- Department of Neurological Surgery, University of Miami, Miami, Florida, United States,
- Department of Neurosurgery, King Fahad Medical City, Riyadh, Saudi Arabia,
- College of Medicine, Alfaisal University, Riyadh, Saudi Arabia.
Correspondence Address:
Turki Elarjani
Department of Neurosurgery, King Fahad Medical City, Riyadh, Saudi Arabia,
DOI:10.25259/SNI_521_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Turki Elarjani1, Othman T. Almutairi2, Modhi Alhussinan3, Gmaan Alzhrani2, Fahad E. Alotaibi2, Mohammed Bafaquh2. Bibliometric analysis of the top 100 most-cited articles on astrocytoma. 17-Feb-2021;12:62
How to cite this URL: Turki Elarjani1, Othman T. Almutairi2, Modhi Alhussinan3, Gmaan Alzhrani2, Fahad E. Alotaibi2, Mohammed Bafaquh2. Bibliometric analysis of the top 100 most-cited articles on astrocytoma. 17-Feb-2021;12:62. Available from: https://surgicalneurologyint.com/surgicalint-articles/10591/
Abstract
Background: Citation analysis reflects the scientific recognition and influential performance of a published article within its field. We aim to identify the top 100 most-cited articles on astrocytoma using this bibliometric analysis method.
Methods: In May 2020, we performed a thorough search in the Scopus database using the word “Astrocytoma.” The top 100 most-cited articles were arranged based on citation count in descending order. The resultant articles were then analyzed with an assessment of pertinent factors.
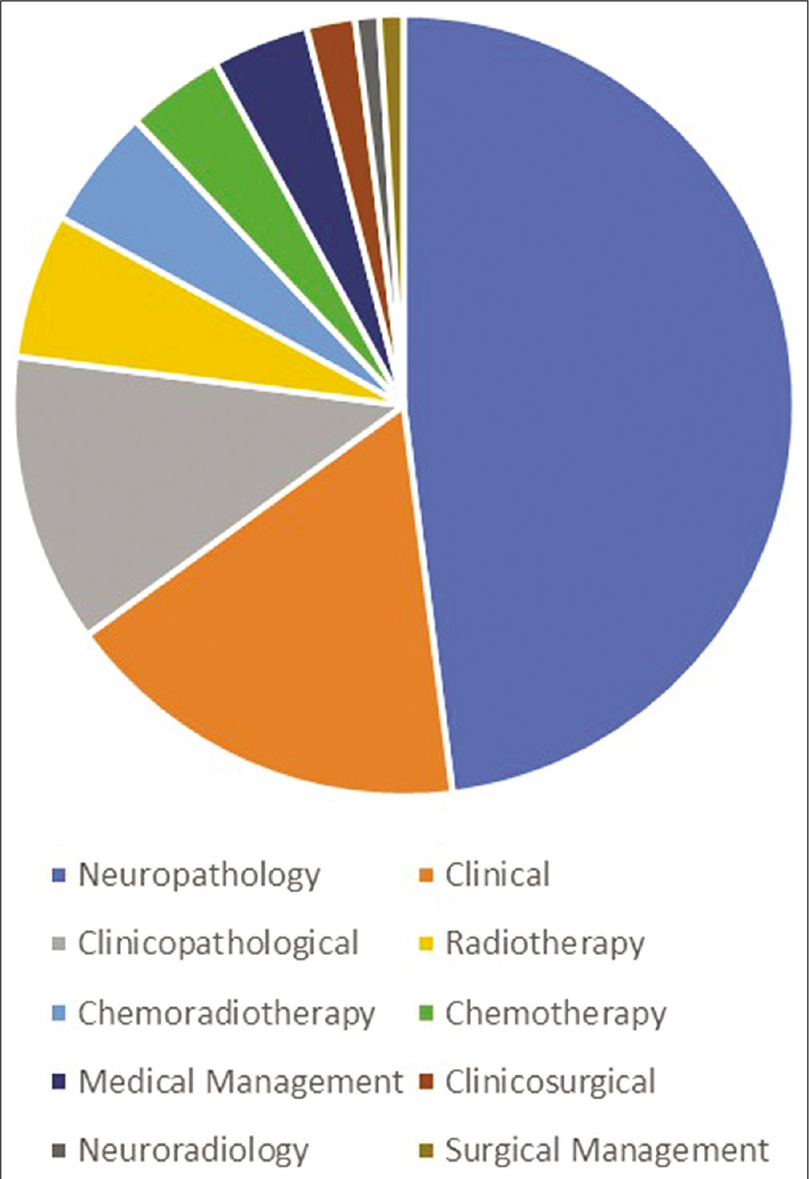
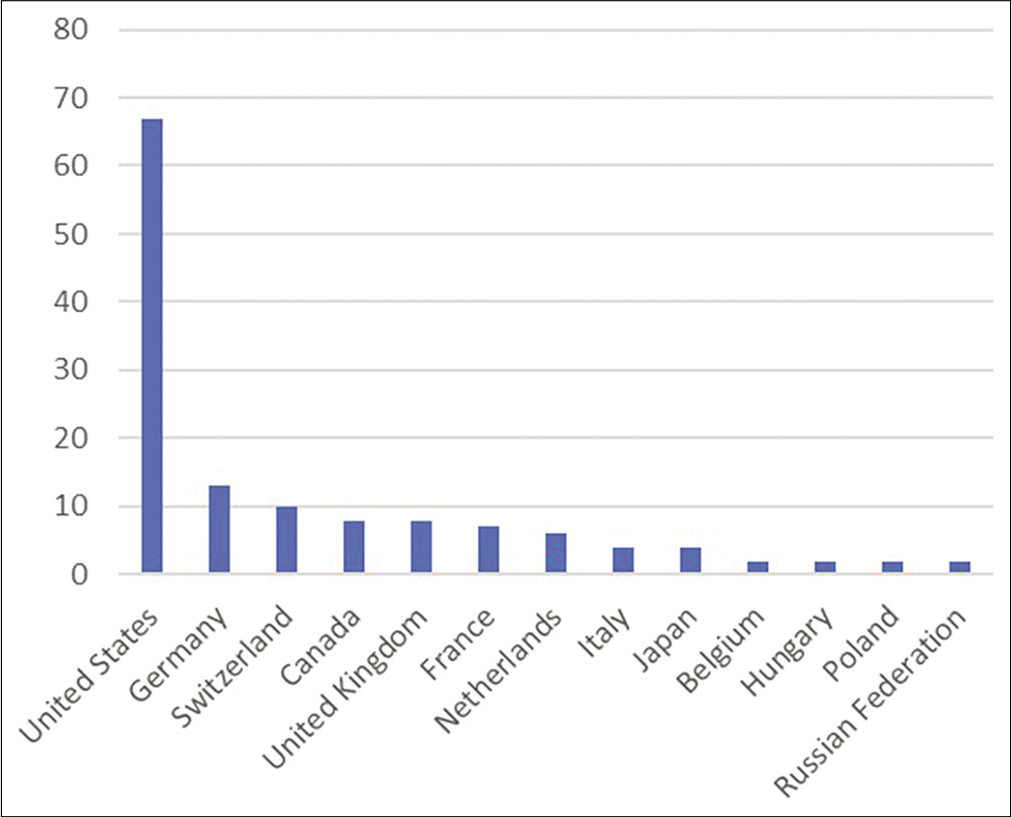
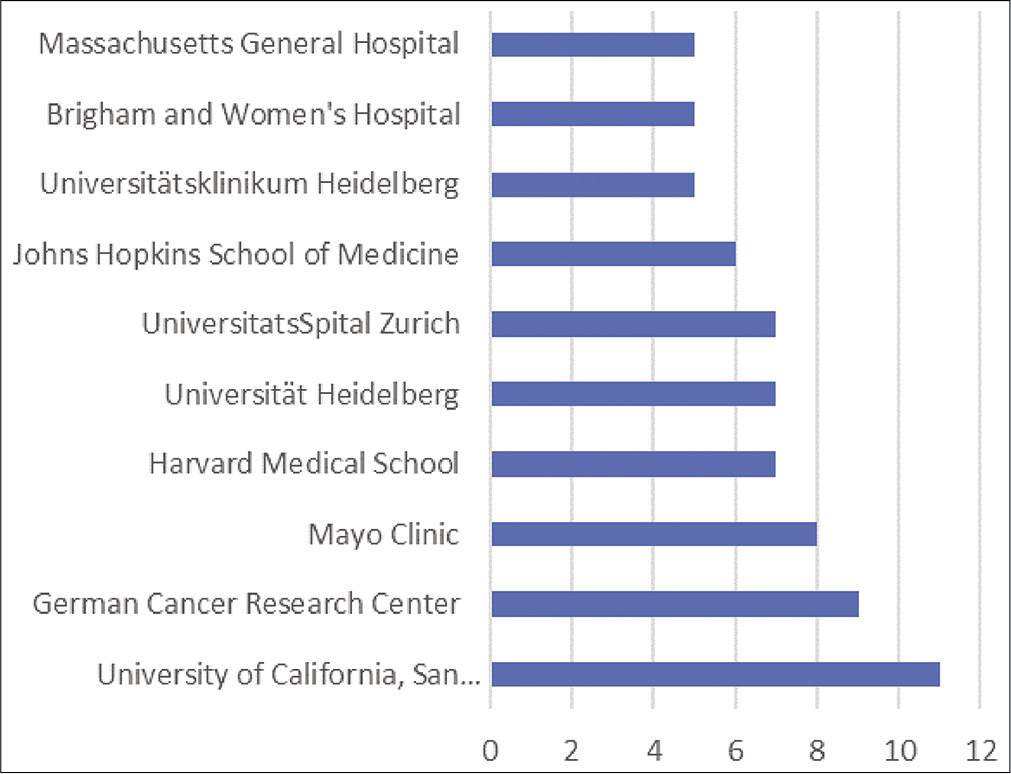
