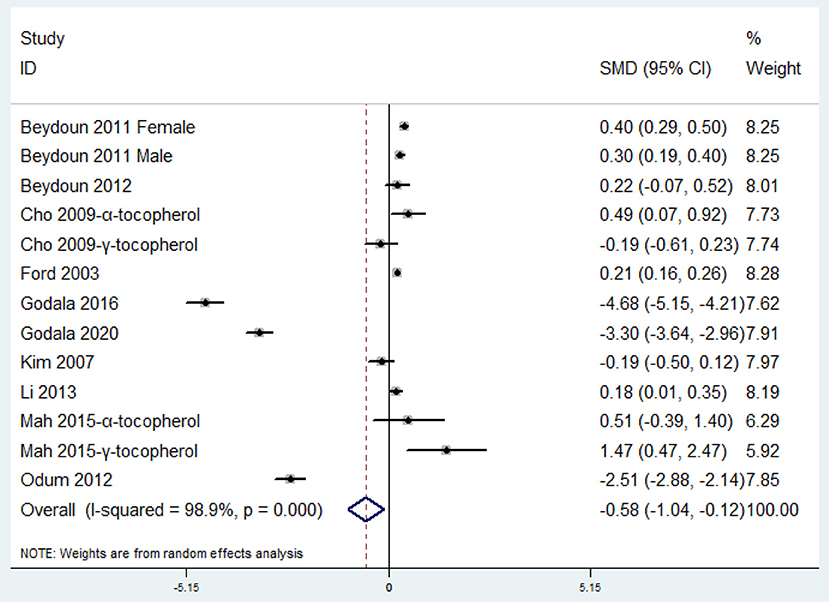
Figure 5. Forest plot of meta-analysis: SMD of circulating vitamin E level for MetS vs. control subjects.
Discussion
In the present meta-analysis, a total of 25 observational studies were identified for examination. The pooled analysis showed that the dietary vitamin E level was inversely associated with MetS.
Since both the oxidative stress and inflammation plays important role in the pathophysiology of MetS (46), the negative relationship between dietary vitamin E level and MetS may be mainly attributed to the antioxidant and anti-inflammatory property of vitamin E (12, 47, 48). Consistently, the clinical trial evidence demonstrates that the vitamin E supplementation may ameliorate MetS via anti-inflammation and anti-oxidative stress (49, 50). Moreover, some experimental animal studies have also indicated the beneficial impact of vitamin E intake on the MetS-related context (13–16). Nevertheless, very limited prospective cohort studies are identified for meta-analysis. The dietary vitamin E level is measured after MetS event occurs in cross-sectional/case-control studies. The factors that matter the dietary vitamin E level may change after MetS, which may reverse the causality. In addition, the significant heterogeneity has also been specified (I2 = 67.1%). Therefore, these above issues should be addressed by further well-designed prospective cohort studies.
In contrast to dietary vitamin E (a general/overall estimation that calculated from the FFQ or recall method), the issue of circulating vitamin E level is rather complicated. On one hand, vitamin E is composed of 8 similar structure compounds: 4 tocopherol and 4 tocotrienol derivatives including α-, β-, γ-, δ-tocopherol and tocotrienol, respectively. All vitamin E isomers from dietary or supplementary sources are absorbed and delivered to the liver. Only α-tocopherol is preferentially recognized by the α-tocopherol transfer protein for incorporation into circulating plasma, whereas the other tocopherol and tocotrienol isomers are mostly excreted (51, 52). Indeed, the concentration of tocotrienol is significantly lower than that of α-tocopherol (52). This is the main reason why α-tocopherol is currently severed as the standard to estimate human vitamin E requirements (53). However, it is increasingly acknowledged that tocopherol and tocotrienol serve different biological functions (tocotrienol may result in superior therapeutic properties than tocopherol), which has greatly challenged the accuracy of α-tocopherol estimation alone (54–56). Unfortunately, only several studies reported the exposure as “tocopherol” (21, 32, 39) (most studies reported the exposure as “circulating vitamin E” directly). The combination of tocopherol/tocotrienol may probably preclude a clear clarification for this issue. On the other hand, chronic inflammation and oxidative stress caused by MetS may lower the circulating antioxidant and anti-inflammatory agent level (57). In turn, the circulating antioxidant and anti-inflammatory agent level may also increase to cope with chronic inflammation and oxidative stress caused by MetS (58). As a consequence, the level of circulating vitamin E might be dynamic in MetS condition. Taken together, the specification of tocopherol/tocotrienol and potential feedback system should be considered for circulating vitamin E in further studies.
