Evaluation of children’s oral diagnosis and treatment using imaging examination using AI based Internet of Things
Abstract
BACKGROUND:
Although cone beam computed tomography (CBCT) plays an important role in the diagnosis and treatment of oral diseases, its image segmentation method needs to be further improved, and there are still objections about the clinical application effect of general anesthesia (GA) on children’s dental fear (CDF).
OBJECTIVE:
This study aimed to investigate the application value of CBCT based on intelligent computer segmentation model in oral diagnosis and treatment of children in the context of biomedical signals, and to analyze the alleviating effect of GA on CDF.
METHODS:
Based on the regional level set (CV) algorithm, the local binary fitting (LBF) model was introduced to optimize it, and the tooth CBCT image segmentation model CV-LBF was established to compare the segmentation accuracy (SA), maximum symmetric surface distance (MSSD), average symmetric surface distance (ASSD), over segmentation rate (OR), and under segmentation rate (UR) between these model and other algorithms. 82 children with CDF were divided into general anesthesia group (GAG) (
RESULTS:
The results showed that the
CONCLUSION:
The results revealed that the computer intelligent segmentation model CV-LBF has potential application value in CBCT image segmentation of children’s teeth, and GA can effectively alleviate anxiety of children with CDF and can be used as biomedical signals.
1.Introduction
As the oral part of the digestive system, teeth play an important role in food chewing and pronunciation [1]. In recent years, with the development of social economy and the improvement of people’s health concerns, oral health has attracted more and more attention. According to statistics, the annual number of oral diagnosis and treatment in China is about 300 million, the prevalence of oral diseases is as high as 97.6%, and only 0.22% of the adult population meets the oral health standards [2]. Oral health in children plays an active role in systemic nutritional intake and maxillofacial growth and development, and dental caries is the most common oral disease in children. The oral cavity’s development and maintenance, as well as the progression of oral diseases, are influenced by nutrition and diet. These factors play a significant role in the etiology and pathogenesis of oro-facial diseases and disorders. Nutrition and oral health are interdependent, and consuming foods that are rich in calcium and other nutrients such as leafy greens, almonds, cheese, milk, plain yogurt, and calcium-fortified tofu can benefit tooth health. Additionally, protein-rich foods like eggs, milk, poultry, fish, and meat are excellent sources of phosphorus. In trauma theory, protective factors are qualities, situations, or experiences that can help people or communities in protecting off, adjusting with, or recovering from the negative consequences of trauma. They consist of access to resources, resilience, a sense of control, social support, and positive self-image. These factors are important for developing resilience and are frequently the focus of interventions aimed at mitigating the negative effects of trauma. According to statistics, the prevalence of dental caries in children aged 3–5 years in China is as high as 66.0%, and the incidence of dental trauma in children aged 12 years is as high as 19.5% [3], but the visit rate and caries supplementation ratio are only 19.4% and 3.1% [4]. Because the root of the tooth is located in the alveolar bone, in order to accurately understand the tooth arrangement and root distribution and collision characteristics, dentists need to evaluate the tooth status of patients in detail based on imaging techniques, cone beam computed tomography (CBCT) technology can diagnose tooth, periodontal, and jaw diseases due to its advantages of high imaging accuracy and low artifact rate [5]; and in addition, it provides a reference basis for the selection of treatment options and prognosis, so it is used as a common means of diagnosis and treatment of oral diseases. CBCT can not only accurately measure root canal length and volume, root canal curvature, root inclination, but also show the anatomical shape of C-type root canals. In the process of traditional disease diagnosis, CT image segmentation is mainly completed by manual delineation by physicians, which is not only time-consuming, but also has low segmentation efficiency, and has obvious subjectivity [6]. In recent years, with the introduction of computer intelligence technology, CT image segmentation has evolved from traditional threshold algorithms to supervised or unsupervised computer intelligence algorithms [7]. Because there is obvious noise in CBCT images of teeth, the root part belongs to bone structure, which makes alveolar bone and root difficult to distinguish; and the distance between teeth is close, which is easy to produce adhesion on images, and a variety of computer intelligent algorithms can’t be directly applied in tooth segmentation. Horizontal set image method avoids the parameterization process of curve tracking and has potential advantages in tooth CT image segmentation [8]. A tooth CT image segmentation model is constructed based on edge level set algorithm. This model has high continuity and smoothness of the segmentation curve, but its segmentation gray distribution is not uniform and needs further optimization [9]. Uneven grey distribution in images can lead to inaccurate and unreliable segmentation, causing over or under-segmentation, sensitivity to lighting, and increased computational requirements.
The current study results suggested that the medical treatment rate of oral diseases in children in China was low, which was related to factors such as weak awareness of oral supervision by parents and long treatment time of oral diseases. Fear in children was one of the main reasons for low medical treatment rate, and age was inversely proportional to the incidence of anxiety in children [10]. According to statistics, about 48.4%
CHI-Net is a medical image segmentation network that utilizes a hierarchical context integration approach to accurately identify important regions in medical images. The network comprises two main modules, DDC and SRP, which work together to achieve superior performance compared to other existing methods for object segmentation in medical images [17]. CANet, a medical image segmentation network that incorporates a dual-stream pyramid module and an encoder-decoder module with context awareness. The network is designed to extract useful information from various medical images by combining these modules. The proposed network aims to improve medical image segmentation accuracy by leveraging the benefits of these different modules [18].
Although CBCT plays an important role in the diagnosis and treatment of oral diseases, its image segmentation method needs to be further improved, and there are still objections about the clinical application effect of GA in CDF. Therefore, based on the level set CT image segmentation method, through improving the algorithm, a tooth CBCT image computer intelligent segmentation model was established, and it was applied to the diagnosis and treatment of dental diseases in children to analyze the performance of the optimization algorithm in CBCT image segmentation. It aimed to investigate the effect of GA in CDF and provide some clinical basis for intelligent diagnosis and treatment of pediatric oral computer and selection of CDF intervention program.
2.Materials and methods
2.1Study subjects
82 children with CDF who were diagnosed and treated at the Yantai Mountain Hospital from December 2020 to March 2022 were selected as the study subjects. All children underwent CBCT, and the degree of dental anxiety was assessed using the children’s fear survey schedule-dental subscale (CFSS-DS) and Venham scale. Inclusion criteria: (1) children aged 3–6 years; (2) children with good general health; (3) children need to return to the dental clinic for many times; (4) CFSS-DS score higher than 34 points, (5) Venham grade
2.2Dental biomedical signal and image preprocessing
CBCT images during oral diagnosis and treatment in Yantai Mountain Hospital were collected and saved as DICOM standard format. All CBCT images were scanned by Italian NEWTOM VGi scanner. The scanning parameters were as follows: tube voltage 110 kV, current 2.81 mA, scanning field of vision 150 mm
For DICOM biological signal data, image gray value transformation was required. The specific operation method was as follows: window-adding method [19] was adopted to display the gray scale of DICOM format image, and linear mapping between the original gray scale value and the displayed gray scale was established according to the gray scale value of image. It establishes a linear mapping between the original grayscale values and the displayed grayscale. By selecting a specific range of grayscale values, called a window, and mapping it to the full display range, the method enhances the visibility of relevant image details. This allows healthcare professionals to better visualize anatomical structures or pathological features. The implementation of the window-adding method may vary depending on the software or viewer used, and different users may customize the window settings based on their specific requirements. Then, the full gray value of the original image can be expressed as follows.
(1)
The logarithmic transformation method of window function was adopted to map the gray scale of the image, and the gray scale value displayed in the window CBCT image is computed.
(2)
The CBCT image after gray value transformation needed to be processed by adaptive enhancement algorithm to improve the gray level balance of the image. CLAHE enhancement algorithm was used to process the image. CLAHE is an image enhancement technique that improves contrast and quality of digital images by dividing them into smaller tiles and applying histogram equalization to each tile individually. Unlike traditional histogram equalization, CLAHE applies the equalization to a limited range of intensity values within each tile and uses a clipping or limiting function to prevent over-enhancement and noise amplification. By combining the enhanced tiles, CLAHE produces an image with improved contrast and quality while avoiding artifacts and noise. The gray value
(3)
2.3Establishment of CBCT image intelligent segmentation model based on level set algorithm
CV model can accurately segment image edges and obtain global convergence, but it still has obvious defects when segmenting images with uneven gray distribution. However, they have significant limitations for images with an uneven gray distribution. Such images present difficulties for CV models, resulting in errors such as inaccurate edge detection, boundary placement, and sensitivity to local variations. The segmentation performance of these models is being actively enhanced by researchers in order to better handle uneven gray distribution and improve segmentation accuracy [20]. For the CBCT image after adaptive enhancement processing, if CV is used for processing, its level set energy function
(4)
Based on global information,
(5)
Local binary fitting (LBF) model can solve the problem of image segmentation accuracy with uneven gray scale, but it is highly dependent on the initial contour position [21]. LBF model is introduced into the local driving energy function of CV model to avoid the shortcomings of CV model in segmenting images with uneven gray distribution. The accuracy of the Local Binary Fitting (LBF) model for image segmentation in the presence of uneven grayscale depends greatly on the initial contour position. The model iteratively refines the contour based on local image information and prior knowledge of the object shape. Howeve an incorrect initial contour placement can lead to inaccurate segmentation. Therefore, selecting the optimal initial contour position is crucial to achieve precise segmentation results.