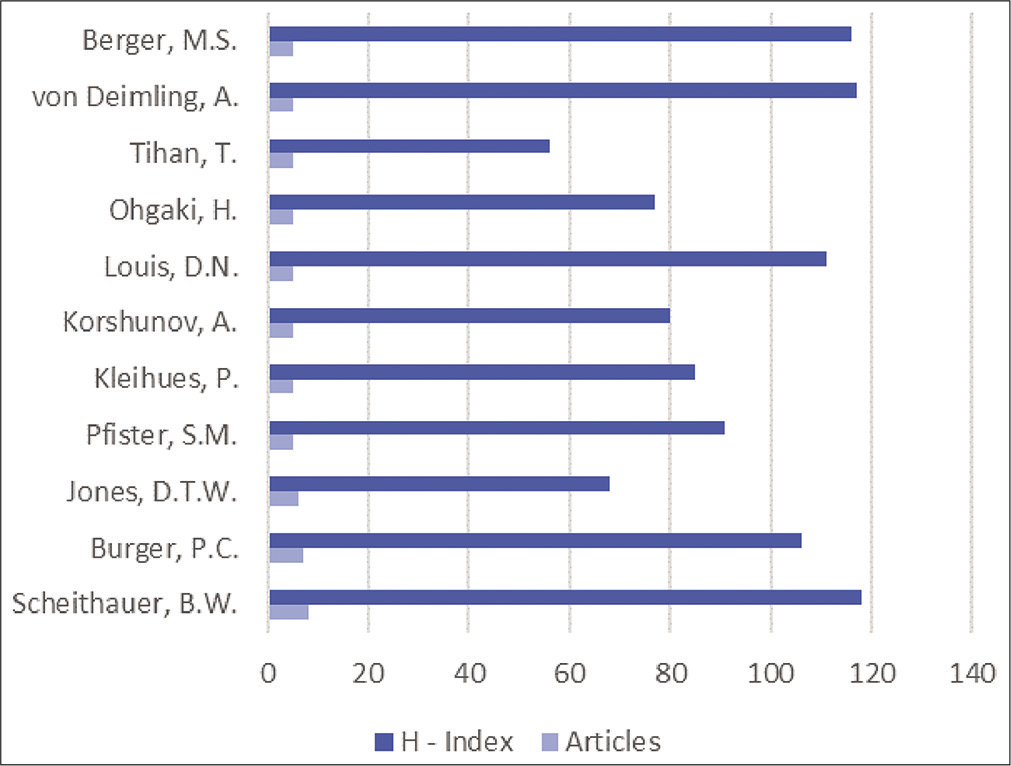
Results: The most-cited articles on astrocytoma had been cited 23,720 times. The top-cited article received a total of 682 citations, with an average of 34.1 citations annually. The list comprised eight clinical trials, in which the highest cited article received 625 citations. Articles were published from 1975 to 2015 with the 1995–2005 era as the most prolific period. Neuropathology studies were the most studied category, followed by clinical studies. The United States of America was the most significant contributor, with 49 published articles. The University of California San Francisco was the most contributing institution by producing 11 articles. Articles were published in 32 different journals led by the Cancer Research Journal, with a total of 12 publications. Approximately 160 authors contributed to the list in which Scheithauer, B.W. contributed the most with a total of eight articles.
Conclusion: This report clustered the most impactful articles on astrocytoma. It serves as an adequate tool to identify publication trends and helps in achieving evidence-based clinical practice.
Keywords: Astrocytoma, Bibliometric, Citation analysis, Low-grade glioma, Neurosurgery
INTRODUCTION
Astrocytoma (ICD: 9400/3) is a tumor of the central nervous system (CNS) originating from astrocytes, a glial cell with various essential supporting roles. Commonly, astrocytoma is integrated with oligodendroglioma in a more extensive nomenclature termed “glioma.”[