The epidemiological data has demonstrated that BMI, physical activity and energy intake is associated with both dietary vitamin E and MetS (59–63). Indeed, our finding is lost in studies without adjustment of these factors (Table 2). The adjustment of confounding factors can exclude the effect on both exposure and outcome (leave the direct relationship between vitamin E and MetS). Therefore, BMI, physical activity and energy intake may be adjusted when further study is employed. In addition, the lower dietary vitamin E level in MetS is only obtained in females, NCEP ATP III, 24 h or 3 days recall and high-quality studies (Table 3). Although females are more precise and reliable in completing the exposure assessment, some genetic gender differences with the diet-related pathology of MetS cannot be fully excluded (64). Moreover, the diagnostic criteria of MetS and exposure assessment may also influence the results. Since a substantial improvement may exist in laboratorial techniques to assess the circulating vitamin E level, a subgroup analysis for assessment method has also been employed. Interestingly, the results only exist in spectrophotometric method, but not HPLC. Notably, the spectrophotometric method is utilized in only one study (34). Taken together, more study with appropriate confounding factors adjustment and different circulating vitamin E assessment is needed.
The strengths of the present meta-analysis are mainly reflected in the following aspects: First, this is the first meta-analysis of observational studies on the associations of dietary and circulating vitamin E level with MetS. Second, our findings for dietary vitamin E level and MetS are consistence with current corresponding experimental and clinical studies. The limitations should also be acknowledged. First, the substantial level of heterogeneity might have distorted the reliability of our results (especially for circulating vitamin E level). Second, due to the limitation in the relevant literature, very few prospective cohort studies are identified totally (precluded causal relationships). Third, the classification of exposure vary greatly among individuals. For example, “tertiles,” “quartiles” and “quintiles” are employed to classify the dietary/circulating vitamin E level. Fourth, the selection of adjusted factors and definition of MetS are not uniform. Last but not the least, very few studies have considered the isomers of tocopherol/tocotrienol. These limitations may weaken the significance of this study.
Conclusions
The results of this meta-analysis suggest that the dietary vitamin E level may be inversely associated with MetS. On the other hand, current evidence is still insufficient to conclude a relationship between the circulating vitamin E level and MetS. More well-designed prospective cohort studies with the specification of circulating tocopherol/tocotrienol are needed to address the issues further.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author Contributions
YZ, DZ, and JL conceived the idea and drafted this meta-analysis. ZL and QL performed the statistical analysis. YL and JD selected and retrieved relevant papers. HG assessed each study. YZ, DZ, and JL was the guarantor of the overall content. All authors revised and approved the final manuscript.
Funding
This study was supported by National Natural Science Foundation of China (82102581), National Postdoctoral Science Foundation of China (2021M693562), Provincial Outstanding Postdoctoral Innovative Talents Program of Hunan (2021RC2020), Provincial Natural Science Foundation of Hunan (2019JJ40517), Young Investigator Grant of Xiangya Hospital, Central South University (2020Q14), and FuQing Postdoc Program of Xiangya Hospital, Central South University (176).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Zhang Y, Zhang DZ. Relationship between serum zinc level and metabolic syndrome: a meta-analysis of observational studies. J Am Coll Nutr. (2018) 37:708–15. doi: 10.1080/07315724.2018.1463876
2. Athyros V, Ganotakis E, Elisaf M, Mikhailidis D. The prevalence of the metabolic syndrome using the National Cholesterol Educational Program and International Diabetes Federation definitions. Curr Med Res Opin. (2005) 21:1157–9. doi: 10.1185/030079905X53333