(6)
The regularization term is introduced in Eq. (6) to constrain the shape change of root canal segmentation contour, so the level set energy functions are expressed as follows.
(7)
(8)
(9)
(10)
The specific process of CV-LBF model segmentation of tooth CBCT image is shown in Fig. 1.
Figure 1.
Flowchart of CBCT images of teeth segmented by CV-LBF model.
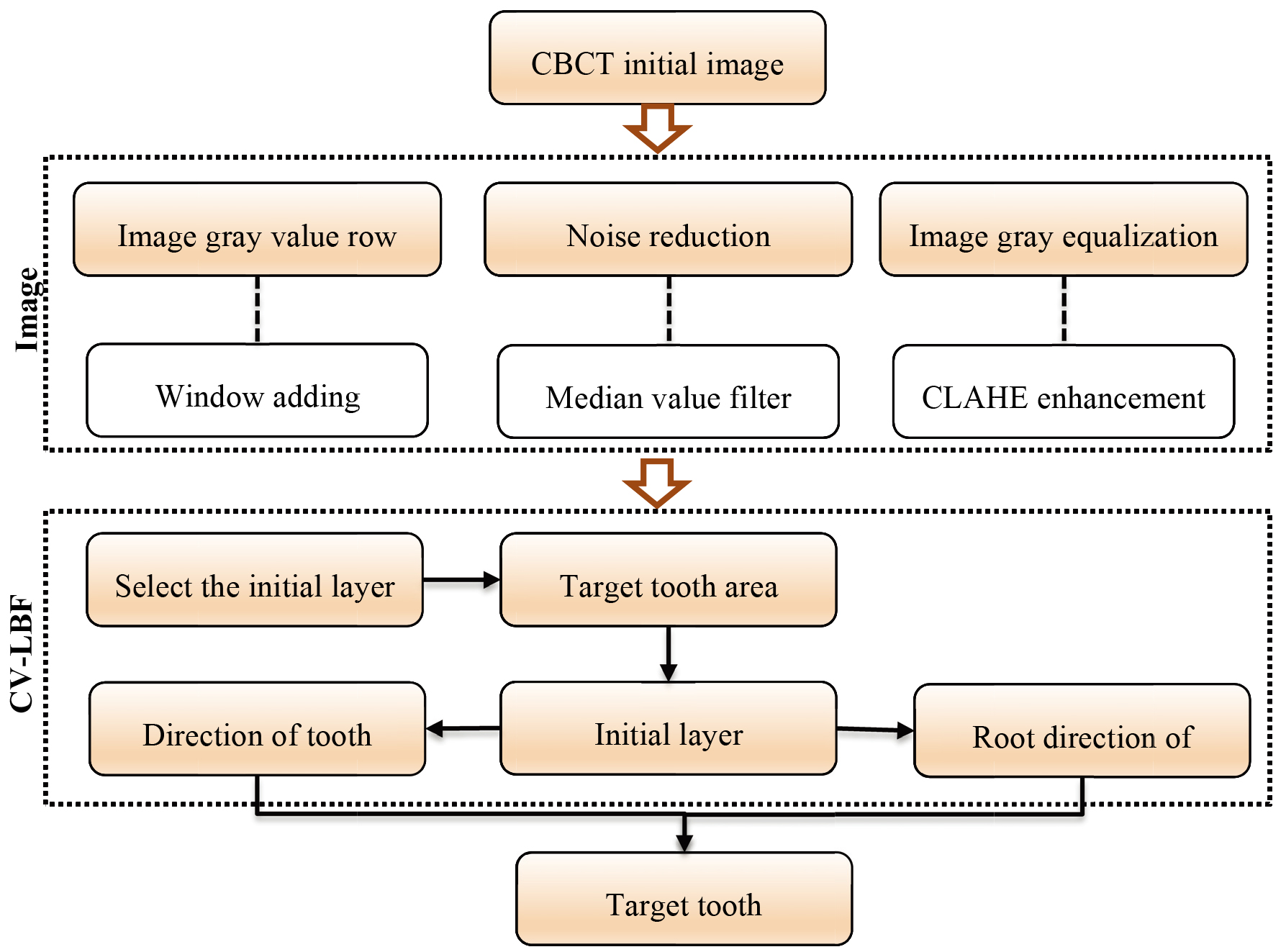
First, the windowing method is applied to transform the image gray value, the median filter is used to denoise the image, and the CLAHE enhancement algorithm to improve the gray balance of CBCT image. The median filter reduces noise in images by replacing each pixel with the median value of its neighboring pixels, making it effective at removing isolated noisy pixels without affecting the image details and edges. Its adaptability to the local image structure, rather than a fixed kernel size, helps preserve the image quality. An appropriate initial layer image is selected to obtain a small window area containing the target teeth. The level set segmentation method is adopted to perform the initial layer results. In children’s oral diagnosis and treatment, level set segmentation is utilized to segment the oral cavity and teeth from other structures in the image. This involves image acquisition, preprocessing, initialization, evolution, and postprocessing to extract a final contour for diagnosis and treatment planning. The resulting segmented image can be analyzed to detect abnormalities and plan orthodontic treatments or oral surgeries. Based on the initial layer segmentation, the CV-LBF tooth segmentation model in the direction of the crown and root respectively for fine segmentation, the target tooth segmentation image is obtained.
2.4CBCT image evaluation index
The performance of CBCT images was evaluated with segmentation accuracy (SA), maximum symmetrical surface distance (MSSD), average symmetrical surface distance (ASSD), over segmentation rate (OR), and under segmentation rate (UR). Maximum Symmetrical Surface Distance (MSSD) and Average Symmetric Surface Distance (ASSD) are two metrics that assess the precision of image registration algorithms by measuring the distance between two surfaces in a symmetric manner. They share the feature of being used in medical imaging to align images of the same patient taken at different times or align images from different patients to a common coordinate system. However, the main contrast between them is that while MSSD computes the maximum distance between the two surfaces, ASSD measures the average distance. The segmentation result of optimized CV-LBF algorithm was compared with those of adaptive threshold [22], region growing [23], DRLSE [24] and CV algorithms [25]. Adaptive thresholding is an image processing technique that adjusts the threshold for each pixel or region based on local image properties, useful for enhancing visibility and segmenting regions of interest in CBCT images. Region growing is a segmentation algorithm that groups neighboring pixels or voxels based on similarity, allowing for the extraction of distinct regions in CBCT images. Distance Regularized Level Set Evolution (DRLSE) is a level set-based segmentation algorithm that accurately captures complex shapes and boundaries of anatomical structures in CBCT images and finally computer vision algorithms encompass various techniques used for tasks such as image registration, feature extraction, object detection, and classification in CBCT image evaluation, enabling tasks like image alignment, quantitative analysis, and automated quality control.
(11)
(12)
(13)
2.5Intervention modalities in children with CDF
According to the voluntary principle, the family members of cldren with CDF chose the intervention method, of which 38 children were in the general anesthesia group (GAG) and the remaining 44 children chose the protective fixation intervention method and they were in controls. Before treatment, the two groups of children through the cartoons, toys, doctors dress, and other means to establish a warm and relaxed treatment environment, preoperative nurses through chatting with children and other means to promote a sense of trust, making the children’s mood relaxed.
The child in controls was fasted and water deprived for more than 4 hours before surgery, and the family signed the informed consent form for protective fixation therapy. The nurse assisted the child to lie supine on the oral treatment chair and adjust it to the appropriate height, and the restraint plate was placed flat on the oral treatment chair to fix the top of the restraint plate and the headrest. The child was wrapped with a restraint plate towel to expose only the child’s head and neck. During oral treatment, the family assisted with head immobilization and mouthpiece was used to assist the child’s mouth opening.