The preferred astrocytoma site of origin is the supratentorial compartment, mainly the frontal (25.6%) followed by temporal (19.6%) lobes, apart from pilocytic astrocytoma (infratentorial compartment) and primary glioblastoma (temporal lobe predilection in 31% of patients).[
Bibliometric analysis studies the impact of specific articles in their respective field. Since its inception in 1969, bibliometric analysis has gained popularity and approval among the scientific community, as it introduces junior physicians and others in different specialties to the subject analyzed in the article.[
MATERIALS AND METHODS
Search strategy
A title specific nontime restricted search using the Scopus database was performed in May 2020 utilizing the following keywords “astrocytoma, diffuse astrocytoma, anaplastic astrocytoma, pilocytic astrocytoma, subependymal giant cell astrocytoma, pleomorphic astrocytoma, and xanthoastrocytoma.” The outcome of the search was rearranged based on the citation count (CC), and the top 100 most-cited articles were collected for the authors’ review.
Data
The critical data of importance were collected and included the following: article title, authors, first authors specialty, institute of contribution, publishing journal, country of origin, year of publication, and CC. Critical appraisal of the top 100 articles from abstract to full articles was performed to categorize the studied titles into the following 10 categories: clinical, clinicopathological, clinicosurgical, medical management, surgical management, radiotherapy, chemotherapy, chemoradiotherapy, neuropathology, and neuroradiology.
