More Information
Submitted: September 27, 2022 | Approved: October 06, 2022 | Published: October 07, 2022
How to cite this article: Singh G, Chauhan SS, Nagpal A, Sinha A, Sharma S, et al. A surgical procedure for re-implanting a tooth that has been rendered hopeless because of periodontitis: a case report. Arch Surg Clin Res. 2022; 6: 013-015.
DOI: 10.29328/journal.ascr.1001064
Copyright License: © Singh G, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Replantation; Periodontitis; RCT; TFO; Treatment outcome
A surgical procedure for re-implanting a tooth that has been rendered hopeless because of periodontitis: a case report
Gaurav Singh1*, Shailendra S Chauhan2, Ajay Nagpal3, Aditya Sinha4, Satendra Sharma5 and Saksham Kulshrestha1
1MDS, Dr. Bheemrao Ambedkar University, India
2Department of Periodontology, Dr. Bheemrao Ambedkar University, India
3Department of Endodontics, Dr. Bheemrao Ambedkar University, India
4Professor, Dr. Bheemrao Ambedkar University, India
5Reader, Dr. Bheemrao Ambedkar University, India
*Address for Correspondence: Gaurav Singh, MDS, Dr. Bheemrao Ambedkar University, India, Email: drgauravsingh118@gmail.com
Aim and methodology: This article describes a periodontally compromised, hopeless incisor tooth that was purposefully replanted, along with the results after six months. This entails the deliberate removal of the tooth and its subsequent correct manipulation and endodontic restoration before reinserting it into the socket.
Results: Hopeless lower incisors with periodontal involvement were transplanted utilizing an implant surgical drilling approach after receiving root canal therapy and tetracycline-HCI conditioning. Bone graft material was added and the procedure was monitored for six months. The tooth was observed to be asymptomatic, functioning normally, and showing no pathologic radiological changes. With minimal bleeding during probing and no growth of pathological pockets, the periodontal condition was within normal limits. Alveolar bone support was seen to be adequate. The results may suggest that, in some circumstances, purposeful replantation is a viable strategy of treatment for maintaining native dentition.
Conclusion: Intentional tooth reimplantation can be an alternative treatment option for periodontally involved teeth with poor or hopeless prognoses.
Periodontal therapy’s primary purpose is to repair the teeth. On a biological and functional level, managing anterior teeth with extensive periodontal damage is difficult. In individuals with severe periodontal disease, neither surgical nor non-surgical treatment options are effective, and extraction may be required [1]. When a tooth is taken from its socket and treated outside the mouth, it is replanted [2]. This sort of treatment may be employed when more traditional types of treatment fail or are unfeasible [3]. It has also been utilized to treat vertical fractures in addition to horizontal fractures, endodontic and periodontal diseases, periodontal impaired teeth with unknown results, and specific anatomical anomalies, such as radicular grooves [4].
Following purposeful replantation for periodontally affected teeth, Baykara and Eratalay observed a substantial decrease in pocket depth, bone development, and ankylosis after eight years of follow-up [5].
In this case report, the clinical and radiographic 3-month results of purposeful replantation of periodontal damaged teeth were attempted.
In this 28-year-old individual with a normal systemic state, radiographs and clinical results revealed localized Periodontitis. On the left and right central incisors, a combination of significant periodontal bone loss, deep periodontal pockets, over-expansion, pathological migration, suppuration, bleeding on probing, sensitivity on the lower central and lateral incisors, and general gum recession was detected. Attachment loss was moderate to severe, and oral hygiene was modest to moderate, according to a general oral examination. The radiographs indicated a substantial alveolar bone loss, as well as apical bone loss and a widening of the periodontal ligament gaps (Figure 1). The patient was scheduled for periodontal therapy. Oral hygiene education, scaling, and root planning was all part of the early stages of periodontal treatment. Within a week, the periodontal treatment resulted in considerable improvements in oral hygiene and gum health, as well as a reduction in periodontal pocket depth. The central and lateral incisors were endodontically treated and replanted in two visits. Despite the chance that the tooth may not survive, the patient agreed to reimplantation. The written consent was signed by the patient.
Figure 1: Preoperative radiograph.
Reimplantation procedure
After the administration of local anesthesia sulcular incision was given, and the gingival attachments of central and lateral incisors were removed using a peristome. Teeth were gently removed and placed on a moistened, sanitized sponge using an atraumatic approach. After the apex was gently dried, a little quantity of zinc-free amalgam was added to close the apical foramen. To remove the granulation tissue at the bottom of the socket, curette it and gently rinse it with sterile saline solution. The socket walls were prepared by drilling at a low speed and chilling with sterile saline (Figure 2). Scaling and planning were done on the root surfaces.
Figure 2: Reimplantation site prepared.