Children in GAG were fasted and water deprived for 8 hours before anesthesia. All children underwent GA using intravenous inhalation combined anesthesia technique. Combining inhalation anesthetics is common in anesthesia practice because it allows for a more precise and reliable level of anesthesia while reducing the risk of side effects associated with higher concentrations of a single agent. This approach also enables synergistic effects and reduced side effects, as well as flexibility in tailoring the anesthetic to the individual patient and procedure. After entering the operating room, the child underwent sedation, arteriovenous puncture, GA, and other operations. The assistant recorded the intraoperative conditions in detail. At the end of the operation, the patient was transferred to the GA recovery room and could leave the hospital after the vital signs were stable for 2 hours.
2.6Outcome measures
CFSS-DS and Venham [26] scores were counted before intervention in both groups, and CFSS-DS scores were also recorded at 2 hours after intervention in controls, after recovery in GAG. CFSS-DS and Venham scores were performed in all children at return visit 1 week after surgery.
The CFSS-DS [27] was rated 1 to 5 points according to the degree of fear, 5 points for very fear, 4 for more fear, 3 for comparative fear, 2 for a little fear, and 1 for no fear, with a total of 17 items, and with a total score of more than 42 indicating a high level of fear and less than 42 indicating a low level of fear.
2.7Statistical methods
Data were statistically analyzed using SPSS 22.0. The included measurement data were in accordance with the normal distribution, the measurement data were presented as mean
3.Results
3.1CBCT image segmentation results for CV-LBF model teeth
The CV-LBF model segments root canals in CBCT images by extracting local binary features and training a machine learning algorithm to predict root canal boundaries. It is trained on annotated datasets and can be used to segment the root canals of individual or multiple teeth, as well as images taken at different angles. CV-LBF model was applied to segment the root canals of teeth at different positions in CBCT images, and the results are illustrated in Fig. 2. CV-LBF model can accurately segment the root canals of teeth with different morphologies.
Figure 2.
Automatic segmentation diagram of root canal of CV-LBF model.
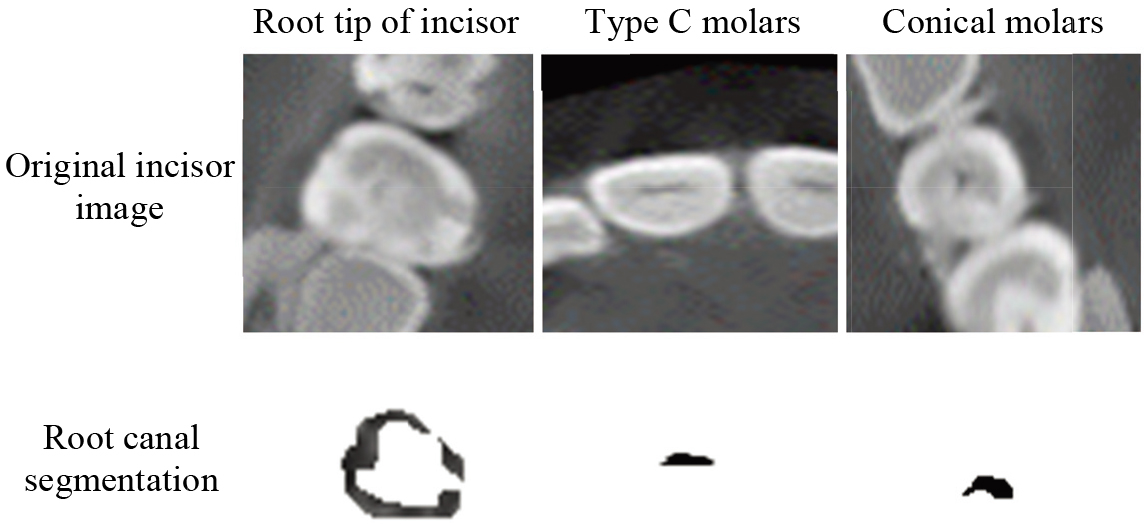
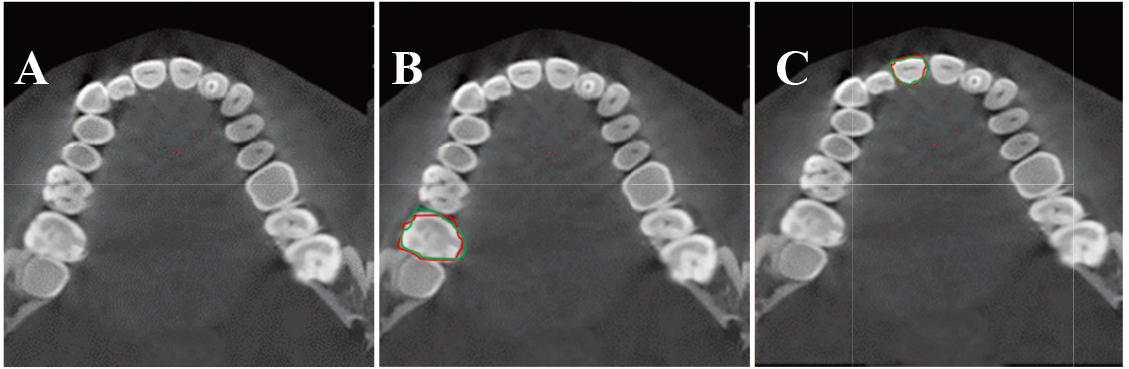
The CV-LBF model (red) was compared with the manual segmentation (green) (Fig. 3), and the tooth segmentation contours of the CV-LBF model were highly coincident with the manual segmentation results.
Figure 3.
CBCT cross-sectional tooth segmentation results. A: original CBCT image; B: molar segmentation result; C: incisor segmentation result.
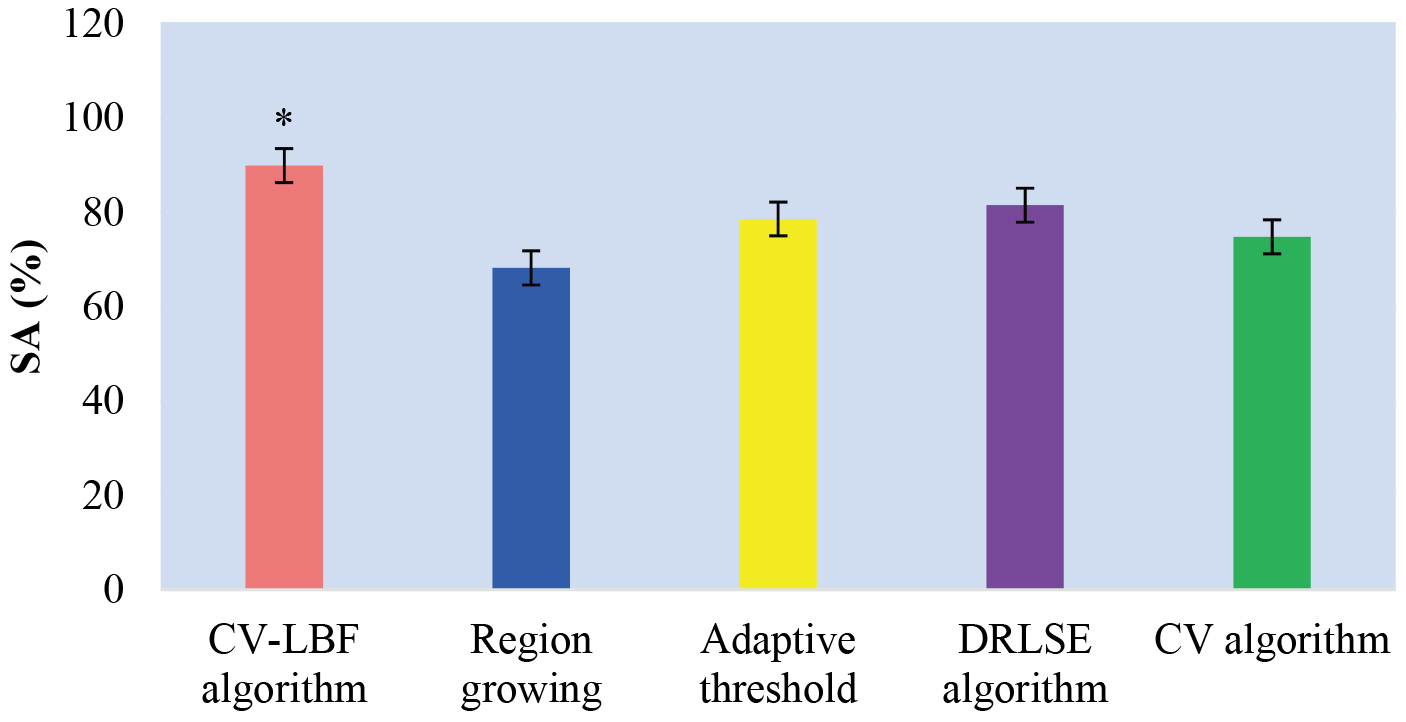
3.2Comparison of tooth segmentation accuracy of intelligent algorithm
The performance of various image segmentation algorithms on CBCT images, measured using the
Figure 4.