Bibliometric parameters
Article-based cytometrics like CC were obtained from the Scopus database, and the citation per year (CY) was calculated based on the total number of citations divided by the number of years since their publication. Journal-based cytometric identifiers such as the Source Normalized Impact per Paper (SNIP), SCImago Journal Rank (SJR), and impact factor were obtained from the Scopus base.
RESULTS
Article, author, and journal analysis
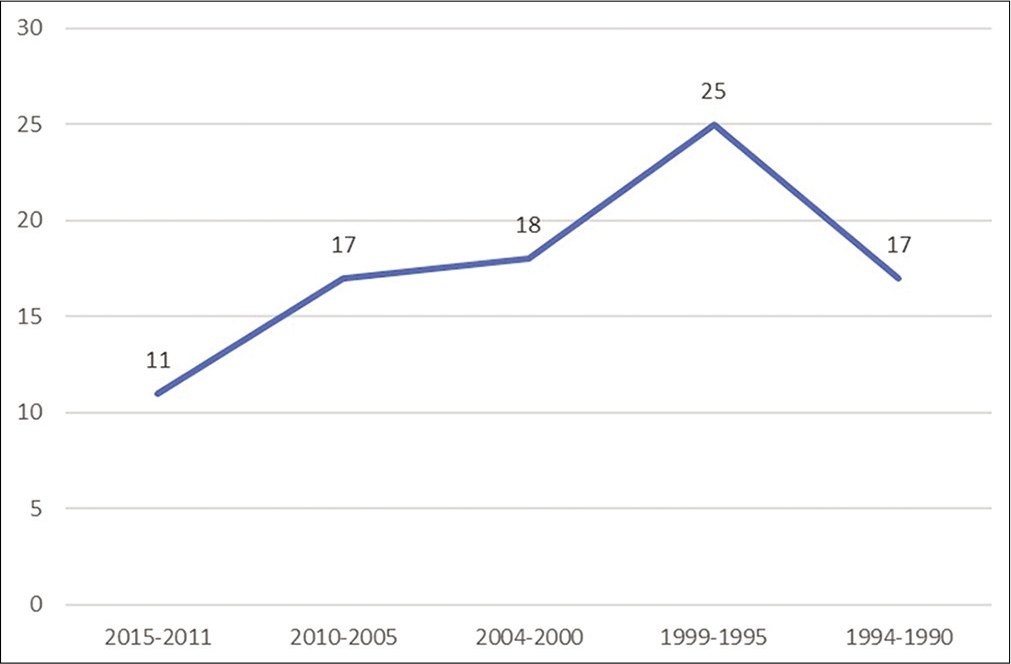
The search outcome showed 4303 articles that were published on astrocytoma. The top 100 most-cited articles received a total of 23,720 citations with an average CC of 237 cites per paper with an overall 9.2% rate of self-citations. The list of the most influential articles is listed in [
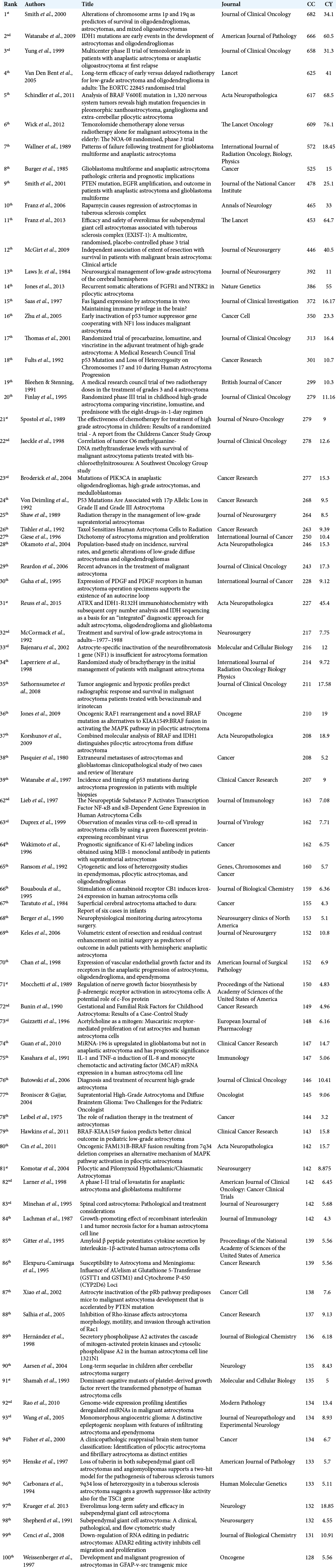
Subcategorical critical appraisal showed that approximately 50% of publications were discussing neuropathological studies, and clinical studies halted the 2nd most studied category by 17 articles in the list [
The USA was the most active in studying astrocytoma by collaborating in producing 67 articles in the top 100 most-cited articles [
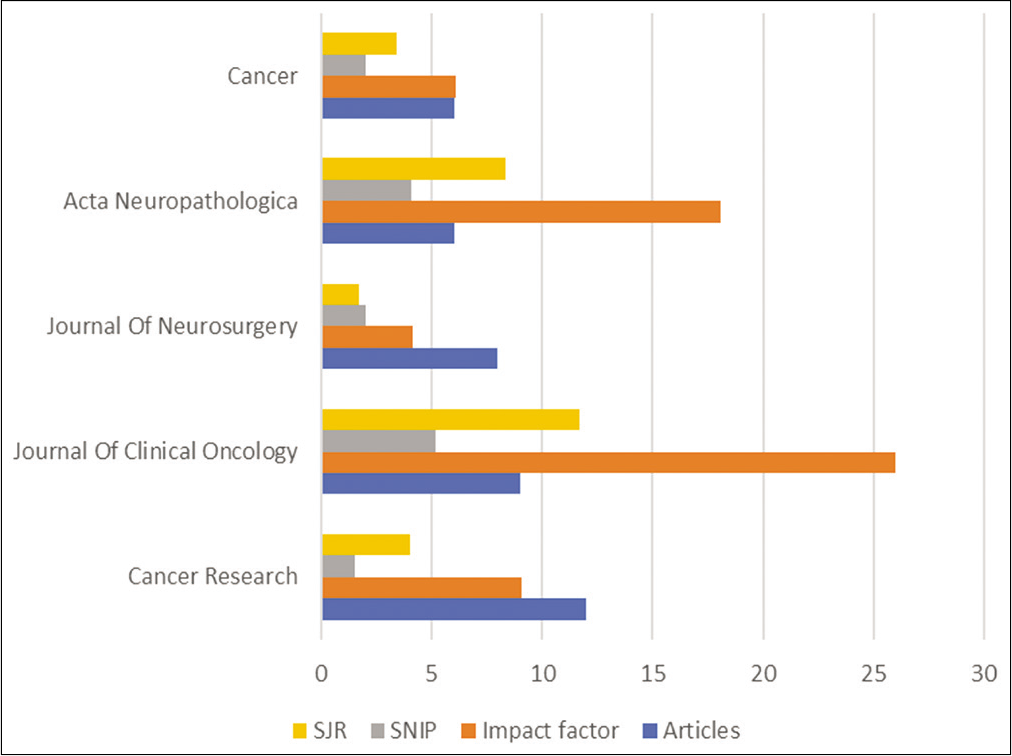