3. Zhang Y, Zhang DZ. Relationship between nut consumption and metabolic syndrome: a meta-analysis of observational studies. J Am Coll Nutr. (2019) 38:499–505. doi: 10.1080/07315724.2018.1561341
4. Zhang Y, Zhang DZ. Associations of vegetable and fruit consumption with metabolic syndrome. A meta-analysis of observational studies. Public Health Nutr. (2018) 21:1693–703. doi: 10.1017/S1368980018000381
5. Guo HB, Ding J, Liang JY, Zhang Y. Associations of whole grain and refined grain consumption with metabolic syndrome. A meta-analysis of observational studies. Front Nutr. (2021) 8:695620. doi: 10.3389/fnut.2021.695620
6. Guo HB, Ding J, Liang JY, Zhang Y. Association of red meat and poultry consumption with the risk of metabolic syndrome: a meta-analysis of prospective cohort studies. Front Nutr. (2021) 8:691848. doi: 10.3389/fnut.2021.691848
7. Guo HB, Ding J, Liu Q, Li YS, Liang JY, Zhang Y. Vitamin C and metabolic syndrome: a meta-analysis of observational studies. Front Nutr. (2021) 8:728880. doi: 10.3389/fnut.2021.728880
8. Sherf-Dagan S, Buch A, Ben-Porat T, Sakran N, Sinai T. Vitamin E status among bariatric surgery patients: a systematic review. Surg Obes Relat Dis. (2021) 17:816–30. doi: 10.1016/j.soard.2020.10.029
9. Kuwabara A, Nakade M, Tamai H, Tsuboyama-Kasaoka N, Tanaka K. The association between vitamin E intake and hypertension: results from the re-analysis of the National Health and Nutrition Survey. J Nutr Sci Vitaminol. (2014) 60:239–45. doi: 10.3177/jnsv.60.239
10. Knekt P, Reunanen A, Marniemi J, Leino A, Aromaa A. Low vitamin E status is a potential risk factor for insulin-dependent diabetes mellitus. J Intern Med. (1999) 245:99–102. doi: 10.1046/j.1365-2796.1999.00416.x
11. Salonen JT, Nyyssönen K, Tuomainen TP, Mäenpää PH, Korpela H, Kaplan GA, et al. Increased risk of non-insulin dependent diabetes mellitus at low plasma vitamin E concentrations: a four year follow up study in men. BMJ. (1995) 311:1124–7. doi: 10.1136/bmj.311.7013.1124
12. Asbaghi O, Sadeghian M, Nazarian B, Sarreshtedari M, Mozaffari-Khosravi H, Maleki V, et al. The effect of vitamin E supplementation on selected inflammatory biomarkers in adults: a systematic review and meta-analysis of randomized clinical trials. Sci Rep. (2020) 10:17234. doi: 10.1038/s41598-020-73741-6
13. Vasdev S, Gill V, Parai S, Gadag V. Dietary vitamin e supplementation attenuates hypertension in Dahl salt-sensitive rats. J Cardiovasc Pharmacol Ther. (2005) 10:103–11. doi: 10.1177/107424840501000204
14. Noguchi T, Ikeda K, Sasaki Y, Yamamoto J, Yamori Y. Effects of vitamin E and sesamin on hypertension and cerebral thrombogenesis in stroke-prone spontaneously hypertensive rats. Clin Exp Pharmacol Physiol. (2004) 31:S24–6. doi: 10.1111/j.1440-1681.2004.04103.x
15. Kamimura W, Doi W, Takemoto K, Ishihara K, Wang D, Sugiyama H, et al. Effect of vitamin E on alloxan-induced mouse diabetes. Clin Biochem. (2013) 46:795–8. doi: 10.1016/j.clinbiochem.2013.02.016
16. Mardones P, Strobel P, Miranda S, Leighton F, Quiñones V, Amigo L, et al. α-Tocopherol metabolism is abnormal in scavenger receptor clas B type1 (SR-B1)-deficient mice. J Nutr. (2002) 132:443–9. doi: 10.1093/jn/132.3.443
17. Ford ES, Mokdad AH, Giles WH, Brown DW. The metabolic syndrome and antioxidant concentrations: findings from the Third National Health and Nutrition Examination Survey. Diabetes. (2003) 52:2346–52. doi: 10.2337/diabetes.52.9.2346
18. Kim MH, Lee HS, Park HJ, Kim WY. Risk factors associated with metabolic syndrome in Korean elderly. Ann Nutr Metab. (2007) 51:533–40. doi: 10.1159/000112977
19. Kim WY, Kim JE, Choi YJ, Huh KB. Nutritional risk and metabolic syndrome in Korean type 2 diabetes mellitus. Asia Pac J Clin Nutr. (2008) 17 Suppl 1:47–51.
20. Czernichow S, Vergnaud AC, Galan P, Arnaud J, Favier A, Faure H, et al. Effects of long-term antioxidant supplementation and association of serum antioxidant concentrations with risk of metabolic syndrome in adults. Am J Clin Nutr. (2009) 90:329–5l. doi: 10.3945/ajcn.2009.27635
21. Cho SW, Paek YM, Kang JY. Park Yk, Choi TI. The relationship between plasma antioxidant levels and metabolic syndrome risk factors in male workers. Korean J Food Nutr. (2009) 22:357–66.