Comparison of
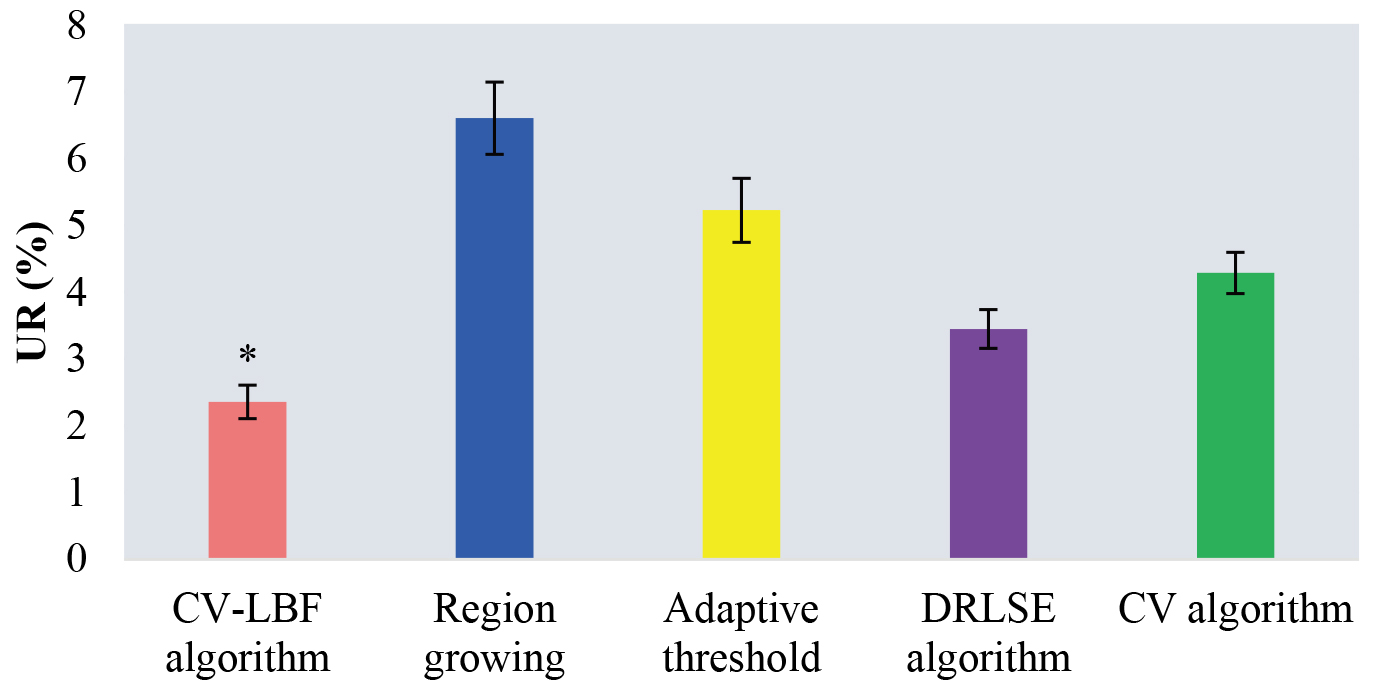
The OR value is a common metric used to evaluate the similarity between the segmented object and the ground truth object. It represents the ratio of the intersection between the segmented object and the ground truth object to the union of the two objects. A higher OR value indicates a better segmentation accuracy. The results find that the OR values of tooth CBCT images segmented by the CV-LBF (1.53
Figure 5.
Comparison of OR values of CBCT images of teeth segmented by different algorithms.
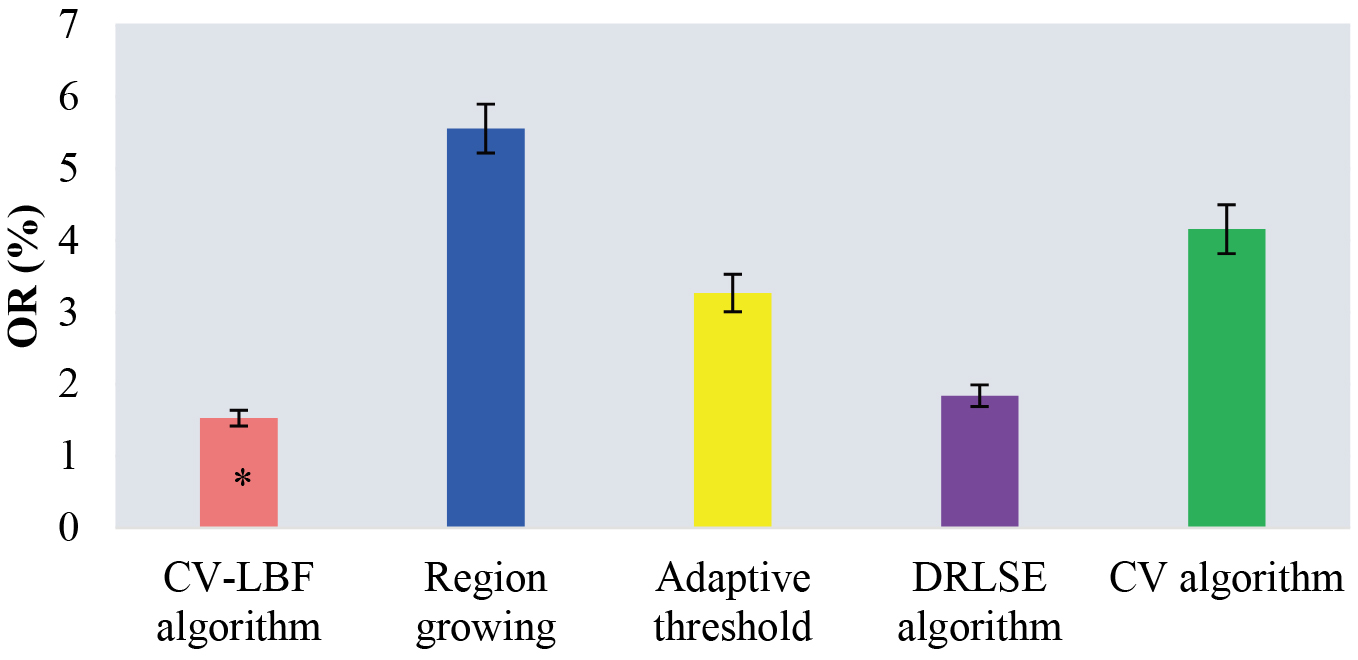
Figure 6.