A quantified review of the 32 contributing journals showed that 8 journals contributed to at least 4 or more articles in the list. The Cancer Research Journal was the most productive by publishing 12 articles. The Journal of Clinical Oncology is the 2nd most prolific journal and had the highest impact (26), highest SNIP score (5.2), and highest SJR score (11.7) among the journals of contribution [
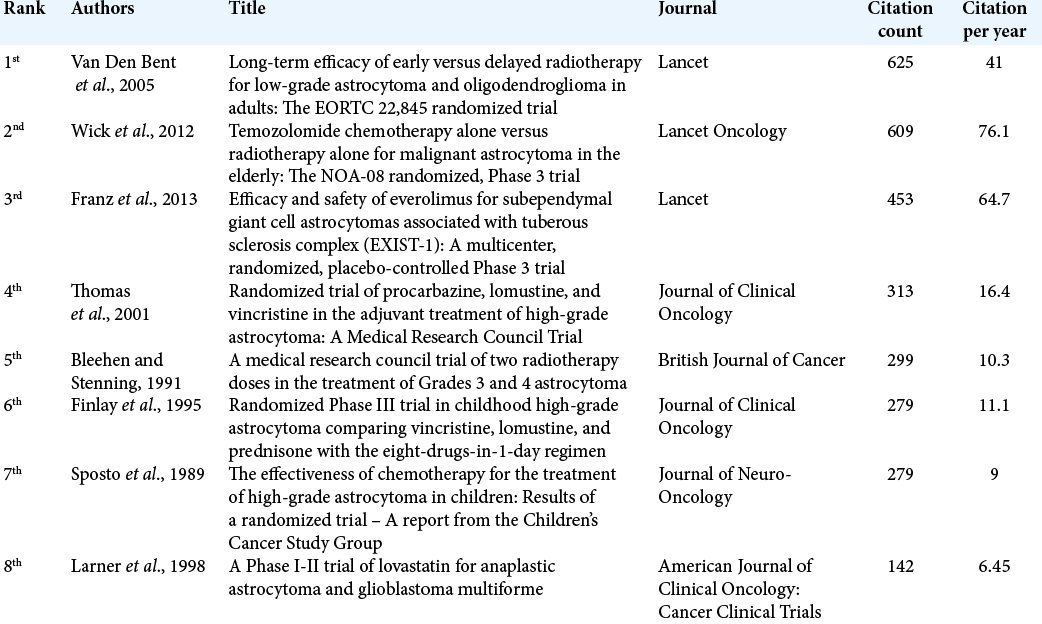
A summary of the eight identified clinical trials showed the most-cited clinical trial on astrocytoma was “Long-term Efficacy of early versus delayed radiotherapy for low-grade astrocytoma and oligodendroglioma in adults: The European Organization for Research and Treatment of Cancer (EORTC) 22,845 Randomized trial” that received a total of 625 citations and 41 citations/year which was published in The Lancet journal and authored by Van Den Bent et al. in 2005 [
The top most-cited article in the field of astrocytoma was published in 2000 by Smith et al. in the Journal of Clinical Oncology titled “Alterations of chromosome arms 1p and 19q as predictors of survival in oligodendrogliomas, astrocytomas, and mixed oligoastrocytomas” where it received a total of 682 citations and 34.1 citations/year.
