- 1School of Tropical Medicine and Global Health, Nagasaki University, Nagasaki, Japan
- 2Institute of Tropical Medicine, Nagasaki University, Nagasaki, Japan
- 3Global Health Research and Medical Interventions for Development, Kathmandu, Nepal
- 4DEJIMA Infectious Disease Research Alliance Nagasaki University, Nagasaki, Japan
Dengue has become a recurrent and growing threat to public health in Nepal. The epidemic in 2022 was the largest ever reported, with cases being reported in all of the country’s seven provinces and 77 districts. Despite the establishment of an early-warning and reporting system (EWARS) in 1997, the lack of clear criteria for alarm signals and outbreak definitions in national guidelines delayed the epidemic declaration in 2022, which resulted in an increased number of cases and fatalities. For this article, we analyzed national data from previous years, which demonstrate that an epidemic could have been declared early in July, and that that would have resulted in fewer cases and fatalities if clear criteria for outbreak declarations had also been put in place. We also reviewed the existing national guidelines for dengue prevention and control, and propose recommendations to improve their implementation, particularly with regard to vector control measures. This article also highlights the need for a coordinated effort between multisector stakeholders, strengthened disease surveillance systems, and the establishment of predefined alarm signals and epidemic declaration criteria so that future epidemics are identified in a timely manner. The early outbreak warning system can potentially prevent future large outbreaks and minimize their negative impacts on the country’s health systems and economy.
Introduction
As of 30 November 2022, Nepal had reported 53,951 dengue cases with 62 deaths in that year (1). This cumulative number of cases is the largest ever reported and demonstrates that this is Nepal’s largest dengue epidemic to date. The first case of dengue in Nepal was detected in 2004 (2). Subsequently, periodic outbreaks were reported in 2010, 2013, 2016, and 2017, with the number of cases increasing from 686 to 2,111 per annum. A large outbreak occurred in 2019, with 17,992 cases being reported. In recent years, dengue cases have not only been reported in newer, more heavily populated districts, but also in the higher mountainous regions of the country, indicating that the infection has had an increased expansion. According to Nepal’s Ministry of Health and Population (MoHP), in 2022, for the first time, dengue infection was reported in all seven provinces and 77 districts (1). Kathmandu, the capital city of Nepal, with a population of approximately 1.5 million, was heavily affected by the epidemic, as cases reported within it constituted more than 55% of total number of cases reported in the country (1).
The 2022 epidemic was the largest dengue epidemic in the history of Nepal (1, 3). The Epidemiology and Disease Control Division (EDCD) at the MoHP’s Department of Health Services adopted a multisectoral approach and conducted “search and destroy” campaigns and public awareness activities to control dengue in response to this crisis. The EDCD led a virtual meeting with officials from the country’s provinces, districts, local governments, and other stakeholders, organized responses at district and local levels, and coordinated overall efforts to curb the increasing numbers of dengue cases (1, 4). For the “search and destroy” campaigns, the EDCD allocated budgets for 139 affected municipalities, 60 districts, and the country’s seven provinces. In the last week of August, district health offices in Lalitpur and Kathmandu intensified mass dengue search and destruction campaigns as well as awareness-raising activities in close collaboration with the metropolitan cities (4). Later, the campaign was expanded all over the country. However, owing to the inadequacy of vector surveillance and molecular study of circulating DENV serotypes and the inefficient early-warning system, it was difficult to precisely estimate the virus transmission across geographies and altitudes, and, in turn, failed to plan and implement the control measures in a timely manner.
Early warning and reporting of dengue outbreaks
Dengue infection in Nepal is recurrent, with cyclical outbreaks. There is also a high risk of secondary infection among infected individuals, which is indicated by an increasing number of severe dengue cases and case fatality rate (5). The World Health Organization (WHO) has reported that there has also been an increase in the incidence and geographical expansion of other vector-borne diseases (VBDs) in Nepal, such as chikungunya, leishmaniasis, and scrub typhus, which together with dengue, have had a serious impact on the country’s national health systems (5).
