Ocular Involvement in Coronavirus Disease 2019: Up-to-Date Information on Its Manifestation, Testing, Transmission, and Prevention
- 1State Key Laboratory of Ophthalmology, Zhongshan Ophthalmic Center, Sun Yat-sen University, Guangzhou, China
- 2Department of Geriatrics, The First Affiliated Hospital, Sun Yat-sen University, Guangzhou, China
The coronavirus disease 2019 (COVID-19) pandemic, caused by the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is still underway. An understanding of the virus's mode of transmission and infection is required for its effective containment. Besides the respiratory and digestive tracts, the ocular surface presents an additional mucosal surface that is exposed to infectious droplets and direct/indirect contact. The relationship between SARS-CoV-2 infection and the eye remains controversial. This review examines up-to-date information on ocular manifestation, laboratory testing, transmission, and prevention of COVID-19. Based on clinical observations, the risk of conjunctivitis in COVID-19 is low. Despite the low incidence, positive SARS-CoV-2 results in eye specimens suggest that the ocular surface may harbor SARS-CoV-2, which may increase the infection and transmission risk. We conclude that the ocular surface remains a potential transmission route for the virus that should not be ignored. In addition, the intraocular findings have also been described in COVID-19. The measures for eye and face protection should be widely adopted to stem the tide of the pandemic.
Introduction
Coronavirus disease 2019 (COVID-19) is caused by the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and has been recognized by the World Health Organization as a global pandemic. COVID-19 was first reported in Wuhan, China in December 2019 (1). As of May 31, 2020, COVID-19 has been confirmed to have affected more than 5,000,000 people with more than 300,000 deaths spanning most countries in the world (2). Coronaviruses have attracted worldwide attention since the outbreak of severe acute respiratory syndrome (SARS) in 2003, caused by the severe acute respiratory syndrome coronavirus (SARS-CoV) (3), and the Middle Eastern respiratory syndrome (MERS) in 2012, caused by the Middle Eastern respiratory syndrome coronavirus (MERS-CoV) (4). The ongoing COVID-19 global pandemic is a vivid reminder of the continuous evolution of microbes. SARS-CoV-2 shares 79.6% sequence identity with SARS-CoV (5). These two viruses bind to the same human cell receptor, namely, angiotensin-converting enzyme 2 (ACE2). Although these viruses are genetically related, SARS-CoV-2 is much more communicable than SARS-CoV (1). Human-to-human transmission of SARS-CoV-2 occurs mainly through respiratory droplets and direct/indirect contact via the mucous membranes. The ocular surface presents an additional mucosal surface that is exposed to infectious droplets and hand contact. Concerns have been raised over whether SARS-CoV-2 could be transmitted through ocular exposure or lead to ocular complications, following reports of a Chinese expert on COVID-19 who was not wearing eye protection during an inspection in Wuhan, and subsequently developed redness of the eyes several days before he was diagnosed with SARS-CoV-2 infection (6). In previous studies, several patients with COVID-19 were observed to exhibit ocular abnormalities (7–10). With the ongoing outbreak, mounting evidence suggests a relationship between SARS-CoV-2 infection and ocular involvement; however, it remains controversial. To analyze the evidence, we performed a review of the published literature and preprints in the following databases: PubMed, World of Science, ScienceDirect, the Cochrane Library, medRxiv, and bioRxiv. We searched for literature published from January 1, 2002 to May 31, 2020, to present up-to-date information on ocular involvement in COVID-19.
Ocular Manifestation in COVID-19 Patients
Seven kinds of human coronaviruses have been identified. Four of these, HCoV-229E, HCoV-NL63, HCoV-OC43, and HCoV-HKU1, generally cause only mild respiratory tract infections in humans (11, 12). The three most pathogenic human coronaviruses, SARS-CoV-2, SARS-CoV, and MERS-CoV more commonly cause life-threatening pneumonia and even death. Human coronaviruses and their association with ocular diseases have been discussed before. HCoV-NL63 was first isolated from the respiratory specimen of a 7-month-old child with bronchiolitis and conjunctivitis (11). In one study, 3/18 HCoV-NL63 patients (17%) <20 years of age had conjunctivitis (13). Loon et al. (14) detected SARS-CoV in the tears of 3/8 probable SARS patients (38%) in the early course of the disease (within 9 days of onset). However, in a case series reported by Chan et al. (15), neither tears nor conjunctival scraping samples were positive for SARS-CoV in any of the 17 patients confirmed to have SARS, and no virus-associated ocular complications were detected in these confirmed cases. Ocular involvement has not been described with human MERS-CoV infection.