DISCUSSION
The highest cited article in our top 100 list with 682 CC is “Alterations of chromosome arms 1p and 19q as predictors of survival in oligodendrogliomas, astrocytomas, and mixed oligoastrocytomas” by Smith et al. published in 2000 in the Journal of Clinical Oncology. However, it is ranked 9th in terms of CY (34.1). The large CC of the article stems from the novel finding of positive outcomes in 1p/19q co-deleted tumors. Of the 162 glioma samples collected, 79 were astrocytomas, 52 oligodendrogliomas, and 31 mixed oligoastrocytomas. There was a significant finding of high 1p/19q codeletion associated oligodendroglioma (P < 0.0001) and that it confers positive chemosensitivity (P = 0.03).[
The 2nd highest cited article with 666 citations is “Isocitrate dehydrogenase 1(IDH1) mutations are early events in the development of astrocytomas and oligodendrogliomas” by Watanabe et al. in 2009 in the American Journal of Pathology. It is ranked 4th in terms of CY (60.5). Of the 321 gliomas collected in the study, 130 showed IDH1 mutation. Diffuse astrocytoma showed the highest rate of having IDH mutation (88%) followed by secondary glioblastoma (82%). Primary glioblastoma and pilocytic astrocytoma were found to have low IDH mutation (5 and 10%, respectively).[
Further published articles have studied the physiology of IDH mutations concerning gliomas.[
Neuropathological studies comprised the majority of studied influential articles. The 1st ranked cited article (ranked 14th overall) with 386 CC and 55 CY is “Recurrent somatic alterations of FGFR1 and NTRK2 in pilocytic astrocytoma” by Jones et al. in 2013 in Nature Genetics journal. The authors found that pilocytic astrocytoma is a single pathway tumor with over activation of mitogen-activated protein kinase due to mutations in FGFR1, NTRK2, and PTPN11 genes.[
The most-cited clinical study (ranked 8th overall) in the list accounted for 525 CC, and 15 CY is “Glioblastoma multiforme and anaplastic astrocytoma pathologic criteria and prognostic implications” by Burger et al. in 1985 in the Cancer journal. In this article, two groups of patients with high-grade glioma (known as malignant astrocytic gliomas at the time) were studied to define histologic variants based on three-tiered systems and its associated outcome. They concluded that malignant astrocytic gliomas could be classified into anaplastic astrocytoma and glioblastoma multiforme, with the latter conferring a more unfortunate outcome than the former.[
The most influential publication on radiotherapeutic management of astrocytoma (ranked 4th overall) was “Long-term efficacy of early versus delayed radiotherapy for low-grade astrocytoma and oligodendroglioma in adults: The EORTC 22845 randomized trial” by Van Den Bent et al. in 2005 in the Lancet journal with 525 CC and 41 CY. The randomized controlled trial (RCT) segregated patients into an early radiotherapy group (n = 157) and late radiotherapy group (n = 157) and found that early radiotherapy group had a better PFS with a median of 5.3 years than late radiotherapy group with a median of 3.4 years (P < 0.0001).[
Another RCT on radiotherapy for astrocytoma was the 3rd ranked cited article (ranked 19th overall) with 299 CC and 10.3 CY is “A medical research council trial of two radiotherapy doses in the treatment of Grades 3 and 4 astrocytoma” by Bleehen and Stenning in 1992 in the British Journal of Cancer. Of the 474 patients with high-grade astrocytoma, 318 were allocated to high-dose radiation course (60 Gy in 30 fractions over 6 weeks) and 156 to low-dose course (45 Gy in 20 fractions over 4 weeks). The trial showed modest improvement and statistical significance in median survival from 9 months to 12 months in the high-dose receiving group.[
The analyzed studies entertaining chemotherapy and radiation therapy treatment in astrocytoma showed three published RCT. The 1st ranked cited article (ranked 6th overall) with 609 CC and 76.1 CY is “TMZ chemotherapy alone versus radiotherapy alone for malignant astrocytoma in the elderly: The NOA-08 randomized, Phase 3 trial” by Wick et al. in 2012 in the Lancet Oncology journal. The trial allocated 373 patients with high-grade astrocytoma into TMZ group (n = 195) and radiotherapy group (n = 178), with median OS of 9.6 months in radiotherapy (95% CI 8.2–10.8) versus 8.6 months in TMZ (7.3–10.2) (P [noninferiority] = 0.033). The MGMT promoter methylated high-grade astrocytoma patients had a longer OS than nonmethylated group (median 11.9 vs. 8.2 months, P = 0.014). The event-free survival was higher in the methylated group receiving TMZ (median of 8.4 months vs. 4.6), and the nonmethylated group had a higher event-free survival when receiving radiotherapy (median 4.6 months vs. 3.3).[