For early detection of cases and timely response to outbreaks, the EDCD established an Early-Warning and Reporting System (EWARS) in 1997, which now has 118 sentinel sites across Nepal that report the weekly status of epidemic-prone diseases [e.g., acute gastroenteritis, cholera, severe acute respiratory infection, dengue, malaria, and visceral leishmaniasis (kala-azar)] (6). EWARS has been reporting weekly dengue cases in recent years; however, it has not mentioned definite criteria for alarm signals and outbreak definitions in its guidelines that can send uniform messages to the concerning government and non-government public health organizations and to the general public (5).Through this article, we propose the use of “endemic channels” as a tool for early detection of dengue outbreaks in Nepal. We used the data published by EWARS from 2017 to 2021 to create Figure 1. It shows endemic channels: the “alarm zone” is the area between the two lines of the moving mean of the previous 5 years and the 2 standard deviations (2 SDs); the “secure zone” is the area between the moving mean and the −2 SDs; and the “epidemic zone” is the area above the alarm zone. The figure demonstrates that dengue cases increased above the secure zone (blue area) in March and crossed the alarm zone (orange area) in July 2022. We suggest that the alarms could have been triggered for the potential outbreak in March, and an epidemic could have been declared in early July. Just as they are in other countries, endemic channels can be a useful tool for the early detection of outbreaks in Nepal (7).
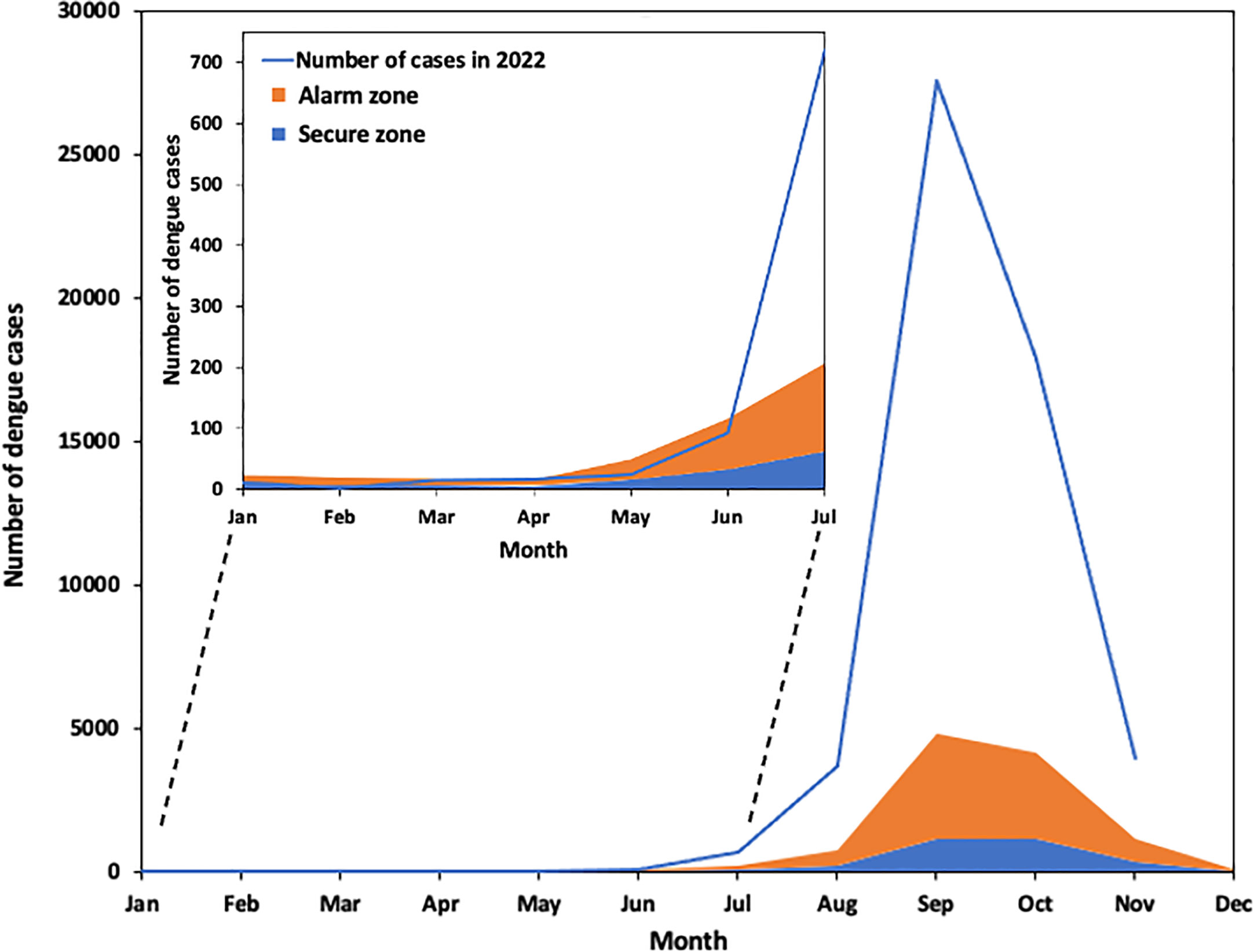
Figure 1 Outbreak detection using endemic channels. The x-axis and the y-axis show the months of year and the number of dengue cases reported in each month, respectively. The secure zone (blue area) is the area between the moving mean and 2 SDs (standard deviations) of the monthly number of dengue cases from 2017 to 2021. The alarm zone (orange area) is the area between the mean and +2 SDs. The area above the alarm zone is the epidemic zone. The number of cases in 2022 is shown by the blue line. It indicates that the number of cases increased above the secure zone in March and above the alarm zone in early July.
From this simple analysis of data from previous years, and its comparison with the current year’s data, the recent dengue epidemic could have been declared as early as July 2022. However, in absence of predefined criteria for an alarming signal, the EDCD delayed the declaration of an epidemic. Had an epidemic been declared in July 2022 and the concerned authorities taken intensive measures to mobilize resources for its control, the number of dengue cases and deaths could have been reduced dramatically. There is evidence that the failure, at the national and district levels, to respond to the alarm signals generated by EWARS has had a negative impact on the control of dengue epidemics (8).