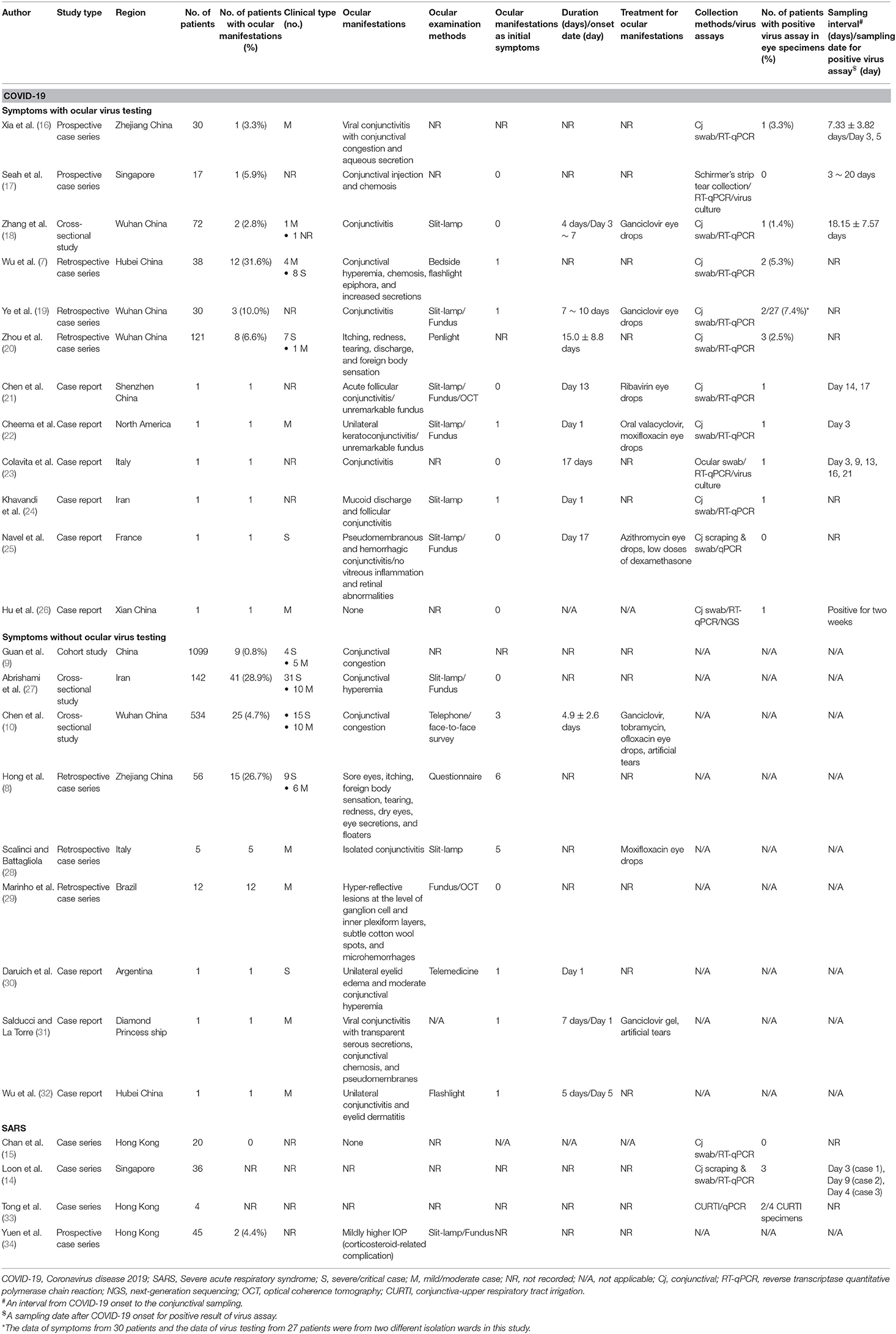
Since the beginning of the current outbreak, a growing amount of clinical reports of ocular manifestations in COVID-19 patients have been published (Table 1), more so than in SARS patients. The incidence of ocular manifestations in COVID-19 is varied and generally low (Table 1). The ocular manifestations described most commonly in COVID-19 patients, apart from discomforts, include unilateral or bilateral conjunctival congestion, hyperemia, chemosis, increased secretions, watery discharges, epiphora, or conjunctival follicles with (16, 18, 19, 21–25, 28, 31, 32) or without (7–10, 17, 20, 27, 30) a diagnosis of conjunctivitis by an ophthalmologist. Subconjunctival hemorrhage (25), pseudomembranes (25, 31), and impaired vision (22) were also reported, although less often. Ocular manifestation can present as an initial symptom (7, 8, 10, 19, 22, 24, 30–32), or an isolated symptom (28), in COVID-19.
Although the incidence is low, evidences show that SARS-CoV-2 can infect the ocular surface to cause conjunctivitis. Xia et al. (16) detected viral conjunctivitis in 1/30 COVID-19 patients (3.3%); the patient was a 53-year-old man with moderate COVID-19, conjunctival congestion, and aqueous secretion of the eyes, and SARS-CoV-2 nucleotides were detected in conjunctival swab samples. Zhang et al. (18) discovered that 2/72 COVID-19 patients (2.8%) had conjunctivitis; SARS-CoV-2 nucleotides were detected in the ocular discharges of one of these. The latter, a 29-year-old female nurse, working in an emergency department, presented with persistent bilateral conjunctival congestion, and watery discharges on day 2 with the onset of a moderate fever (day 1). Chen et al. (21) presented a case of a 30-year-old man with COVID-19 who had bilateral acute viral conjunctivitis of moderate hyperemia, a watery discharge, and inferior palpebral conjunctival follicles with a delayed onset (13 days after the onset of systemic disease), when conjunctival swab specimens were positive for SARS-CoV-2. The acute onset of the ocular manifestations with conjunctival hyperemia and watery discharges, and the positive virus testing of ocular samples indicated that it was viral conjunctivitis because of SARS-CoV-2 infection of the ocular surface.
However, not all studies reported the specific ocular manifestations related to SARS-CoV-2 infection (8–10, 27). The varying incidence in different reports may be attributed to the different methodology and varying definitions/criteria of conjunctivitis. Because of the risk to healthcare workers and the critical condition of patients, telemedicine, or penlight examinations were performed in some reported cases instead of slit-lamp microscopy and fundus examinations. Conjunctivitis is known to be a common ophthalmic manifestation with a variety of infectious or non-infectious causes (35). Conjunctivitis in a proportion of COVID-19 patients may have other viral, bacterial, or allergic causes and should be diagnosed differentially, especially in those cases lacking of ocular virus testing (28, 30, 32). The conjunctival congestion and chemosis, which mimic the symptoms of conjunctivitis, exhibited by COVID-19 patients (9, 27) may be related to mechanical ventilation, electrolyte disturbances, and fluid overload, especially in severe cases in intensive care units (ICUs) (36, 37). A study from Iran demonstrated that patients with COVID-19 in ICU were at an increased risk of developing chemosis (27). In addition, prolonged periods of reading during the isolation may be the cause of dry eye in COVID-19 patients (8, 10).