22. Bruscato NM, Vieira J, Nascimento N, Canto M, Stobbe J, Gottlieb M G, et al. Dietary intake is not associated to the metabolic syndrome in elderly women. N Am J Med Sci. (2010) 2:182–8. doi: 10.4297/najms.2010.2182
23. Beydoun MA, Shroff MR, Chen X, Beydoun HA, Wang YF. Zonderman AB. Serum antioxidant status is associated with metabolic syndrome among US adults in recent national surveys. J Nutr. (2011) 141:903–13. doi: 10.3945/jn.110.136580
24. Kouki R, Schwab U, Hassinen M, Komulainen P, Heikkilä H, Lakka TA, et al. Food consumption, nutrient intake and the risk of having metabolic syndrome: the DR's EXTRA Study. Eur J Clin Nutr. (2011) 65:368–77. doi: 10.1038/ejcn.2010.262
25. Beydoun MA, Canas JA, Beydoun HA, Chen XL, Shroff MR. Zonderman AB. Serum antioxidant concentrations and metabolic syndrome are associated among US adolescents in recent national surveys. J Nutr. (2012) 142:1693–704. doi: 10.3945/jn.112.160416
26. de Oliveira Otto MC, Alonso A, Lee DH, Delclos GL, Bertoni AG, Jiang R, et al. Dietary intakes of zinc and heme iron from red meat, but not from other sources, are associated with greater risk of metabolic syndrome and cardiovascular disease. J Nutr. (2012) 142:526–33. doi: 10.3945/jn.111.149781
27. Odum EP, Orluwene CG, Ejilemele AA, Wakwe VC. Antioxidant status of subjects with Metabolic Syndrome in Port Harcourt, Nigeria. Niger Postgrad Med J. (2012) 19:199–203.
28. Al-Daghri NM, Khan N, Alkharfy KM, Al-Attas OS, Alokail MS, Alfawaz HA, et al. Selected dietary nutrients and the prevalence of metabolic syndrome in adult males and females in Saudi Arabia: a pilot study. Nutrients. (2013) 5:4587–604. doi: 10.3390/nu5114587
29. Bian S, Gao Y, Zhang M, Wang X, Liu W, Zhang D, et al. Dietary nutrient intake and metabolic syndrome risk in Chinese adults: a case-control study. Nutr J. (2013) 12:106. doi: 10.1186/1475-2891-12-106
30. Li Y, Guo H, Wu M, Liu M. Serum and dietary antioxidant status is associated with lower prevalence of the metabolic syndrome in a study in Shanghai, China. Asia Pac J Clin Nutr. (2013) 22:60–8. doi: 10.6133/apjcn.2013.22.1.06
31. Motamed S, Ebrahimi M, Safarian M, Ghayour-Mobarhan M, Mouhebati M, Azarpazhouh M, et al. Micronutrient intake and the presence of the metabolic syndrome. N Am J Med Sci. (2013) 5:377–85. doi: 10.4103/1947-2714.114171
32. Mah E, Sapper TN, Chitchumroonchokchai C, Failla ML, Schill KE, Clinton SK, et al. α-Tocopherol bioavailability is lower in adults with metabolic syndrome regardless of dairy fat co-ingestion: a randomized, double-blind, crossover trial. Am J Clin Nutr. (2015) 102:1070–80. doi: 10.3945/ajcn.115.118570
33. Wei J, Zeng C, Gong Q, Li X, Lei G, Yang T. Associations between dietary antioxidant intake and metabolic syndrome. PLoS ONE. (2015) 10:e0130876. doi: 10.1371/journal.pone.0130876
34. Godala MM, Materek-Kuśmierkiewicz I, Moczulski D, Rutkowski M, Szatko F, Gaszyńska E, et al. Lower plasma levels of antioxidant vitamins in patients with metabolic syndrome: a case control study. Adv Clin Exp Med. (2016) 25:689–700. doi: 10.17219/acem/41049
35. Ahn S, Jun S, Kang M, Shin S, Wie G, Baik HW, et al. Association between intake of antioxidant vitamins and metabolic syndrome risk among Korean adults. J Nutr Health. (2017) 50:313–24. doi: 10.4163/jnh.2017.50.4.313
36. Lim HS, Shin EJ, Yeom JW, Park YH, Kim SK. Association between Nutrient Intake and Metabolic Syndrome in Patients with Colorectal Cancer. Clin Nutr Res. (2017) 6:38–46. doi: 10.7762/cnr.2017.6.1.38
37. Ahn S, Jun S, Shin J, Ham D, Choi E, Joung H. Association between intake of antioxidant vitamins and metabolic syndrome prevalence among Korean adults. Curr Develop Nutr. (2019) 3:nzz044. doi: 10.1093/cdn/nzz044.P24-001-19