Various modalities of early-warning systems (EWSs) are in place globally; the particular type used by each dengue-endemic country depends on its particular situation. The countries with high dengue burdens, that is, South America, Malaysia, Singapore, and many others, use the criteria of meteorological alarm indicators, particularly temperature and rainfall. Entomology alarm indicators, such as the Breteau index (BI), the house index (HI), the ovitrap index, and breeding percentage are also used (9). In other studies, population, dengue cases, and socioeconomic alarm indicators were used (9). The indicators take account of factors including population density, midyear population size, poverty index, GINI index, electricity access, drinking water access, sanitation index, and education coverage. Some studies have shown that the use of a combination of meteorological and epidemiological indicators, such as previous dengue cases, could represent the most effective method for predicting future dengue cases (10, 11). Scientists in Nepal should conduct research so that an accurate prediction model can be developed; it is probable that a model based on meteorological data and previous dengue cases would be most effective.
Climate change, unplanned urbanization, poor solid-waste management, easy transit between dengue-endemic regions, and limited public health resources are common reasons for dengue outbreaks in Nepal (12, 13). Although the Government of Nepal published the National Guidelines on Prevention, Management, and Control of Dengue in Nepal, in 2019, its implementation seems ineffective, particularly that of general preventive measures, such as vector management (1, 14). The current guidelines should be revised so that they incorporate all available epidemiological and clinical evidence. A simple, accessible clinical assessment and diagnostic tool should be developed for end users such as primary health care workers. Preventive dengue control strategies, such as vector control, should be another important topic in the guidelines. In particular, Nepal should proactively implement Aedes mosquito vector control measures, such as encouraging the use of antilarval and anti-adult sprays, publishing personal protection guidelines, and effecting legislative control in line with its national guidelines (14). Nepal should also learn lessons, both positive and negative, from other countries that have been engaged in decade-long battles with dengue (12, 15). For example, the Philippines government adopted environmental control measures, intensified chemical fogging, and reminded its citizens to follow the “4 o’clock habit” (i.e., emptying water containers, which are potential breeding sites for Aedes mosquitos, on a daily basis). New human vaccines against dengue infection and the potential use of bacteria called Wolbachia for vector control are other types of measures that are currently being researched and developed in some other countries.