Another concern is that the cornea and intraocular tissues may be affected by COVID-19. Cheema et al. (22) reported a case of a 29-year-old female who was diagnosed with COVID-19 after initial presentation of unilateral keratoconjunctivitis with subepithelial infiltrates and overlying epithelial defects that spread diffusely through the entire cornea; a conjunctival swab sample was positive for SARS-CoV-2. Interestingly, it has been reported that ACE2 is expressed in the retina (38) and aqueous humor (39). Moreover, coronaviruses have been reported to cause retinopathy and optic neuritis in animal models (40). Marinho et al. (29) reported retinal and optical coherence tomography (OCT) changes in patients with COVID-19 and observed hyper-reflective lesions at the level of the ganglion cell and inner plexiform layers, with no visual disturbance or intraocular inflammation in either eye of any of the patients. However, the authors did not test for the SARS-CoV-2 virus in the aqueous humor or vitreous body of those patients. SARS-CoV-2 may target not only the ocular surface but also intraocular tissues; however, more researches are required to determine the scope of its ocular targets. It also suggests the importance of performing full eye examinations in COVID-19 patients.
As for the treatment, there is no proven specific therapy against ocular SARS-CoV-2 infection. Topical antiviral (ganciclovir, valacyclovir, or ribavirin) medicine, antibiotic medicine, corticosteroid eye drops, and artificial tears were applied in some reports (10, 18, 19, 21, 22, 25, 28, 31). However, the therapeutic effect of these medicine was required to be evaluated further. Most ocular manifestations in COVID-19 were mild, and recovered in a relatively short duration, without severe and sight-threatening complications detected (7, 18, 20, 21).
Laboratory Testing of SARS-COV-2 on the Ocular Surface
During the COVID-19 pandemic, a variety of nucleic acid and serological assays were established for the laboratory-based diagnosis of SARS-CoV-2 (41, 42). Ocular testing for SARS-CoV-2 is most commonly conducted by amplifying virus RNA using reverse transcription quantitative polymerase chain reaction (RT-qPCR) in conjunctival swabs samples or tear fluids. In a few studies, isolating the virus and culture were performed (17, 23). The primer sets used for RT-qPCR of the virus in the respiratory tract and in other specimens, targeting open reading frame 1ab, as well as the nucleocapsid, envelope, spike (S), and RNA-dependent RNA polymerase genes (41, 43), can also be used for ocular specimens. A cycle threshold (Ct) value of 40 or higher is interpreted as negative for SARS-CoV-2 RNA (44, 45). No immunoglobulin or cytokine tests for ocular specimens have been described, as far as we know.
Nucleic acid assays have demonstrated that SARS-CoV-2 can infect the ocular surface and cause conjunctivitis, yet the rate of RT-qPCR tests positive for SARS-CoV-2 RNA in ocular specimens appeared to be low (Table 1). Detection of SARS-CoV-2 in conjunctival or tear specimens may depend on viral load and shedding, as well as timing of sampling during the disease course. The SARS-CoV-2-positive conjunctival swab samples reported by Xia et al. (16) were obtained at the early stages of the disease, on days 3 and 5 after the onset of conjunctivitis. In the case reported by Chen et al. (21), the viral loads in conjunctival specimens collected on days 1 and 2 after conjunctivitis onset (Ct: 31) were much lower than those in nasopharyngeal (Ct: 23.52) and sputum (Ct: 25) specimens. The viral load decreased until it was undetectable on days 5 to 7 after conjunctivitis onset. Hence, we infer that SARS-CoV-2 is prone to exist on the ocular surface during the early stages of conjunctivitis, as verified in a study by Colavita et al. (23). They detected SARS-CoV-2 RNA in ocular swab specimens of a COVID-19 patient with conjunctivitis on days 3, 9, 13, 16, and 21 after symptom onset, even though it was undetectable in nasal swab specimens on day 19. Furthermore, they observed a cytopathic effect 5 days after inoculating Vero E6 cells with the first positive ocular specimen. These findings suggested that the ocular surface of SARS-CoV-2-positive patients may become infectious during the early stages of the disease (23). However, in a study by Seah et al. (17), Schirmer's test strips were used to collect tears on days 3 to 20 after the onset of systemic symptoms, and Vero E6 cells were inoculated with these samples for 4 days. Neither cytopathic effects in Vero E6 cells nor SARS-CoV-2 RNA was detected in 64 tear samples from 17 COVID-19 patients. Low viral loads (below the sensitivity of the tests) or inappropriate timing of sampling may have resulted in false-negative results. On the other hand, very low prevalence (0 ~ 7.4%) of ocular viral findings was reported in six studies with dozens to more than one hundred patients (Table 1). We cannot rule out the false-positive results due to the contamination with hands or testing items. Nevertheless, because SARS-CoV-2 infection is a life-threatening disease, further studies are required to clarify whether and how this virus could be transmitted through the eyes.
Meanwhile, it is noteworthy that SARS-CoV-2 nucleotides have been detected on the ocular surface of patients without ocular symptoms. Zhou et al. (20) discovered positive conjunctival swab samples for 3/121 patients, two of whom did not have ocular symptoms. Ye et al. (19) detected SARS-CoV-2 RNA in conjunctival specimens of 2/27 COVID-19 patients without conjunctivitis. Hu et al. (26) reported a case of a 70-year-old COVID-19 patient with a history of obstruction of the common lacrimal duct in his left eye but did not have conjunctivitis. Nasopharyngeal swab samples were positive for 22 days in this patient, yet ocular swab samples remained positive for 2 weeks after the former became negative. These cases indicate that the ocular surface may harbor SARS-CoV-2, where it may cause a latent and asymptomatic infection without entering the epithelial cells.