38. Godala M, Gaszyńska E, Moczulski D, Materek-Kuśmierkiewicz I, Krzyzak M. An assessment of the antioxidant vitamins concentration in people with metabolic syndrome working in agriculture. Med Pr. (2020) 23:128769. doi: 10.13075/mp.5893.01046
39. Kim T, Kang J. Association between serum retinol and α-tocopherol levels and metabolic syndrome in Korean general population: analysis of population-based nationally representative data. Nutrients. (2020) 12:1689. doi: 10.3390/nu12061689
40. Peng Z, Wang Y, Huang X, Zhu Q, Zhao Y, Xie H, et al. Dietary vitamin intake and risk of metabolic syndrome among centenarians in China. Exp Ther Med. (2021) 21:105. doi: 10.3892/etm.2020.9537
41. Zaeemzadeh N, Sadatmahalleh SJ, Ziaei S, Kazemnejad A, Movahedinejad M, Mottaghi A, et al. Comparison of dietary micronutrient intake in PCOS patients with and without metabolic syndrome. J Ovarian Res. (2021) 14:10. doi: 10.1186/s13048-020-00746-0
42. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. (2009) 339: b2700. doi: 10.1136/bmj.b2700
43. Bergin P, Leggett A, Cardwell CR, Woodside JV, Thakkinstian A, Maxwell AP, et al. The effects of vitamin E supplementation on malondialdehyde as a biomarker of oxidative stress in haemodialysis patients: a systematic review and meta-analysis. BMC Nephrol. (2021) 22:126. doi: 10.1186/s12882-021-02328-8
44. Yuhara H, Steinmaus C, Cohen S, Corley D, Tei Y, Buffler P. Is diabetes mellitus an independent risk factor for colon cancer and rectal cancer? Am J Gastroenterol. (2011) 106:1911–22. doi: 10.1038/ajg.2011.301
45. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. (1994) 50:1088–101. doi: 10.2307/2533446
46. Birben E, Sahiner UM, Sackesen C, Erzurum S, Kalayci O. Oxidative stress and antioxidant defense. World Allergy Organ J. (2012) 5:9–19. doi: 10.1097/WOX.0b013e3182439613
47. Spiteller G. Peroxyl radicals: inductors of neurodegenerative and other inflammatory diseases. Their origin and how they transform cholesterol, phospholipids, plasmalogens, polyunsaturated fatty acids, sugars, and proteins into deleterious products. Free Radic Biol Med. (2006) 41:362–87. doi: 10.1016/j.freeradbiomed.2006.03.013
48. Saboori S, Shab-Bidar S, Speakman JR. Rad EYousefi, Djafarian K. Effect of vitamin E supplementation on serum C-reactive protein level: a meta-analysis of randomized controlled trials. Eur J Clin Nutr. (2015) 69:867–73. doi: 10.1038/ejcn.2014.296
49. Pastor RF, Repetto MG, Lairion F, Lazarowski A, Merelli A, Carabetti ZM, et al. Supplementation with resveratrol, piperine and alpha-tocopherol decreases chronic inflammation in a cluster of older adults with metabolic syndrome. Nutrients. (2020) 12:3149. doi: 10.3390/nu12103149
50. Devaraj S, Leonard S, Traber MG, Jialal I. Gamma-tocopherol supplementation alone and in combination with alpha-tocopherol alters biomarkers of oxidative stress and inflammation in subjects with metabolic syndrome. Free Radic Biol Med. (2008) 44:1203–8. doi: 10.1016/j.freeradbiomed.2007.12.018
51. Traber MG, Vitamin E. Regulatory mechanisms. Annu Rev Nutr. (2007) 27:347–62. doi: 10.1146/annurev.nutr.27.061406.093819
52. Fairus S, Nor RM, Cheng HM, Sundram K. Alpha-tocotrienol is the most abundant tocotrienol isomer circulated in plasma and lipoproteins after postprandial tocotrienol-rich vitamin E supplementation. Nutr J. (2012) 11:5. doi: 10.1186/1475-2891-11-5
53. Food and Nutrition Board, Institute Institute of Medicine. Dietary Reference Intakes for Vitamin C, Vitamin E, Selenium and Carotenoids. Washington DC: National Academy Press (2000).