In the context of a newly established federal government system, Nepal has an opportunity to strengthen its dengue prevention and control program, from the national to the local government levels. The revised national program should focus on case and vector surveillance in communities, the improvement of clinical and laboratory diagnosis capacities, and a protocol-based case management approach. Integrated vector management, early warning and reporting during outbreaks, health promotion and advocacy, and research are other areas for improvement. Furthermore, as climate change is responsible for the expansion of dengue toward new areas and altitudes, the EDCD’s vision should also incorporate environmental control measures, such as the search and destruction of potential breeding sites of Aedes mosquitos (16).
Conclusion
As a result of the 2022 dengue epidemic, Nepal’s health systems and economy were seriously, negatively impacted, and the densely populated city of Kathmandu was especially affected. To minimize the impact of these epidemics, the government should allocate resources to the improvement of disease surveillance systems. Predefined alarm signals and epidemic declaration criteria might help authorities to identify future epidemics in time. In addition, the development of a prediction model based on meteorological data and previous dengue cases could be an effective intervention in the context of climatic changes. Long-term vector control measures should be urgently and rigorously implemented, in coordination and collaboration with multisector stakeholders. The general public should be at the forefront of such control strategies, so that the negative impacts of future dengue epidemics can be reduced and the effectiveness of control programs sustained.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: https://www.edcd.gov.np/ewars; https://dohs.gov.np/category/annual-report/.
Ethics statement
The present work is a commentary and analysis of previously published public data and guidelines; therefore, ethics review was not applicable in this article. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
BD: literature search, data analysis, data interpretation, and preparation of the first draft. YH: data analysis and figure preparation. FD: revision of the first draft and figure preparation. SB: data collection, data interpretation and revision of the first draft. KA: data interpretation and revision of the first draft. BP: data interpretation, revision of the manuscript, and interpretation of the results. All authors contributed to the article and approved the submitted version.
Funding
It is funded by Japan Society for the Promotion of Health Sciences (JSPS) (Kakenhi Grant number: 22K15924). The funder did not have any role in the study design, data analysis, and report preparation.
Acknowledgments
The authors express their sincere gratitude toward the Ministry of Health and Population, Government of Nepal, and the Epidemiology and Disease Control Division (EDCD) for establishing the Early-Warning and Reporting System (EWARS) and making the data available for analysis.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
EDCD, Epidemiology and Disease Control Division, Government of Nepal; WHO, World Health Organization; EWARS, Early-Warning and Reporting System; SD, Standard Deviation.
References
1. Epidemiology and Disease Control Division. Situation updates of dengue (2022). Available at: https://edcd.ekbana.info/news/download/situation-updates-of-dengue-as-of-15-oct-2022 (Accessed Oct 16, 2022).
2. Rijal KR, Adhikari B, Ghimire B, Dhungel B, Pyakurel UR, Shah P, et al. Epidemiology of dengue virus infections in Nepal, 2006-2019. Infect Dis Poverty (2021) 10:1–10. doi: 10.1186/s40249-021-00837-0
3. Rimal S, Shrestha S, Pandey K, Nguyen TV, Bhandari P, Shah Y, et al. Co-Circulation of dengue virus serotypes 1, 2, and 3 during the 2022 dengue outbreak in Nepal: a cross-sectional study. Viruses (2023) 15(2):507. doi: 10.3390/v15020507
4. WHO Nepal. Responding to dengue outbreak in Nepal (2022). Available at: https://www.who.int/nepal/news/detail/24-10-2022-responding-to-dengue-outbreak-in-nepal (Accessed 10 June 2023).
5. WHO. Disease outbreak news: dengue fever-Nepal (2022). Available at: https://www.who.int/emergencies/disease-outbreak-news/item/2022-DON412 (Accessed Oct 12, 2022).