Comparison of
3.3Comparison of MSSD and ASSD values of CBCT image segmentation with intelligent algorithm
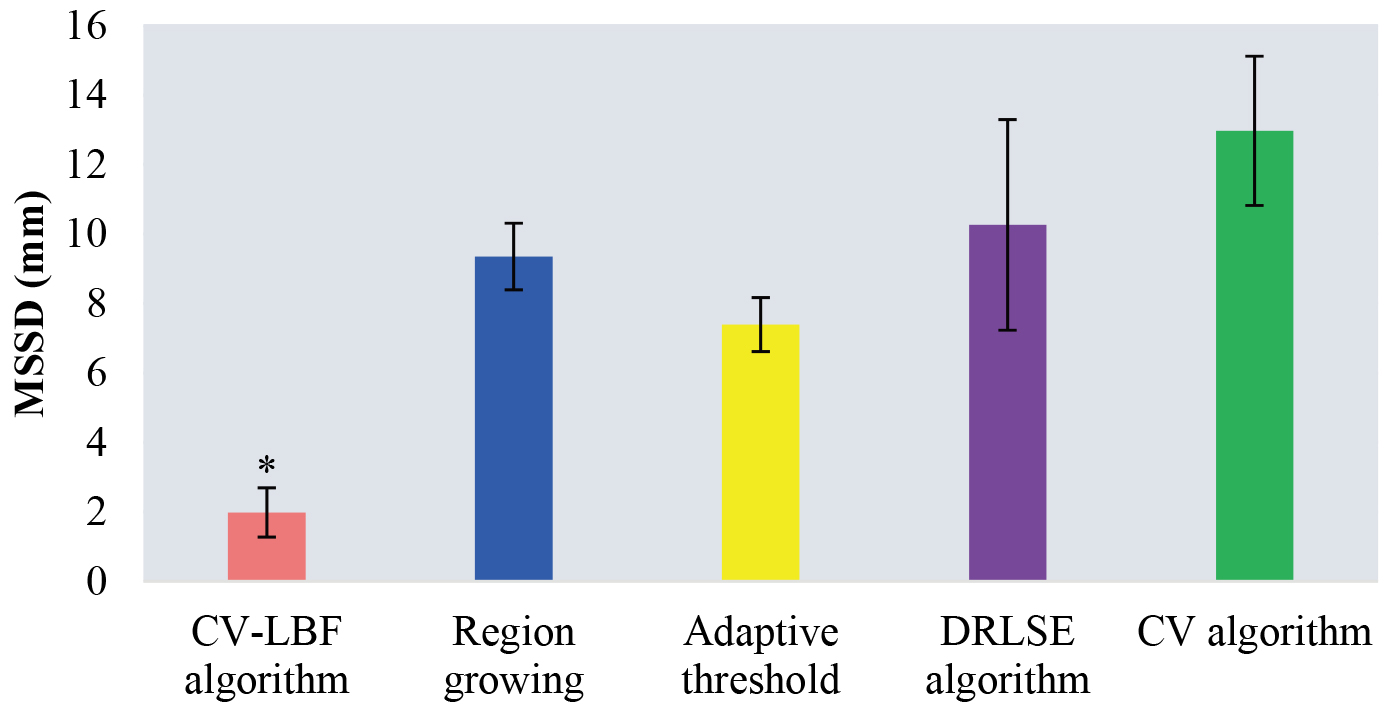
The evaluation metric used to compare the algorithms was the Mean Symmetric Surface Distance (MSSD), which measures the average distance between corresponding points on the surfaces of the segmented image and the ground truth image. The CV-LBF, region growing, adaptive threshold, DRLSE, and CV algorithms were compared, in which the MSSD values obtained for each algorithm were (1.98
ASSD is a widely used metric that measures the distance between the surfaces of two segmented objects. The CV-LBF, regional growth, adaptive threshold, DRLSE, and CV are the five different algorithms tested in the experiment. The average ASSD values obtained for each algorithm were (0.27
3.4Comparison of clinical characteristics of children with CDF before intervention
Statistical analysis was performed on the age, gender, parenting style, whether the child was the only child, and mode of delivery of GAG and controls (Table 1). The results indicated that there were no statistically significant differences in the age, gender, parenting style, whether the child was the only child, and mode of delivery between two groups (
Table 1
Basic data of patients
| Factor | GAG ( | Controls ( |
|
|
|---|---|---|---|---|
| Gender [case (%)] | 0.796 | 0.315 | ||
| Male | 18 (47.37%) | 21 (47.73%) | ||
| Female | 20 (52.63%) | 23 (52.27%) | ||
| Age (years) | 4.53 | 4.39 | 0.223 | 0.734 |
| Parenting style | 0.583 | 0.401 | ||
| Parenting rearing | 30 (78.95%) | 33 (75.00%) | ||
| Grandparental rearing | 8 (21.05%) | 11 (25.00%) | ||
| Only child | 1.753 | 0.226 | ||
| Yes | 23 (60.53%) | 28 (63.64%) | ||
| No | 15 (39.47%) | 16 (36.36%) | ||
| Mode of delivery | 0.441 | 0.503 | ||
| Spontaneous delivery | 26 (68.42%) | 29 (65.91%) | ||
| Caesarean section | 12 (31.58%) | 15 (34.09%) |
Figure 7.
Comparison of MSSD values of segmenting CBCT images by different algorithms. *Indicates statistical difference compared with CV algorithm,
3.5Comparison of education level of mothers and family income
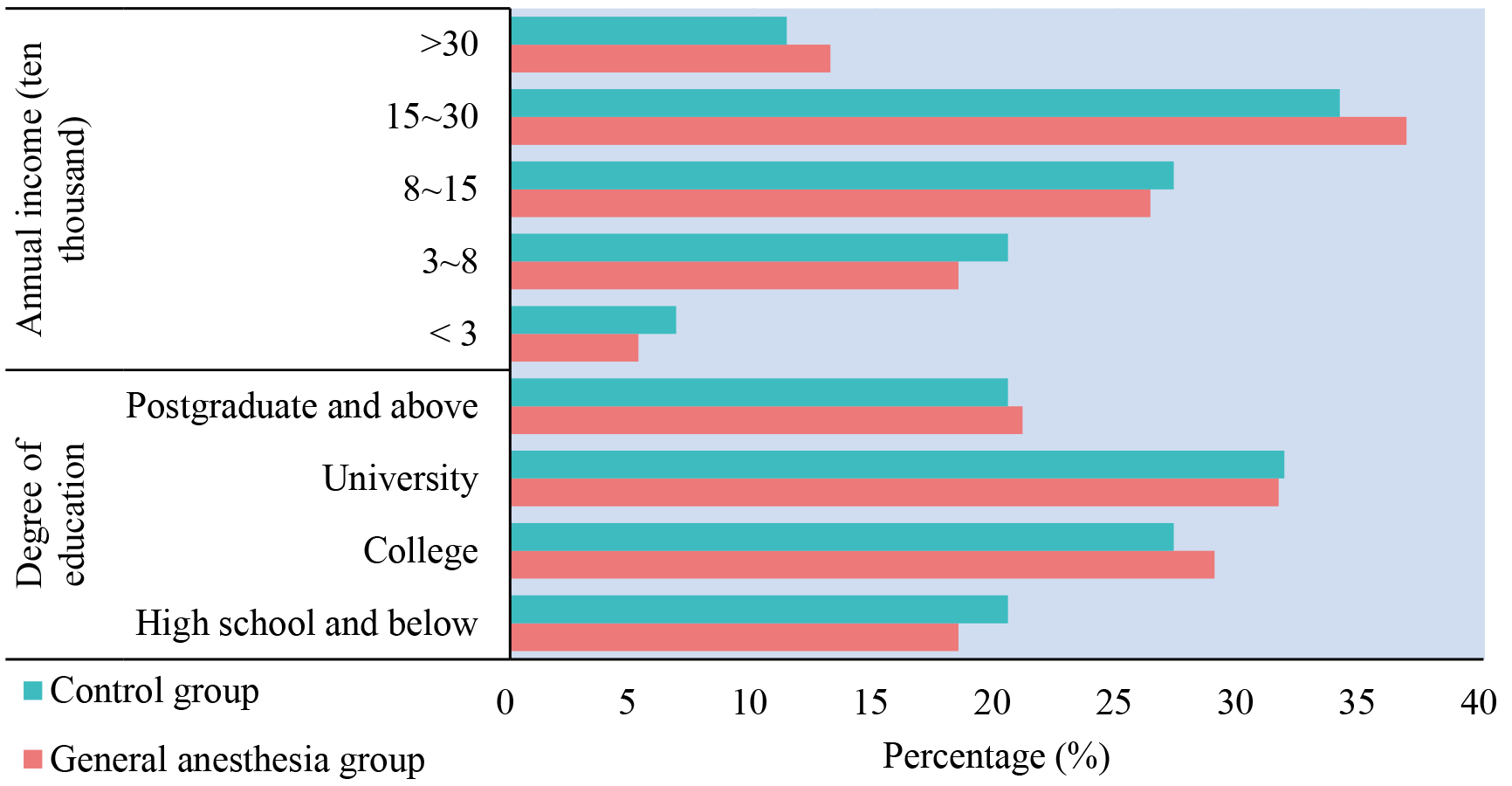
There were not clear different in maternal education level and family income between the two groups (
Figure 8.
Comparison of family income and maternal education level.
3.6Comparison of distribution of temperament types in children
Figure 9 shows the proportion of different temperament types in the two groups, 9 (23.68%), 10 (26.32%), 11 (28.95%), and 8 (21.05%) children with phlegmatic temperament, biliary temperament, sanguine temperament, and depressive temperament in GAG; 10 (22.73%), 12 (27.27%), 12 (27.27%), and 10 (22.73%) children in controls, respectively (
Figure 9.
Comparison of temperament type distribution.