Transmission and Infection of SARS-COV-2 via the Eye
As indicated above, the ocular surface has been suggested as a potential target tissue for infection by SARS-CoV-2. However, in a review, Sun et al. (46) considered the ocular surface a less likely route of infection, because of the low prevalence of SARS-CoV-2 detected on the ocular surface and related conjunctivitis in COVID-19. They did, nevertheless, caution that the virus may be transmitted during ophthalmic practice. Peng et al. (47) stated that detection of SARS-CoV-2 RNA in tears and conjunctival secretions of COVID-19 patients with conjunctivitis may be a coincidence, rather than indicating SARS-CoV-2 infection of the conjunctiva as the cause of conjunctivitis.
The S protein of human coronaviruses is responsible for binding to host receptors and entry into host cells, by fusing the viral membrane with that of the host cell, a critical step for viral transmission and infection (48). The SARS-CoV-2 S protein has a receptor-binding domain with amino acids (49) that enhance binding to ACE2, and it has a higher affinity for ACE2 than the SARS-CoV S protein has (50). The S protein of SARS-CoV-2 binds to ACE2, after which it is cleaved and activated by transmembrane protease, serine 2 (TMPRSS2) (51). Moreover, it has been reported that the viral shedding pattern of SARS-CoV-2 appears different from that of SARS-CoV (45, 52). Compared with those of SARS-CoV, higher nasopharyngeal viral loads of SARS-CoV-2 were detected soon after the onset of symptoms (45, 52).
The distribution and expression of ACE2 in the human body may indicate potential infection routes of SARS-CoV-2. ACE2 is widely expressed, including in the lungs, oral and nasal mucosa, nasopharynx, ileum, colon, liver, and kidneys (53, 54). ACE2 and TMPRSS2 are also known to be expressed in the epithelium of the ocular surface. By single-cell RNA-sequencing of healthy donors, Sungnak et al. (54) determined that, in the eye, ACE2 was expressed in the conjunctival, corneal, and limbal epithelial cells; of these, ACE2 was co-expressed with TMPRSS2 in the conjunctival epithelial cells. However, it appeared to be inappropriate for the classification of cell types on the ocular surface in this study (54). The expression levels of these two genes were lower in the conjunctiva than in the lungs (54), which might indicate a lower risk for SARS-CoV-2 transmission through the ocular surface than via the respiratory tract. Based on immunostaining data of mice eyes and transcriptomic data of human conjunctival tissue, Zhang et al. (55) discovered that Ace2 and Tmprss2 were expressed in a similar pattern, with high levels in the mouse corneal epithelium, conjunctival epithelium, and lacrimal gland serous cells. The expression level of human ACE2 and TMPRSS2 was statistically significantly higher in the conjunctiva than in the cornea, which was consistent with the results in mice. In a study by Ma et al. (56), consistent expression of ACE2 was detected in human conjunctival and pterygium cell lines from some pterygium patients. The authors also discovered high expression levels of Ace2 and Tmprss2 in mouse corneas and suggested that the cornea, rather than conjunctiva, has the highest for SARS-CoV-2 infection. The distribution of ACE2 on the ocular surface indicates that SARS-CoV-2 may enter epithelial cells of the ocular surface and replicate there, as demonstrated by Hui and colleagues (57).They performed an ex vivo study using human conjunctival explant cultures, observing that these were more extensively infected by SARS-CoV-2 than by SARS-CoV, with higher infectious viral titers 48 h post infection. Thus, they provided direct evidence for the potential of the conjunctival epithelium to be a portal of infection for SARS-CoV-2. However, in a study by Lange et al. (58), ACE2, TMPRSS2, and other auxiliary mediators were not substantially expressed in healthy or diseased human conjunctival samples at the mRNA and protein level. Thus, the authors suggested that it is unlikely that SARS-CoV-2 infects the conjunctiva via ACE2 and its auxiliary mediators.
There is also anatomical evidence supporting the possibility that the ocular surface is a transmission route of SARS-CoV-2. The ocular surface, which comprises the tear film and the epithelia of the conjunctiva and cornea, is closely linked to the respiratory tract via the nasolacrimal system (59). Blinking spreads, mixes, and distributes tears and generates a pumping effect that draws tears into the lacrimal sac and then to the inferior meatus of the nose (59, 60). The nasolacrimal system therefore forms a route for viruses to spread between the eye and the upper respiratory tract. However, it is unknown in which direction SARS-CoV-2 would spread along this route. Tong et al. (33) exploited this connection, using conjunctiva-upper respiratory tract irrigation to test for the presence of SARS-CoV nucleotides. Patients self-administered one drop of saline to each eye, blinked repeatedly, tilted their head backward, and sniffed to facilitate drainage into the nasopharynx. In two of four confirmed SARS patients, these specimens tested positive, whereas none of the nasopharyngeal swab or stool specimens were positive. Deng et al. (61) performed a single conjunctival inoculation of 1 × 106 50% tissue culture infectious doses SARS-CoV-2 on two rhesus macaques, and the same was performed via the trachea in another macaque. They detected viral loads in conjunctival swab samples on the first day post inoculation (dpi) in macaques inoculated via the conjunctival route; on the days thereafter, the virus became undetectable in such samples. Viral loads were detected in nasopharyngeal swabs from 1 to 7 dpi in all three animals, while no viral loads were detected in conjunctival swab samples of macaques inoculated via the intratracheal route. Those infected via the conjunctival route had high viral loads in the nasolacrimal system and lower, localized viral loads in the lungs, whereas viral replication was highest in the lungs in those infected via the intratracheal route. These results indicated that rhesus macaques can be infected with SARS-CoV-2 by conjunctival exposure and the systemic condition may be mild. Deng et al. (61) also determined the viral distribution in more detail by euthanizing macaques and performing necropsies at 7 dpi. The results were directly supportive of the hypothesis that SARS-CoV-2 could infect ocular surface epithelial cells and drain into the nasopharyngeal tract via the nasolacrimal system. Although not investigating ocular exposure in isolation, others have studied SARS-CoV (62) and MERS-CoV (63, 64) infection in macaque models, which also indicated that the ocular surface might be a transmission route of human coronaviruses.