6. Epidemiology and Disease Control Division. A guide to early warning and reporting system (EWARS) (2019). Available at: https://edcd.ekbana.info/resources/download/a-guide-to-ewars-2019 (Accessed Oct 10, 2022).
7. WHO/TDR. Technical handbook for dengue surveillance, dengue outbreak prediction/detection and outbreak response (2016). Available at: https://apps.who.int/iris/handle/10665/250240 (Accessed Oct 5, 2022).
8. Benitez-Valladares D, Kroeger A, Tejeda GS, Hussain-Alkhateeb L. Validation of the early warning and response system (EWARS) for dengue outbreaks: evidence from the national vector control program in Mexico. PLoS Negl Trop Dis (2021) 15:e0009261. doi: 10.1371/journal.pntd.0009261
9. Baharom M, Ahmad N, Hod R, Abdul Manaf MR. Dengue early warning system as outbreak prediction tool: a systematic review. Risk Manag Healthc Policy (2022) 15:871–86. doi: 10.2147/RMHP.S361106
10. Jain R, Sontisirikit S, Iamsirithaworn S, Prendinger H. Prediction of dengue outbreaks based on disease surveillance, meteorological and socio-economic data. BMC Infect Dis (2019) 19:272. doi: 10.1186/s12879-019-3874-x
11. Hii YL, Zhu H, Ng N, Ng LC, Rocklöv J. Forecast of dengue incidence using temperature and rainfall. PLoS Negl Trop Dis (2012) 6(11):e1908. doi: 10.1371/journal.pntd.0001908
12. Adhikari S, Basnyat B, Maharjan K. Preparing for the dengue explosion in Kathmandu, Nepal. Lancet Glob Health (2020) 8:e331–e2. doi: 10.1016/S2214-109X(20)30007-3
13. Pandey BD, Pandey K, Dumre SP, Morita K, Costello A. Struggling with a new dengue epidemic in Nepal. Lancet Inf Dis (2022) 23(1):16–7. doi: 10.1016/S1473-3099(22)00798-8
14. Epidemiology and Disease Control Division. National guidelines on prevention, management and control of dengue in Nepal (2019). Available at: https://edcd.ekbana.info/resources/download/national-guidelines-of-prevention-control-and-management-of-dengue-in-nepal-2019-updated (Accessed Oct 5, 2022).
15. Ong EP, Obeles AJT, Ong BAG, Tantengco OAG. Perspectives and lessons from the philippines' decades-long battle with dengue. Lancet Reg Health West Pac (2022) 24:100505. doi: 10.1016/j.lanwpc.2022.100505
16. Ministry of Health and Population, Nepal. Vulnerability and adaptation assessment of climate sensitive diseases and health risks in Nepal (2022). Available at: https://mohp.gov.np/uploads/Resources/V%20%20A%20Assessment%20Report-MoHP-2022.pdf (Accessed May 22, 2023).
Keywords: dengue, Nepal, epidemic, EWARS, early detection, disease surveillance systems
Citation: Dhoubhadel BG, Hayashi Y, Domai FM, Bhattarai S, Ariyoshi K and Pandey BD (2023) A major dengue epidemic in 2022 in Nepal: need of an efficient early-warning system. Front. Trop. Dis 4:1217939. doi: 10.3389/fitd.2023.1217939
Received: 06 May 2023; Accepted: 15 June 2023;
Published: 25 July 2023.
Edited by:
Abhishek Pandey, Yale University, United StatesReviewed by:
Semeeh Omoleke, WHO Regional Office for the Eastern Mediterranean, EgyptCopyright © 2023 Dhoubhadel, Hayashi, Domai, Bhattarai, Ariyoshi and Pandey. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Suraj Bhattarai, surajbpkihs2012@gmail.com
 Bhim Gopal Dhoubhadel
Bhim Gopal Dhoubhadel Yumiko Hayashi
Yumiko Hayashi Fleurette Mbuyakala Domai
Fleurette Mbuyakala Domai Suraj Bhattarai
Suraj Bhattarai Koya Ariyoshi
Koya Ariyoshi Basu Dev Pandey
Basu Dev Pandey