Tetracycline-HCL (100 mg/ml) was administered to root surfaces using sterile cotton pellets. The roots of the teeth were kept inside the socket using a dental bone graft and a PRF membrane, and the splinted tooth was replanted and sutured as illustrated in Figures 3,4. Platelet-Rich Fibrin (PRF) is an autologous platelet concentrate that consists of cytokines, platelets, leukocytes, and circulating stem cells. It has been considered to be effective in bone regeneration and is mainly used for oral and maxillofacial bone. Although currently the use of PRF is thought to support alveolar ridge preservation, there is a lack of evidence regarding the application of PRF in osteogenesis. In this paper, we will provide examples of PRF application, and we will also summarize different measures to improve the properties of PRF for achieving better osteogenesis. The effect of PRF as a bone graft material on osteogenesis based on laboratory investigations, animal tests, and clinical evaluations is first reviewed here. In vitro, PRF was able to stimulate cell proliferation, differentiation, migration, mineralization, and osteogenesis-related gene expression. Preclinical and clinical trials suggested that PRF alone may have a limited effect. To enlighten researchers, modified PRF graft materials are further reviewed, including PRF combined with other bone graft materials, PRF combined with drugs, and a new-type PRF [5].
Figure 3: Mixing of PRF with bone graft demineralized bone matrix xenograft-Type I collagen granules.
Figure 4: Splinting after reinsertion of the tooth in the socket.
Postoperative care
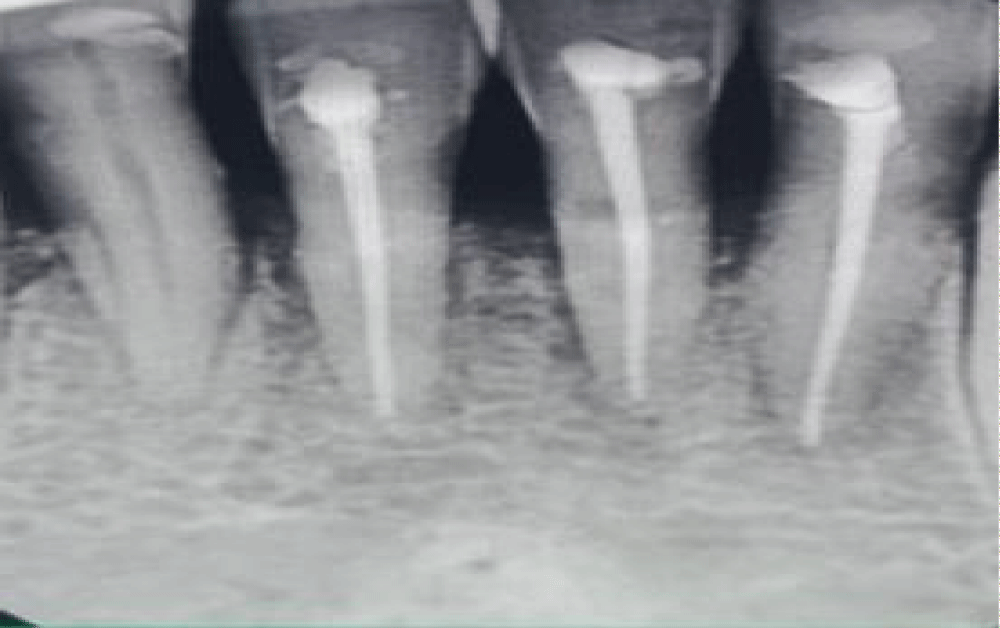
Patients were advised to avoid eating stiff foods with their anterior teeth for at least three months. A dose of amoxicillin 500 mg is prescribed twice a day. In addition to routine oral hygiene, prescribe analgesics and interdental brushing on the replanted area for five days. A 0.2% chlorhexidine mouthwash was prescribed twice daily for 14 days. Regeneration followed three months later. A maintenance recall program was placed on the patient for the first three months following regeneration therapy. Figure 5 shows an indicated positive result three months after insertion. At each recall visit, we reviewed clinical parameters such as splint integrity and provided oral prophylaxis and instructions on oral hygiene. Observations and radiographs indicate the patient has continued receiving supportive periodontal therapy for 6 months and has not displayed any untoward signs of root resorption or mobility. Although the supportive periodontal therapy will go on and will observe the changes in the future.
Figure 5: 6 Months follow-up radiographic picture.
As this procedure is having an advantage over other procedures like extraction and implants are:
- we can preserve the natural tooth
- There is no need for a costly procedure like an implant
- To overcome the complications associated with implant placement
- This procedure consumes less time.