Prevention in Ophthalmology
The rapidly growing number of COVID-19 patients has prompted countries around the world to take measures to control and prevent the transmission of SARS-CoV-2. The ocular surface is a potential route of such transmission through the deposition of respiratory droplets on a surface followed by hand-eye contact, or through aerosolized droplets. Therefore, the potential need for the public and healthcare providers to protect their eyes should not be ignored, especially in areas with high infection rates. Patients with asymptomatic or presymptomatic infections may present to ophthalmologists with initial or isolated conjunctivitis associated with SARS-CoV-2. Therefore, such healthcare providers face an occupational risk during the pandemic. A couple of reports have provided guidance to ophthalmological clinics as precaution to protect patients and healthcare providers (65, 66).
Ophthalmological consultation and care have been altered, including the suspension of elective clinical services and the increased use of telemedicine. All patients and their companions are screened with non-contact thermometers and questionnaires at the entrance to the clinic. Symptoms of upper respiratory tract infections and acute conjunctivitis in patients have also been screened (37, 65, 67). Qiao et al. (68) reported an overall incidence rate of symptomatic COVID-19 infections among eye professionals in 10 hospitals in Wuhan was 2.52%. The authors highly recommended the use of personal protective equipment, a lack of which was one of the risk factors for symptomatic COVID-19 (68). It is important for healthcare workers to use face and eye protection and practice good hand hygiene, in order to protect exposed mucous membranes of the respiratory tract and ocular surfaces (69, 70). Personal protective equipment includes face masks (N95 respirators and surgical masks), goggles, face shields, and gloves (65, 66). To lower the risk of transmission via droplets, protective shields have been installed on slit lamps (67). The use of non-contact tonometry machines has been suspended to prevent possible aerosolization (67). Protective strategies have been recommended for cataract surgery, glaucoma care, corneal transplants, and the management of vitreoretinal diseases (71–74).
Conclusion
Transmission routes for human coronaviruses are still not completely elucidated. Despite the low prevalence of ocular manifestations compared with respiratory and other systemic disorders, SARS-CoV-2 may be able to infect the ocular surface or intraocular tissues. Further studies should therefore be performed on the interaction between SARS-CoV-2 and the human eye. As the ocular surface may be an additional transmission route, measures should be provided to protect patients' and healthcare workers' eyes from the virus to assist in stemming the tide of the pandemic. Ophthalmologists should take special precaution by wearing eye and face protection, practicing good hand hygiene, and avoiding direct/indirect mucosal contact with patients. Finally, the ocular surface might present a novel treatment route for vaccine delivery.
Author Contributions
ZC and GY collected the data as well as drafted and revised the manuscript. FD revised the manuscript. KW conceptualized and designed the study as well as reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agreed to be accountable for all aspects of the work.
Funding
This study was supported by funding from the National Natural Science Foundation of China (KW: 81770896; ZC: 81600710).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Abbreviations
COVID-19, coronavirus disease 2019; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; ACE2, angiotensin-converting enzyme 2; SARS-CoV, severe acute respiratory syndrome coronavirus; MERS-CoV-2, Middle Eastern respiratory syndrome coronavirus; RT-qPCR, reverse transcription quantitative polymerase chain reaction; Ct, cycle threshold; S, spike; TMPRSS2, transmembrane protease serine 2.
References
1. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. (2020) 395:497–506. doi: 10.1016/S0140-6736(20)30183-5
2. World Health Organization. Coronavirus disease (COVID-2019) Situation reports. WHO (2020). Available online at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/
3. Lee N, Hui D, Wu A, Chan P, Cameron P, Joynt GM, et al. A major outbreak of severe acute respiratory syndrome in Hong Kong. N Engl J Med. (2003) 348:1986–94. doi: 10.1056/NEJMoa030685
4. Zaki AM, van Boheemen S, Bestebroer TM, Osterhaus AD, Fouchier RA. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N Engl J Med. (2012) 367:1814–20. doi: 10.1056/NEJMoa1211721
5. Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. (2020) 579:270–3. doi: 10.1038/s41586-020-2012-7
6. Lu CW, Liu XF, Jia ZF. 2019-nCoV transmission through the ocular surface must not be ignored. Lancet. (2020) 395:e39. doi: 10.1016/S0140-6736(20)30313-5
7. Wu P, Duan F, Luo C, Liu Q, Qu X, Liang L, et al. Characteristics of ocular findings of patients with coronavirus disease 2019 (COVID-19) in Hubei Province, China. JAMA Ophthalmol. (2020) 138:575–8. doi: 10.1001/jamaophthalmol.2020.1291
8. Hong N, Yu W, Xia J, Shen Y, Yap M, Han W. Evaluation of ocular symptoms and tropism of SARS-CoV-2 in patients confirmed with COVID-19. Acta Ophthalmol. (2020). doi: 10.1111/aos.14445. [Epub ahead of print].
9. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. (2020) 382:1708–20. doi: 10.1056/NEJMoa2002032
10. Chen L, Deng C, Chen X, Zhang X, Chen B, Yu H, et al. Ocular manifestations and clinical characteristics of 534 cases of COVID-19 in China: a cross-sectional study. medRxiv [Preprint]. (2020) 20034678. doi: 10.1101/2020.03.12.20034678
11. van der Hoek L, Pyrc K, Jebbink MF, Vermeulen-Oost W, Berkhout RJ, Wolthers KC, et al. Identification of a new human coronavirus. Nat Med. (2004) 10:368–73. doi: 10.1038/nm1024
12. Woo PC, Lau SK, Chu CM, Chan KH, Tsoi HW, Huang Y, et al. Characterization and complete genome sequence of a novel coronavirus, coronavirus HKU1, from patients with pneumonia. J Virol. (2005) 79:884–95. doi: 10.1128/JVI.79.2.884-895.2005
13. Vabret A, Mourez T, Dina J, van der Hoek L, Gouarin S, Petitjean J, et al. Human coronavirus NL63, France. Emerg Infect Dis. (2005) 11:1225–9. doi: 10.3201/eid1108.050110
14. Loon SC, Teoh SC, Oon LL, Se-Thoe SY, Ling AE, Leo YS, et al. The severe acute respiratory syndrome coronavirus in tears. Br J Ophthalmol. (2004) 88:861–3. doi: 10.1136/bjo.2003.035931
15. Chan WM, Yuen KS, Fan DS, Lam DS, Chan PK, Sung JJ. Tears and conjunctival scrapings for coronavirus in patients with SARS. Br J Ophthalmol. (2004) 88:968–9. doi: 10.1136/bjo.2003.039461
16. Xia J, Tong J, Liu M, Shen Y, Guo D. Evaluation of coronavirus in tears and conjunctival secretions of patients with SARS-CoV-2 infection. J Med Virol. (2020) 92:589–94. doi: 10.1002/jmv.25725
17. Seah IYJ, Anderson DE, Kang AEZ, Wang L, Rao P, Young BE, et al. Assessing viral shedding and infectivity of tears in coronavirus disease 2019 (COVID-19) patients. Ophthalmology. (2020) 127:977–9. doi: 10.1016/j.ophtha.2020.03.026
18. Zhang X, Chen X, Chen L, Deng C, Zou X, Liu W, et al. The evidence of SARS-CoV-2 infection on ocular surface. Ocul Surf. (2020) 18:360–2. doi: 10.1016/j.jtos.2020.03.010
19. Ye Y, Song Y, Yan M, Hu C, Chen X, Yu J, et al. Novel coronavirus pneumonia combined with conjunctivitis: three cases report. Chin J Exp Ophthalmol. (2020) 38:242–4. doi: 10.3760/cma.j.issn.2095-0160.2020.0006
20. Zhou Y, Duan C, Zeng Y, Tong Y, Nie Y, Yang Y, et al. Ocular findings and proportion with conjunctival SARS-COV-2 in COVID-19 patients. Ophthalmology. (2020) 127:982–3. doi: 10.1016/j.ophtha.2020.04.028
21. Chen L, Liu M, Zhang Z, Qiao K, Huang T, Chen M, et al. Ocular manifestations of a hospitalised patient with confirmed 2019 novel coronavirus disease. Br J Ophthalmol. (2020) 104:748–51. doi: 10.1136/bjophthalmol-2020-316304
22. Cheema M, Aghazadeh H, Nazarali S, Ting A, Hodges J, McFarlane A, et al. Keratoconjunctivitis as the initial medical presentation of the novel coronavirus disease 2019 (COVID-19). Can J Ophthalmol. (2020) 55:e125–9. doi: 10.1016/j.jcjo.2020.03.003
23. Colavita F, Lapa D, Carletti F, Lalle E, Bordi L, Marsella P, et al. SARS-CoV-2 isolation from ocular secretions of a patient with COVID-19 in Italy with prolonged viral RNA detection. Ann Intern Med. (2020) 173:242–3. doi: 10.7326/M20-1176
24. Khavandi S, Tabibzadeh E, Naderan M, Shoar S. Corona virus disease-19 (COVID-19) presenting as conjunctivitis: atypically high-risk during a pandemic. Cont Lens Anterior Eye. (2020) 43:211–2. doi: 10.1016/j.clae.2020.04.010
25. Navel V, Chiambaretta F, Dutheil F. Haemorrhagic conjunctivitis with pseudomembranous related to SARS-CoV-2. Am J Ophthalmol Case Rep. (2020) 19:100735. doi: 10.1016/j.ajoc.2020.100735
26. Hu Y, Chen T, Liu M, Zhang L, Wang F, Zhao S, et al. Positive detection of SARS-CoV-2 combined HSV1 and HHV6B virus nucleic acid in tear and conjunctival secretions of a non-conjunctivitis COVID-19 patient with obstruction of common lacrimal duct. Acta Ophthalmol. (2020). doi: 10.1111/aos.14456. [Epub ahead of print].