The 2nd ranked cited article in chemoradiation (ranked 20th overall) with 279 CC and 11.16 CY is “Randomized Phase III trial in childhood high-grade astrocytoma comparing vincristine, lomustine, and prednisone with the eight-drugs-in-1-day regimen” by Finlay et al. in 1995 in Journal of Clinical Oncology. They concluded that no difference in PFS and OS in the eight-drugs-in-1-day group versus vincristine, lomustine, and prednisone group; however, PFS improved in the extent of resection (>90%) and nonmidline astrocytoma.[
The assessment of articles discussing medical management used in astrocytoma signified two published RCT. The 1st ranked cited article (ranked 11th overall) with 453 CC and 64.7 CY is “Efficacy and safety of everolimus for subependymal giant cell astrocytomas associated with tuberous sclerosis complex (EXIST-1): A multicenter, randomized, placebo-controlled Phase 3 trial” by Franz et al. in 2013 in the Lancet journal. Patients with SEGA (n = 78) who received everolimus had 35% reduction of at least 50% tumor volume than patients who did not receive everolimus (n = 39).[
A top 50 low-grade glioma bibliometric analysis was published by Atci et al. in 2019.[
Our data showed that 50% of the top 100 articles were published between 1995 and 2005, with the majority between 1995 and 1999. Earlier publications were focused on surgical and radiation management, and over 20 years, the goal was directed on studying molecular pathways that play a significant role in prognosis and their clinical significance in directing a new gene-targeted therapy for astrocytoma.
Limitations
Bibliometric studies have their inherent limitations, such as over signifying old studies by CC accumulation and under signifying recently published impactful articles; this disadvantage can be rectified by utilizing the CY for articles. In addition, articles with high CC do not necessarily signify major impact, as some studies are cited to demonstrate a weakness or error in that study. The source of citation, such as authors self-citing their publications and in-house citation, reflects inherent bibliometric study limitations. We used one search engine, that is, Scopus, and may have missed other impactful studies. A topic-specific limitation to astrocytoma is that some significant articles studying astrocytoma are titled glioma, which is overlooked in our review, but focusing on astrocytoma alone makes our bibliometric representation of the impactful articles more specific.
CONCLUSION
We performed a comprehensive review of astrocytoma citations and collected the top 100 articles. Most articles were published between 1995 and 2005, with 8 RCTs. The highest ranked authors were neuropathologists followed by neuro-oncologists. The highest ranked journal was Cancer Research, followed by the Journal of Clinical Oncology. Most articles were focused on the neuropathology category, with great emphasis on molecular diagnosis and its potential related outcome. This article is to serve as a guide and introduction for medical specialties related to neuro-oncology interested in astrocytoma; it highlights the most impactful studies, the chronological trend, and to govern future studies in neuro-oncology.
Declaration of patient consent
Patients consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Alfaifi A, AlMutairi O, Allhaidan M, Alsaleh S, Ajlan A. The top 50 most-cited articles on acoustic neuroma. World Neurosurg. 2018. 111: e454-64
2. Almutairi O, Albakr A, Al-Habib A, Ajlan A. The top-100 most-cited articles on meningioma. World Neurosurg. 2017. 107: 1025-32.e5
3. Atci IB, Yilmaz H, Samanci MY. The top 50 most-cited articles on low-grade glioma: A bibliometric analysis. Br J Neurosurg. 2019. 33: 171-5
4. Bleehen NM, Stenning SP. A medical research council trial of two radiotherapy doses in the treatment of grades 3 and 4 astrocytoma. The medical research council brain tumour working party. Br J Cancer. 1992. 64: 769-74
5. Burger PC, Vogel FS, Green SB, Strike TA. Glioblastoma multiforme and anaplastic astrocytoma, Pathologic criteria and prognostic implications. Cancer. 1985. 56: 1106-11
6. Dang L, White DW, Gross S, Bennett BD, Bittinger MA, Driggers EM. Cancer-associated IDH1 mutations produce 2-hydroxyglutarate. Nature. 2009. 462: 739-44