Numerous studies have shown positive outcomes but this procedure has a limitation of the will go under ankylosis in the future and the procedure is very fine. It has been reported that periodontally involved teeth can be replanted successfully over 8 years by Baykara and Eratalay [6]. In 2003, Demiralp et al. reported positive results after replanting periodontal hopeless teeth [7]. In 2010, Yaprak, et al. reported successful reimplantation of two upper adjacent central teeth that had become extremely mobile due to extensive periodontal disease [8]. A similar treatment plan was followed in the current cases, which was successful for three months. An alternative is to remove the central incisor and replace it with opposing laterals and central teeth using a fixed prosthetic restoration. However, the treatment would be relatively inexpensive for patients and would yield some results. In the first six months following the extraction, 40% of the alveolar height and 60% of the alveolar width may be lost. Because of this, politics in the central area would be taller than usual, and dark spots in embrasure areas would be larger than usual. Alveolar crest replanting prevented post-extraction loss [9]. According to some reports [10], there should be a 15-minute period between extraction and replanting. The replanting process took about 30 minutes in these case reports. Periodontal disease is treated by removing irritants from tooth surfaces and root surfaces. There is an accumulation of plaque and dental calculus, resulting in periodontal destruction, pocket formation, and bone loss [11]. The mainstay of treatment is extraction, since it may lead to mobility. According to Demiralp, et al. [1], proper patient selection based on clinical and radiographic evaluations directly affects the success of intentional replantation.
When periodontally compromised teeth need to be extracted, intentional replantation is viewed as a last resort treatment option although other options cannot be neglected. Periodontal-involved cases can be treated with intentional replantation, which has the benefits of performing debridement of root surfaces extra orally and carefully without the need for extensive tissue removal. It can also provide access to conditioning or treating root surfaces for better regeneration outcomes. This case report describes the short-term successful replantation of a periodontal involved upper central tooth. After the intentional replantation procedure, the patients were happy and functional. Patient condition is monitored long-term.
- Demiralp B, Nohutçu RM, Tepe DI, Eratalay K. Intentional replantation for periodontally involved hopeless teeth. Dent Traumatol. 2003 Feb;19(1):45-51. doi: 10.1034/j.1600-9657.2003.00084.x. PMID: 12656855.
- Dryden JA, Arens DE. Intentional replantation. A viable alternative for selected cases. Dent Clin North Am. 1994 Apr;38(2):325-53. Erratum in: Dent Clin North Am 1994 Oct;28(4):viii. PMID: 8206180.
- Messkoub M. Intentional replantation: a successful alternative for hopeless teeth. Oral Surg Oral Med Oral Pathol. 1991 Jun;71(6):743-7. doi: 10.1016/0030-4220(91)90286-l. PMID: 2062526.
- Al-Hezaimi K, Naghshbandi J, Simon JH, Oglesby S, Rotstein I. Successful treatment of a radicular groove by intentional replantation and Emdogain therapy. Dent Traumatol. 2004 Aug;20(4):226-8. doi: 10.1111/j.1600-9657.2004.00236.x. PMID: 15245522.
- Liu Y, Sun X, Yu J, Wang J, Zhai P, Chen S, Liu M, Zhou Y. Platelet-Rich Fibrin as a Bone Graft Material in Oral and Maxillofacial Bone Regeneration: Classification and Summary for Better Application. Biomed Res Int. 2019 Dec 6;2019:3295756. doi: 10.1155/2019/3295756. PMID: 31886202; PMCID: PMC6925910.
- Baykara M, Eratalay K. Replantation in cases with advanced periodontal destruction. J Hacettepe Fac Dent. 1995; 19:124‑8.
- Demiralp B, Nohutçu RM, Tepe DI, Eratalay K. Intentional replantation for periodontally involved hopeless teeth. Dent Traumatol. 2003 Feb;19(1):45-51. doi: 10.1034/j.1600-9657.2003.00084.x. PMID: 12656855.
- Yaprak E, Hakki SS, Akman S, Belli S. Aesthetical and functional management of periodontal involved hopeless anterior teeth with multidisciplinary approach: 4 years follow up. Dis Hekimligi Fakültesi dergisi The Journal of the Dental Faculty of Ankara University. 2010; 19:176‑81.
- Lekovic V, Camargo PM, Klokkevold PR, Weinlaender M, Kenney EB, Dimitrijevic B, Nedic M. Preservation of alveolar bone in extraction sockets using bioabsorbable membranes. J Periodontol. 1998 Sep;69(9):1044-9. doi: 10.1902/jop.1998.69.9.1044. PMID: 9776033.
- Dryden JA, Arens DE. Intentional replantation. A viable alternative for selected cases. Dent Clin North Am. 1994 Apr;38(2):325-53. Erratum in: Dent Clin North Am 1994 Oct;28(4):viii. PMID: 8206180.
- Demiralp B, Tözüm TF, Eratalay K. Intentional replantation of a periodontal involved hopeless molar tooth: Results of 3‑year follow-up: A case report. Dergisi cilt Hacettepe Dental Schools. 2005; 29:47‑51.