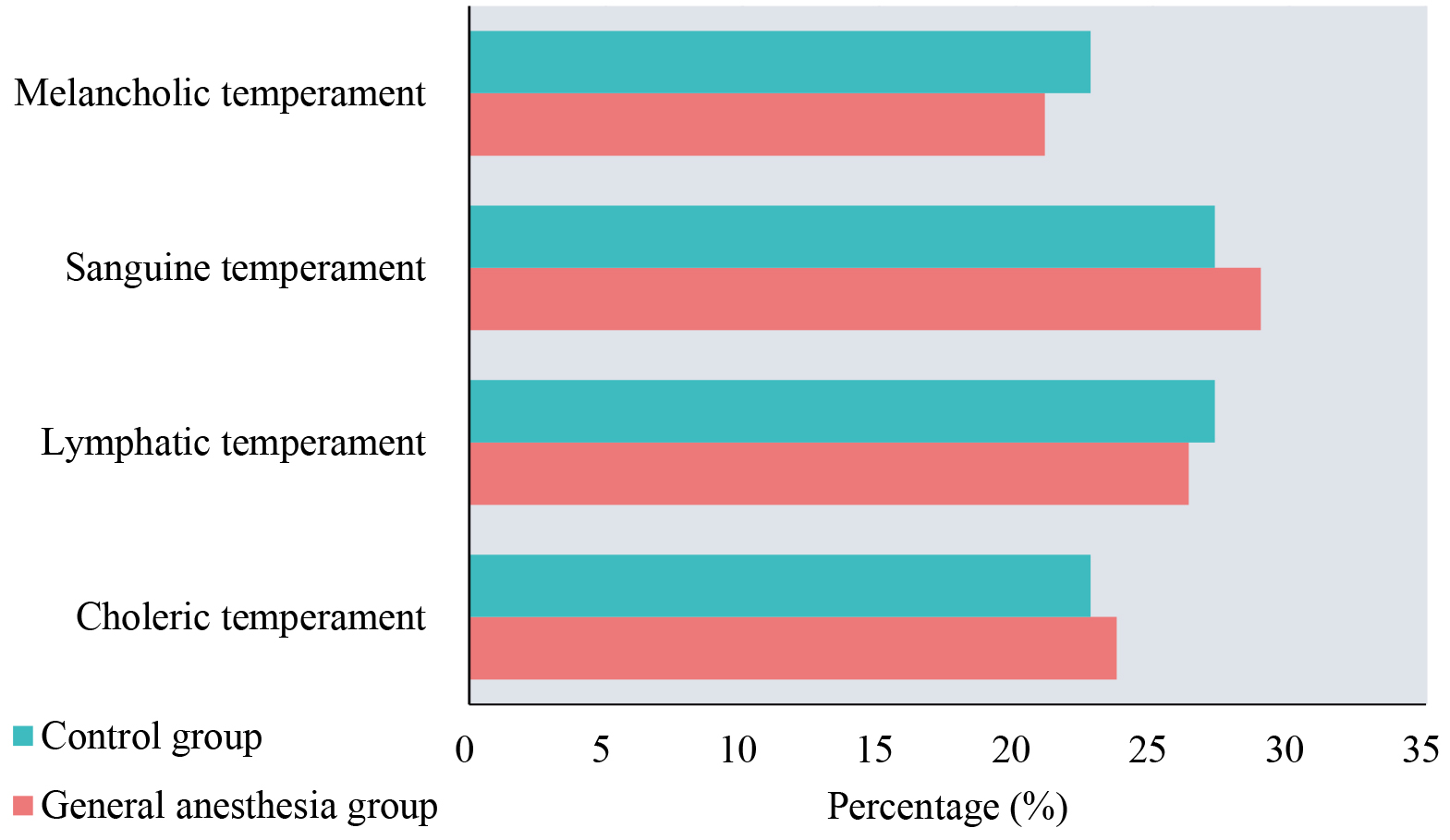
Figure 10.
Comparison of CFSS-DS values at different time periods before and after intervention. **Means compared with before intervention,
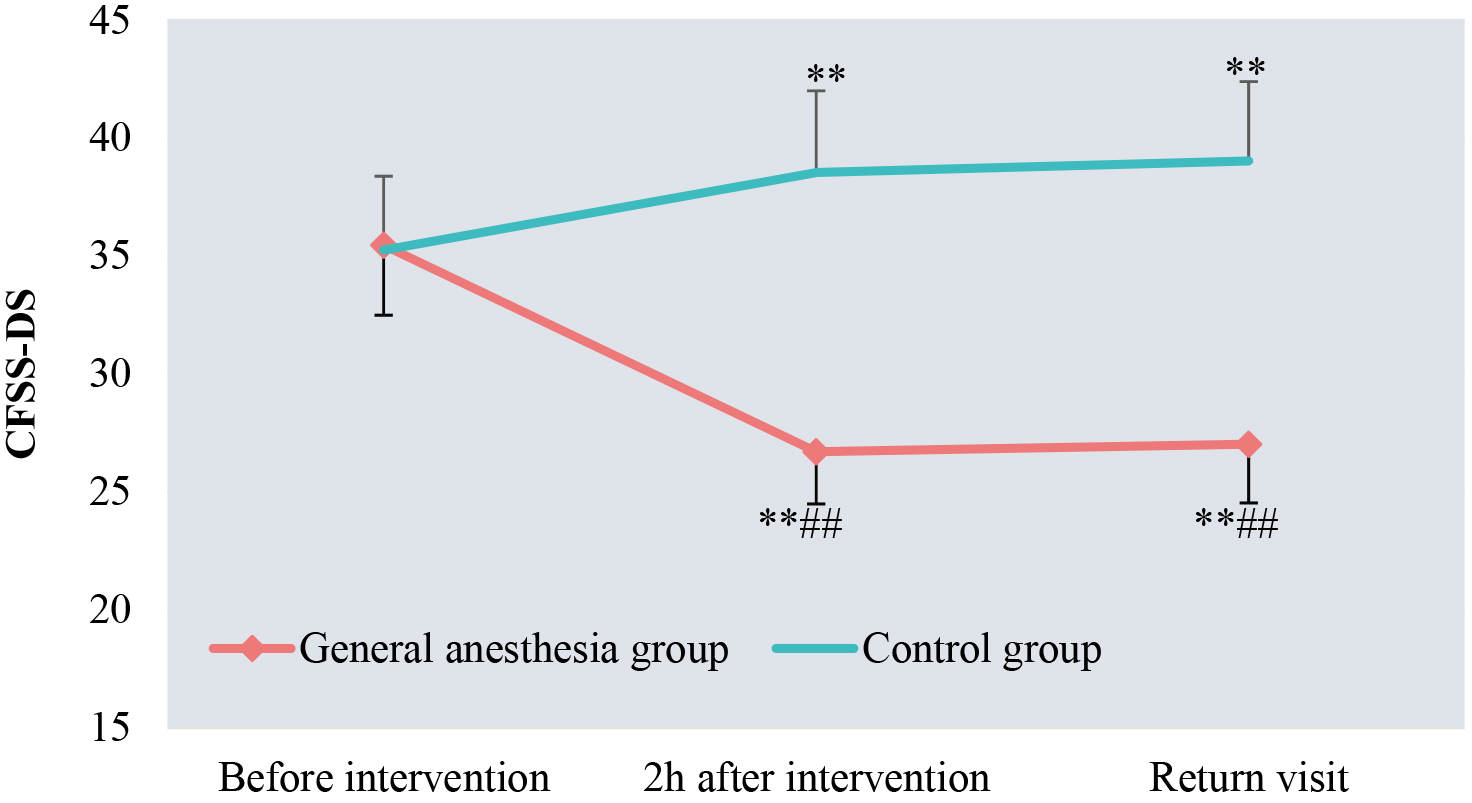
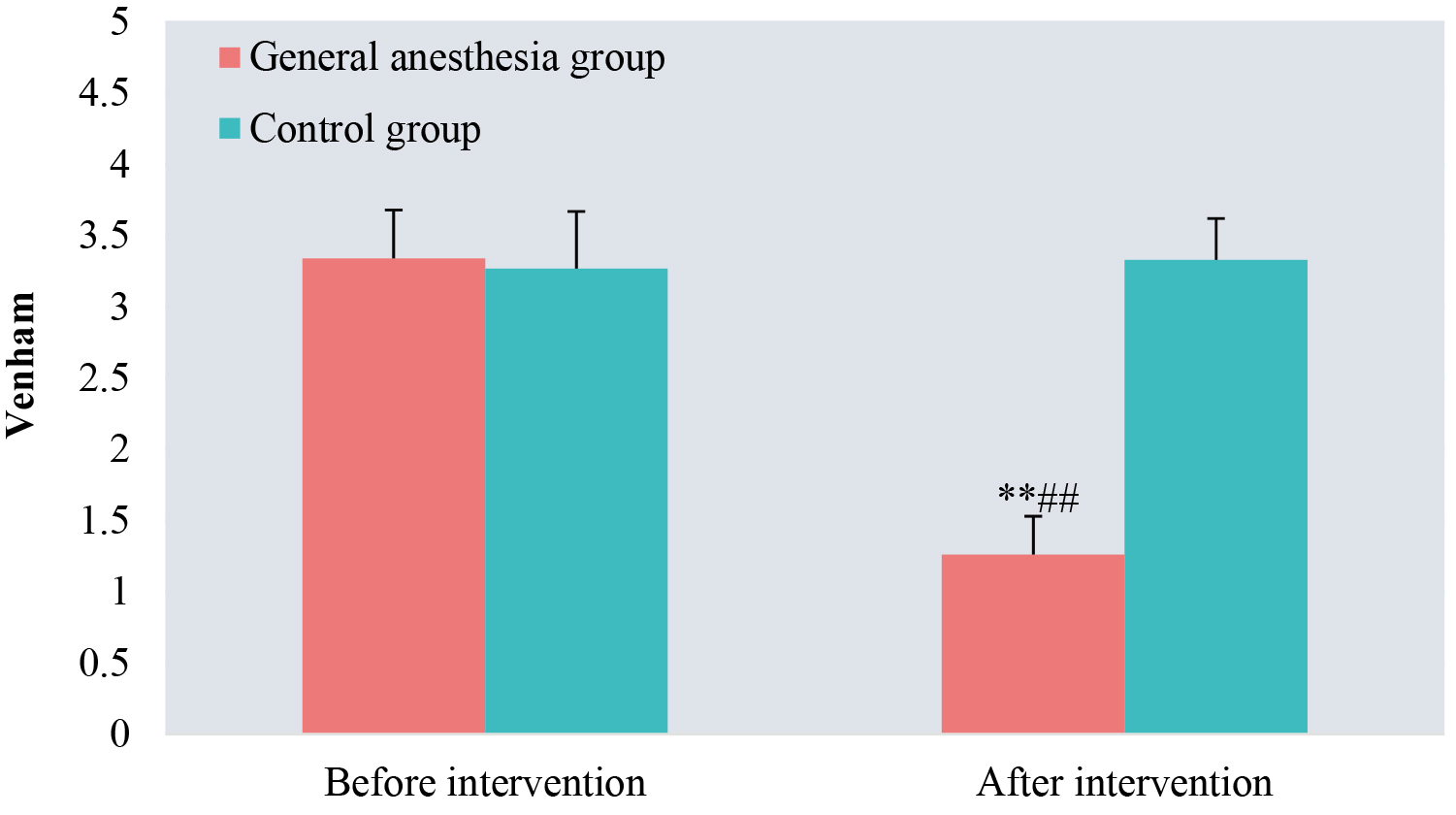
Figure 11.
Comparison of Venham scores before and after intervention.
3.7Comparison of CFSS-DS values at different time periods before and after intervention
Before intervention, the CFSS-DS scores of GAG and controls were (35.47
3.8Comparison of Venham scores before and after intervention
There was not obviously different in Venham scores between the two groups before intervention (
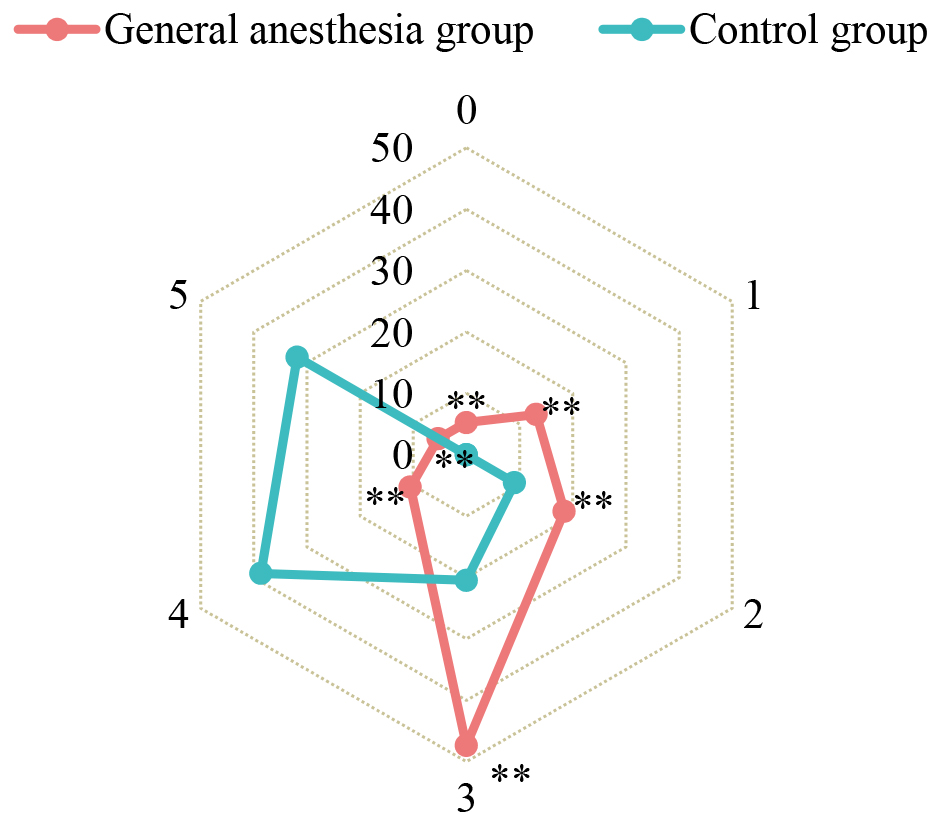
Before the intervention, GAG had 14 (36.84%), 13 (34.21%), and 11 (28.95%) children with Venham grade 3, 4, and 5, 16 (36.36%), and controls had 16 (36.36%), 17 (38.64%), and 11 (25.00%) children (
Figure 12.
Comparison of Venham grade distribution after intervention. **Means
4.Discussion
It was found that relative to regional growth algorithm, the value of CV-LBF algorithm was higher, the
C-type roots in molar root canals have irregular shapes, making them challenging to accurately segment during intelligent imaging. In China, approximately 32% of root canals are classified as C-type. The irregularities of these canals pose difficulties in identifying their boundaries and associated structures, leading to potential treatment complications. Dental professionals need to be well-prepared to address these challenges by utilizing advanced techniques and staying updated with the latest advancements in endodontics [30, 31]. The results suggested that the CV-LBF model could accurately segment the root canals of teeth with different morphologies, and the segmentation results were highly coincident with the manual delineation contours, showing that the CV-LBF model has potential application value in the segmentation of dental CBCT images.
The results of the current study revealed that parental education level, family economic income, and personality type of children with oral diseases will have a certain impact on CDF [32]. The above factors in GAG and controls were statistically analyzed. There was no statistical difference in maternal education level, family income, and personality type of children between the two groups (
5.Conclusion
A tooth CBCT image segmentation optimization algorithm CV-LBF was established to investigate its application value in the segmentation of tooth CBCT images in children. The effect of GA on anxiety relief in CDF was investigated in children with CDF. It is found that the intelligent model CV-LBF has high accuracy in segmenting tooth CBCT images and has potential application value, and GA intervention can effectively alleviate CDF anxiety. However, there are still some shortcomings, the compliance of children at return visit after intervention is not analyzed, and the effect of GA intervention on the compliance of children with CDF will be further analyzed in future work to provide more comprehensive data support for its application in pediatric stomatology. In conclusion, it provides some clinical basis for pediatric oral computer intelligent diagnosis and treatment and selection of CDF intervention program.
Funding
The authors did not receive any funding.
Data availability statement
No datasets were generated or analyzed during the current study.
Author contributions
All authors contributed to the design and methodology of the study, assessment of the outcomes and writing of the manuscript.
Conflict of interest
The authors do not have any conflicts of interest to report.