7. Dolecek TA, Propp JM, Stroup NE, Kruchko C. CBTRUS statistical report: Primary brain and central nervous system tumors diagnosed in the United States in 2005-2009. Neuro Oncol. 2012. 14: v1-49
8. Finlay JL, Boyett JM, Yates AJ, Wisoff JH, Milstein JM, Geyer JR. Randomized phase III trial in childhood high-grade astrocytoma comparing vincristine, lomustine, and prednisone with the eight-drugs-in-1-day regimen, Childrens cancer group. J Clin Oncol. 1995. 13: 112-23
9. Franz DN, Belousova E, Sparagana S, Bebin EM, Frost M, Kuperman R. Efficacy and safety of everolimus for subependymal giant cell astrocytomas associated with tuberous sclerosis complex (EXIST-1): A multicentre, randomised, placebo-controlled phase 3 trial. Lancet. 2013. 381: 125-32
10. Franz DN, Leonard J, Tudor C, Chuck G, Care M, Sethuraman G. Rapamycin causes regression of astrocytomas in tuberous sclerosis complex. Ann Neurol. 2006. 59: 490-8
11. Giordano F, Moscheo C, Lenge M, Biagiotti R, Mari F, Sardi I. Neurosurgical treatment of subependymal giant cell astrocytomas in tuberous sclerosis complex: A series of 44 surgical procedures in 31 patients. Childs Nerv Syst. 2020. 36: 951-60
12. Goodenberger ML, Jenkins RB. Genetics of adult glioma. Cancer Genet. 2012. 205: 613-21
13. Guo X, Gao L, Wang Z, Feng C, Xing B. Top 100 most-cited articles on pituitary adenoma: A bibliometric analysis. World Neurosurg. 2018. 116: e1153-67
14. Houillier C, Wang X, Kaloshi G, Mokhtari K, Guillevin R, Laffaire J. IDH1 or IDH2 mutations predict longer survival and response to temozolomide in low-grade gliomas. Neurology. 2010. 75: 1560-6
15. Johnson DR, Galanis E. Medical management of high-grade astrocytoma: Current and emerging therapies. Semin Oncol. 2014. 41: 511-22
16. Jones DT, Hutter B, Jäger N, Korshunov A, Kool M, Warnatz HJ. Recurrent somatic alterations of FGFR1 and NTRK2 in pilocytic astrocytoma. Nat Genet. 2013. 45: 927-32
17. Louis DN, Perry A, Reifenberger G, von Deimling A, FigarellaBranger D, Cavenee WK. The 2016 World Health Organization classification of tumors of the central nervous system: A summary. Acta Neuropathol. 2016. 131: 803-20
18. Ostrom QT, Gittleman H, Liao P, Vecchione-Koval T, Wolinsky Y, Kruchko C. CBTRUS statistical report: Primary brain and other central nervous system tumors diagnosed in the United States in 2010-2014. Neuro Oncol. 2017. 19: v1-88
19. Ostrom QT, Gittleman H, Truitt G, Boscia A, Kruchko C, Barnholtz-Sloan JS. CBTRUS statistical report: Primary brain and other central nervous system tumors diagnosed in the United States in 2011-2015. Neuro Oncol. 2018. 20: iv1-86
20. Pedersen CL, Romner B. Current treatment of low grade astrocytoma: A review. Clin Neurol Neurosurg. 2013. 115: 1-8
21. Pritchard A. Statistical bibliography or bibliometrics?. J Doc. 1969. 25: 348-9
22. Roth J, Roach ES, Bartels U, Jozwiak S, Koenig MK, Weiner HL. Subependymal giant cell astrocytoma: Diagnosis, screening, and treatment, Recommendations from the international tuberous sclerosis complex consensus conference, 2012. Pediatr Neurol. 2013. 49: 439-44
23. Sanai N, Chang S, Berger MS. Low-grade glioma in adults. J Neurosurg. 2011. 115: 948-65
24. Sathornsumetee S, Rich JN, Reardon DA. Diagnosis and treatment of high-grade astrocytoma. Neurol Clin. 2007. 25: 1111-39
25. Schiff D. Low-grade gliomas. Continuum (Minneap Minn). 2017. 23: 1564-79
26. Smith JS, Perry A, Borell TJ, Lee HK, O’Fallon J, Hosek SM. Alterations of chromosome arms 1p and 19q as predictors of survival in oligodendrogliomas, astrocytomas, and mixed oligoastrocytomas. J Clin Oncol. 2000. 18: 636-45
27. Sposto R, Ertel IJ, Jenkin RD, Boesel CP, Venes JL, Ortega JA. The effectiveness of chemotherapy for treatment of high grade astrocytoma in children: Results of a randomized trial. A report from the childrens cancer study group. J Neurooncol. 1989. 7: 165-77
28. van den Bent MJ, Afra D, de Witte O, Hassel MB, Schraub S, Hoang-Xuan K. Long-term efficacy of early versus delayed radiotherapy for low-grade astrocytoma and oligodendroglioma in adults: The EORTC 22845 randomised trial. Lancet. 2005. 366: 985-90
29. Watanabe T, Nobusawa S, Kleihues P, Ohgaki H. IDH1 mutations are early events in the development of astrocytomas and oligodendrogliomas. Am J Pathol. 2009. 174: 1149-53
30. Wick W, Platten M, Meisner C, Felsberg J, Tabatabai G, Simon M. Temozolomide chemotherapy alone versus radiotherapy alone for malignant astrocytoma in the elderly: The NOA-08 randomised, phase 3 trial. Lancet Oncol. 2012. 13: 707-5