27. Abrishami M, Tohidinezhad F, Daneshvar R, Omidtabrizi A, Amini M, Sedaghat A, et al. Ocular manifestations of hospitalized patients with COVID-19 in Northeast of Iran. Ocul Immunol Inflamm. (2020) 28:739–44. doi: 10.1080/09273948.2020.1773868
28. Scalinci SZ, Battagliola ET. Conjunctivitis can be the only presenting sign and symptom of COVID-19. IDCases. (2020) 20:e00774. doi: 10.1016/j.idcr.2020.e00774
29. Marinho PM, Marcos AAA, Romano AC, Nascimento H, Belfort R Jr. Retinal findings in patients with COVID-19. Lancet. (2020) 395:1610. doi: 10.1016/S0140-6736(20)31014-X
30. Daruich A, Martin D, Bremond-Gignac D. Ocular manifestation as first sign of Coronavirus disease 2019 (COVID-19): Interest of telemedicine during the pandemic context. J Fr Ophtalmol. (2020) 43:389–91. doi: 10.1016/j.jfo.2020.04.002
31. Salducci M, La Torre G. COVID-19 emergency in the cruise's ship: a case report of conjunctivitis. Clin Ter. (2020) 171:e189–91. doi: 10.7417/CT.2020.2212
32. Wu P, Liang L, Chen C, Nie S. A child confirmed COVID-19 with only symptoms of conjunctivitis and eyelid dermatitis. Graefes Arch Clin Exp Ophthalmol. (2020) 258:1565–66. doi: 10.1007/s00417-020-04708-6
33. Tong TR, Lam BH, Ng TK, Lai ST, Tong MK, Chau TN. Conjunctiva-upper respiratory tract irrigation for early diagnosis of severe acute respiratory syndrome. J Clin Microbiol. (2003) 41:5352. doi: 10.1128/JCM.41.11.5352.2003
34. Yuen KS, Chan WM, Fan DS, Chong KK, Sung JJ, Lam DS. Ocular screening in severe acute respiratory syndrome. Am J Ophthalmol. (2004) 137:773–4. doi: 10.1016/S0002-9394(03)01148-6
35. Azari AA, Barney NP. Conjunctivitis: a systematic review of diagnosis and treatment. JAMA. (2013) 310:1721–9. doi: 10.1001/jama.2013.280318
36. Grixti A, Sadri M, Edgar J, Datta AV. Common ocular surface disorders in patients in intensive care units. Ocul Surf. (2012) 10:26–42. doi: 10.1016/j.jtos.2011.10.001
37. Siedlecki J, Brantl V, Schworm B, Mayer WJ, Gerhardt M, Michalakis S, et al. COVID-19: ophthalmological aspects of the SARS-CoV 2 global pandemic. Klin Monbl Augenheilkd. (2020) 237:675–80. doi: 10.1055/a-1164-9381
38. Senanayake P, Drazba J, Shadrach K, Milsted A, Rungger-Brandle E, Nishiyama K, et al. Angiotensin II and its receptor subtypes in the human retina. Invest Ophthalmol Vis Sci. (2007) 48:3301–11. doi: 10.1167/iovs.06-1024
39. Holappa M, Valjakka J, Vaajanen A. Angiotensin(1-7) and ACE2, “The Hot Spots” of renin-angiotensin system, detected in the human aqueous humor. Open Ophthalmol J. (2015) 9:28–32. doi: 10.2174/1874364101509010028
40. Seah I, Agrawal R. Can the coronavirus disease 2019 (COVID-19) affect the eyes? a review of coronaviruses and ocular implications in humans and animals. Ocul Immunol Inflamm. (2020) 28:391–5. doi: 10.1080/09273948.2020.1738501
41. Yan Y, Chang L, Wang L. Laboratory testing of SARS-CoV, MERS-CoV, and SARS-CoV-2 (2019-nCoV): current status, challenges, and countermeasures. Rev Med Virol. (2020) 30:e2106. doi: 10.1002/rmv.2106
42. Long QX, Liu BZ, Deng HJ, Wu GC, Deng K, Chen YK, et al. Antibody responses to SARS-CoV-2 in patients with COVID-19. Nat Med. (2020) 26:845–8. doi: 10.1038/s41591-020-0897-1
43. Corman VM, Landt O, Kaiser M, Molenkamp R, Meijer A, Chu DK, et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. (2020) 25:2000045. doi: 10.2807/1560-7917.ES.2020.25.3.2000045
44. Wang W, Xu Y, Gao R, Lu R, Han K, Wu G, et al. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. (2020) 323:1843–4. doi: 10.1001/jama.2020.3786
45. Zou L, Ruan F, Huang M, Liang L, Huang H, Hong Z, et al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. (2020) 382:1177–9. doi: 10.1056/NEJMc2001737
46. Sun CB, Wang YY, Liu GH, Liu Z. Role of the eye in transmitting human coronavirus: what we know and what we do not know. Front Public Health. (2020) 8:155. doi: 10.3389/fpubh.2020.00155
47. Peng Y, Zhou YH. Is novel coronavirus disease (COVID-19) transmitted through conjunctiva? J Med Virol. (2020). doi: 10.1002/jmv.25753. [Epub ahead of print].
48. Wu A, Peng Y, Huang B, Ding X, Wang X, Niu P, et al. Genome composition and divergence of the novel coronavirus (2019-nCoV) originating in China. Cell Host Microbe. (2020) 27:325–8. doi: 10.1016/j.chom.2020.02.001
49. Wan Y, Shang J, Graham R, Baric RS, Li F. Receptor recognition by the novel coronavirus from Wuhan: an analysis based on decade-long structural studies of SARS coronavirus. J Virol. (2020) 94:e00127–20. doi: 10.1128/JVI.00127-20
50. Wrapp D, Wang N, Corbett KS, Goldsmith JA, Hsieh CL, Abiona O, et al. Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Science. (2020) 367:1260–3. doi: 10.1126/science.abb2507
51. Hoffmann M, Kleine-Weber H, Schroeder S, Kruger N, Herrler T, Erichsen S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. (2020) 181:271–80.e8. doi: 10.1016/j.cell.2020.02.052
52. Wolfel R, Corman VM, Guggemos W, Seilmaier M, Zange S, Muller MA, et al. Virological assessment of hospitalized patients with COVID-2019. Nature. (2020) 581:465–9. doi: 10.1038/s41586-020-2196-x
53. Hamming I, Timens W, Bulthuis ML, Lely AT, Navis G, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. a first step in understanding SARS pathogenesis. J Pathol. (2004) 203:631–7. doi: 10.1002/path.1570
54. Sungnak W, Huang N, Becavin C, Berg M, Queen R, Litvinukova M, et al. SARS-CoV-2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes. Nat Med. (2020) 26:681–7. doi: 10.1038/s41591-020-0868-6
55. Zhang BN, Wang Q, Liu T, Dou SQ, Qi X, Jiang H, et al. [Expression analysis of 2019-nCoV related ACE2 and TMPRSS2 in eye tissues]. Zhonghua Yan Ke Za Zhi. (2020) 56:438–46. doi: 10.3760/cma.j.cn112142-20200310-00170
56. Ma D, Chen CB, Jhanji V, Xu C, Yuan XL, Liang JJ, et al. Expression of SARS-CoV-2 receptor ACE2 and TMPRSS2 in human primary conjunctival and pterygium cell lines and in mouse cornea. Eye. (2020) 34:1212–9. doi: 10.1038/s41433-020-0939-4
57. Hui KPY, Cheung MC, Perera R, Ng KC, Bui CHT, Ho JCW, et al. Tropism, replication competence, and innate immune responses of the coronavirus SARS-CoV-2 in human respiratory tract and conjunctiva: an analysis in ex-vivo and in-vitro cultures. Lancet Respir Med. (2020) 8:687–95. doi: 10.1016/S2213-2600(20)30193-4
58. Lange C, Wolf J, Auw-Haedrich C, Schlecht A, Boneva S, Lapp T, et al. Expression of the COVID-19 receptor ACE2 in the human conjunctiva. J Med Virol. (2020). doi: 10.1002/jmv.25981. [Epub ahead of print].