References
[1] | Xiao J, Fiscella KA, Gill SR. Oral microbiome: Possible harbinger for children’s health. Int J Oral Sci. (2020) ; 12: (1): 12. |
[2] | Kazeminia M, Abdi A, Shohaimi S, Jalali R, Vaisi-Raygani A, Salari N, Mohammadi M. Dental caries in primary and permanent teeth in children’s worldwide, 1995 to 2019: A systematic review and meta-analysis. Head Face Med. (2020) ; 16: (1): 22. |
[3] | Wang ZB, Ma Y, Liu H, et al. Simultaneous determination and pharmacokinetics of tetrandrine, fangchinoline, and cyclanoline in rat plasma by ultra-high performance liquid chromatography-mass spectrometry after oral administration of stephaniae tetrandrae radix extract. World Journal of Traditional Chinese Medicine, (2021) ; 7: (1): 130. |
[4] | Keels MA. Personalized dental caries management in children. Dent Clin North Am. (2019) ; 63: (4): 621-629. |
[5] | Alsadat FA, Alamoudi NM, El-Housseiny AA, Felemban OM, Dardeer FM, Saadah OI. Oral and dental manifestations of celiac disease in children: A case-control study. BMC Oral Health. (2021) ; 21: (1): 669. |
[6] | Wan ZB, Dong YQ, Yu ZC, Lv HB, Lv ZH. Semi-Supervised Support Vector Machine for Digital Twins Based Brain Image Fusion. (2021) ; 15: : 802. |
[7] | Zhou X, Li Y, Liang W. CNN-RNN based intelligent recommendation for online medical pre-diagnosis support. IEEE/ACM Transactions on Computational Biology and Bioinformatics, (2021) ; 18: (3): 912-921. |
[8] | Cakir Karabas H, Ozcan I, Erturk AF, Guray B, Unsal G, Senel SN. Cone-beam computed tomography evaluation of impacted and transmigrated mandibular canines: A retrospective study. Oral Radiol. (2021) Jul; 37: (3): 403-411. |
[9] | Mizuhashi F, Ogura I, Sugawara Y, Oohashi M, Mizuhashi R, Saegusa H. Diagnosis of root fractures using cone-beam computed tomography: Difference of vertical and horizontal root fracture. Oral Radiol. (2021) ; 37: (2): 305-310. |
[10] | Dias FMCS, Gradella CMF, Ferreira MC, Oliveira LB. Molar-incisor hypomineralization: Parent’s and children’s impact perceptions on the oral health-related quality of life. Eur Arch Paediatr Dent. (2021) Apr; 22: (2): 273-282. |
[11] | Alsadat FA, El-Housseiny AA, Alamoudi NM, Elderwi DA, Ainosa AM, Dardeer FM. Dental fear in primary school children and its relation to dental caries. Niger J Clin Pract. (2018) ; 21: (11): 1454-1460. |
[12] | Wu L, Gao X. Children’s dental fear and anxiety: Exploring family related factors. BMC Oral Health. (2018) ; 18: (1): 100. |
[13] | Panda S, Quadri MFA, Hadi IH, Jably RM, Hamzi AM, Jafer MA. Does dental fear in children predict untreated dental caries? An analytical cross-sectional study. Children (Basel). (2021) May 12; 8: (5): 382. |
[14] | Yon MJY, Chen KJ, Gao SS, Duangthip D, Lo ECM, Chu CH. An introduction to assessing dental fear and anxiety in children. Healthcare (Basel). (2020) ; 8: (2): 86. |
[15] | Guney SE, Araz C, Tirali RE, Cehreli SB. Dental anxiety and oral health-related quality of life in children following dental rehabilitation under general anesthesia or intravenous sedation: A prospective cross-sectional study. Niger J Clin Pract. (2018) Oct; 21: (10): 1304-1310. |
[16] | Galeotti A, Garret Bernardin A, D’Antò V, Ferrazzano GF, Gentile T, Viarani V, Cassabgi G, Cantile T. Inhalation conscious sedation with nitrous oxide and oxygen as alternative to general anesthesia in precooperative, fearful, and disabled pediatric dental patients: A large survey on 688 working sessions. Biomed Res Int. (2016) ; 2016: : 7289310. |
[17] | Xie X, Pan X, Zhang W, An J. A context hierarchical integrated network for medical image segmentation. Computers and Electrical Engineering. (2022) ; 101: : 108029. |
[18] | Xie X, Zhang W, Pan X, Xie L, Shao F, Zhao W, An J. CANet: Context aware network with dual-stream pyramid for medical image segmentation. Biomedical Signal Processing and Control. (2023) ; 81: : 104437. |
[19] | Xu L, Zhang XD, Zeng C, Yang HF. Analysis of missed diagnosis of gastric lipomas by CT. Curr Med Imaging. (2021) ; 17: (7): 911-915. |
[20] | Satpute N, Gómez-Luna J, Olivares J. Accelerating Chan-Vese model with cross-modality guided contrast enhancement for liver segmentation. Comput Biol Med. (2020) ; 124: : 103930. |
[21] | Haghnegahdar AA, Kolahi S, Khojastepour L, Tajeripour F. Diagnosis of tempromandibular disorders using local binary patterns. J Biomed Phys Eng. (2018) ; 8: (1): 87-96. |
[22] | Sun H, Yang J, Fan R, Xie K, Wang C, Ni X. Stepwise local stitching ultrasound image algorithms based on adaptive iterative threshold Harris corner features. Medicine (Baltimore). (2020) ; 99: (37): e22189. |
[23] | Jiang Y, Qian J, Lu S, Tao Y, Lin J, Lin H. LRVRG: A local region-based variational region growing algorithm for fast mandible segmentation from CBCT images. Oral Radiol. (2021) ; 37: (4): 631-640. |
[24] | Zheng J, Zhang D, Huang K, Sun Y. A CBCT series slice image segmentation method. J Xray Sci Technol. (2018) ; 26: (5): 815-832. |
[25] | Nag MK, Chatterjee S, Sadhu AK, Chatterjee J, Ghosh N. Computer-assisted delineation of hematoma from CT volume using autoencoder and Chan Vese model. Int J Comput Assist Radiol Surg. (2019) ; 14: (2): 259-269. |
[26] | Rath S, Das D, Sahoo SK, Raj A, Guddala NR, Rathee G. Childhood dental fear in children aged 7–11 years old by using the Children’s Fear Survey Schedule-Dental Subscale. J Med Life. (2021) Jan-Mar; 14: (1): 45-49. |
[27] | Dahlander A, Soares F, Grindefjord M, Dahllöf G. Factors associated with dental fear and anxiety in children aged 7 to 9 years. Dent J (Basel). (2019) ; 7: (3): 68. |
[28] | Zou Y, Yao G, Wang J. Research on 3D crack segmentation of CT images of oil rock core. PLoS One. (2021) Oct 14; 16: (10): e0258463. |
[29] | Zhang L, Zhao J, Yang H, Jiang Z, Li Q. Unsupervised scoliosis diagnosis via a joint recognition method with multifeature descriptors and centroids extraction. Comput Math Methods Med. (2018) ; 2018: : 6213264. |
[30] | Brea G, Gomez F, Gomez-Sosa JF. Cone-beam computed tomography evaluation of C-shaped root and canal morphology of mandibular premolars. BMC Oral Health. (2021) ; 21: (1): 236. |
[31] | Ren HY, Zhao YS, Yoo YJ, Zhang XW, Fang H, Wang F, Perinpanayagam H, Kum KY, Gu Y. Mandibular molar C-shaped root canals in 5th millennium BC China. Arch Oral Biol. (2020) Sep; 117: : 104773. |
[32] | Ghaderi F, Solhjou N. The effects of lavender aromatherapy on stress and pain perception in children during dental treatment: A randomized clinical trial. Complement Ther Clin Pract. (2020) ; 40: : 101182. |
[33] | López-Velasco A, Puche-Torres M, Carrera-Hueso FJ, Silvestre FJ. General anesthesia for oral and dental care in paediatric patients with special needs: A systematic review. J Clin Exp Dent. (2021) Mar 1; 13: (3): e303-e312. |
[34] | Kawai M, Kurata S, Sanuki T, Mishima G, Kiriishi K, Watanabe T, Ozaki-Honda Y, Yoshida M, Okayasu I, Ayuse T, Tanoue N, Ayuse T. The effect of midazolam administration for the prevention of emergence agitation in pediatric patients with extreme fear and non-cooperation undergoing dental treatment under sevoflurane anesthesia, a double-blind, randomized study. Drug Des Devel Ther. (2019) ; 13: : 1729-1737. |
[35] | Ohtawa Y, Yoshida M, Fukuda K. Parental satisfaction with ambulatory anesthesia during dental treatment for disabled individuals and their preference for same in future. Bull Tokyo Dent Coll. (2019) ; 60: (1): 53-60. |
[36] | Singh S, Neyaz N, Tanwar AS, Patil AN, Khan AM, Kakti A. Propofol’s efficacy and outcomes on anxious children’s behavior in the course of dental therapy: An interventional trial. J Pharm Bioallied Sci. (2022) ; 14: (Suppl 1): S550-S553. |
[37] | Ichikawa K, Fujiwara T, Kawachi I. Prenatal alcohol exposure and child psychosocial behavior: A sibling fixed-effects analysis. Front Psychiatry. (2018) ; 9: : 570. |