54. Theriault A, Jun-Tzu C, Wang Q, Gapor A, Adeli K. Tocotrienol: a review of its therapeutic potential. Clin Biochem. (1999) 32:309–19. doi: 10.1016/S0009-9120(99)00027-2
55. Sylvester PW, Theriault A. Role of tocotrienols in the preventive of cardiovascular disease and breast cancer. Curr Top Nutraceutical Res. (2003) 1:121–36.
56. Sen CK, Khanna S, Roy S. Tocotrienols: vitamin E beyond tocopherols. Life Sci. (2006) 78:2088–98. doi: 10.1016/j.lfs.2005.12.001
57. Seo JA, Song SW, Han K, Lee KJ, Kim HN. The associations between serum zinc levels and metabolic syndrome in the Korean population: Findings from the 2010 Korean national health and nutrition examination survey. PLoS ONE. (2014) 9:e105990. doi: 10.1371/journal.pone.0105990
58. Kim HN, Song SW, Choi WS. Association between serum zinc level and body composition: The Korean National Health and Nutrition Examination Survey. Nutrition. (2016) 32:332–7. doi: 10.1016/j.nut.2015.09.006
59. Zillikens MC, van Meurs J, Rivadeneira F, Hofman A, Oostra BA, Sijbrands E, et al. Interactions between dietary vitamin E intake and SIRT1 genetic variation influence body mass index. Am J Clin Nutr. (2010) 91:1387–93. doi: 10.3945/ajcn.2009.28627
60. Ejtahed H, Mahmoodi Z, Qorbani M, Angoorani P, Motlagh ME, Hasani-Ranjbar S, et al. A comparison between body mass index and waist circumference for identifying continuous metabolic syndrome risk score components in Iranian school-aged children using a structural equation modeling approach: the CASPIAN-V study. Eat Weight Disord. (2021) 26:1609–16. doi: 10.1007/s40519-020-00971-y
61. Kang M, Joo M, Hong H, Kang H. Eating speed, physical activity, and cardiorespiratory fitness are independent predictors of metabolic syndrome in Korean University Students. Nutrients. (2021) 13:2420. doi: 10.3390/nu13072420
62. Alghadir AH, Gabr SA, Anwer S, Li H. Associations between vitamin E, oxidative stress markers, total homocysteine levels, and physical activity or cognitive capacity in older adults. Sci Rep. (2021) 11:12867. doi: 10.1038/s41598-021-92076-4
63. Hermenegildo-López Y, Donat-Vargas C, Sandoval-Insausti H, Moreno-Franco B, Rodríguez-Ayala M, Rey-García J, et al. A Higher intake of energy at dinner is associated with incident metabolic syndrome: a prospective cohort study in older adults. Nutrients. (2021) 13:3035. doi: 10.3390/nu13093035
Keywords: dietary vitamin E, circulating vitamin E, metabolic syndrome, meta-analysis, observational studies
Citation: Zhang Y, Ding J, Guo H, Liu Z, Liu Q, Li Y, Zhang D and Liang J (2021) Associations of Dietary and Circulating Vitamin E Level With Metabolic Syndrome. A Meta-Analysis of Observational Studies. Front. Nutr. 8:783990. doi: 10.3389/fnut.2021.783990
Received: 27 September 2021; Accepted: 17 November 2021;
Published: 08 December 2021.
Edited by:
Alessio Molfino, Sapienza University of Rome, ItalyReviewed by:
Reza Rastmanesh, Independent Researcher, Tehran, IranMaria Maraki, National and Kapodistrian University of Athens, Greece
Copyright © 2021 Zhang, Ding, Guo, Liu, Liu, Li, Zhang and Liang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dianzhong Zhang, zdz1962@163.com; Jieyu Liang, jamesliang8@aliyun.com
 Yi Zhang
Yi Zhang Jun Ding3
Jun Ding3  Qi Liu
Qi Liu Yusheng Li
Yusheng Li Jieyu Liang
Jieyu Liang