59. Belser JA, Rota PA, Tumpey TM. Ocular tropism of respiratory viruses. Microbiol Mol Biol Rev. (2013) 77:144–56. doi: 10.1128/MMBR.00058-12
60. Garaszczuk IK, Montes Mico R, Iskander DR, Exposito AC. The tear turnover and tear clearance tests - a review. Expert Rev Med Devices. (2018) 15:219–29. doi: 10.1080/17434440.2018.1435271
61. Deng W, Bao L, Gao H, Xiang Z, Qu Y, Song Z, et al. Rhesus macaques can be effectively infected with SARS-CoV-2 via ocular conjunctival route. bioRxiv [Preprint]. (2020) 990036. doi: 10.1101/2020.03.13.990036
62. Lawler JV, Endy TP, Hensley LE, Garrison A, Fritz EA, Lesar M, et al. Cynomolgus macaque as an animal model for severe acute respiratory syndrome. PLoS Med. (2006) 3:e149. doi: 10.1371/journal.pmed.0030149
63. de Wit E, Rasmussen AL, Falzarano D, Bushmaker T, Feldmann F, Brining DL, et al. Middle east respiratory syndrome coronavirus (MERS-CoV) causes transient lower respiratory tract infection in rhesus macaques. Proc Natl Acad Sci USA. (2013) 110:16598–603. doi: 10.1073/pnas.1310744110
64. Munster VJ, de Wit E, Feldmann H. Pneumonia from human coronavirus in a macaque model. N Engl J Med. (2013) 368:1560–2. doi: 10.1056/NEJMc1215691
65. Olivia Li JP, Shantha J, Wong TY, Wong EY, Mehta J, Lin H, et al. Preparedness among ophthalmologists: during and beyond the COVID-19 pandemic. Ophthalmology. (2020) 127:569–72. doi: 10.1016/j.ophtha.2020.03.037
66. Hu VH, Watts E, Burton M, Kyari F, Mathenge C, Heidary F, et al. Protecting yourself and your patients from COVID-19 in eye care. Community Eye Health. (2020) 33:S1–6.
67. Lai THT, Tang EWH, Chau SKY, Fung KSC, Li KKW. Stepping up infection control measures in ophthalmology during the novel coronavirus outbreak: an experience from Hong Kong. Graefes Arch Clin Exp Ophthalmol. (2020) 258:1049–55. doi: 10.1007/s00417-020-04641-8
68. Qiao C, Zhang H, He M, Ying G, Chen C, Song Y, et al. Symptomatic COVID-19 in eye professionals in Wuhan, China. Ophthalmology. (2020) 127:1268–70. doi: 10.1016/j.ophtha.2020.04.026
69. Li JO, Lam DSC, Chen Y, Ting DSW. Novel coronavirus disease 2019 (COVID-19): the importance of recognising possible early ocular manifestation and using protective eyewear. Br J Ophthalmol. (2020) 104:297–8. doi: 10.1136/bjophthalmol-2020-315994
70. Seah I, Su X, Lingam G. Revisiting the dangers of the coronavirus in the ophthalmology practice. Eye. (2020) 34:1155–7. doi: 10.1038/s41433-020-0790-7
71. Jayaram H, Strouthidis NG, Gazzard G. The COVID-19 pandemic will redefine the future delivery of glaucoma care. Eye. (2020) 34:1203–5. doi: 10.1038/s41433-020-0958-1
72. Chandra A, Haynes R, Burdon M, Laidlaw A, Neffendorf J, Eames I, et al. Personal protective equipment (PPE) for vitreoretinal surgery during COVID-19. Eye. (2020) 34:1196–9. doi: 10.1038/s41433-020-0948-3
73. Shih KC, Wong JKW, Lai JSM, Chan JCH. The case for continuing elective cataract surgery during the COVID-19 pandemic. J Cataract Refract Surg. (2020) 46:921. doi: 10.1097/j.jcrs.0000000000000225
Keywords: COVID-19, SARS-CoV-2, ocular surface, manifestation, testing, transmission, prevention, conjunctivitis
Citation: Chen Z, Yuan G, Duan F and Wu K (2020) Ocular Involvement in Coronavirus Disease 2019: Up-to-Date Information on Its Manifestation, Testing, Transmission, and Prevention. Front. Med. 7:569126. doi: 10.3389/fmed.2020.569126
Received: 03 June 2020; Accepted: 30 October 2020;
Published: 30 November 2020.
Edited by:
Paolo Rama, San Raffaele Hospital (IRCCS), ItalyReviewed by:
Giulio Ferrari, San Raffaele Hospital (IRCCS), ItalyHaotian Lin, Sun Yat-sen University, China
Copyright © 2020 Chen, Yuan, Duan and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kaili Wu, wukaili@maill.sysu.edu.cn
†These authors have contributed equally to this work
 Ziyan Chen
Ziyan Chen Gang Yuan
Gang Yuan Fang Duan
Fang Duan Kaili Wu
Kaili Wu