- Department of Mechanical Engineering, Northern Arizona University, Flagstaff,
- Department of Neurosurgery, Barrow Neurological Institute, Phoenix, Arizona, United States.
Correspondence Address:
Timothy A. Becker, Department of Mechanical Engineering, Northern Arizona University, Flagstaff, Arizona, United States.
DOI:10.25259/SNI_576_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: William C. Merritt1, Holly F. Berns1, Andrew F. Ducruet2, Timothy Andrew Becker1. Definitions of intracranial aneurysm size and morphology: A call for standardization. 06-Oct-2021;12:506
How to cite this URL: William C. Merritt1, Holly F. Berns1, Andrew F. Ducruet2, Timothy Andrew Becker1. Definitions of intracranial aneurysm size and morphology: A call for standardization. 06-Oct-2021;12:506. Available from: https://surgicalneurologyint.com/surgicalint-articles/11154/
Abstract
Background: Intracranial aneurysms (IAs) are classified based on size (maximal dome diameter) as well as additional parameters such as neck diameter and dome-to-neck ratio (DNR). The neurosurgical literature includes a wide variety of definitions for both IA size and neck classifications. Standardizing the definitions of IA size and wide-neck classifications would help eliminate inconsistencies and potential misunderstandings of aneurysm morphology and rupture risk.
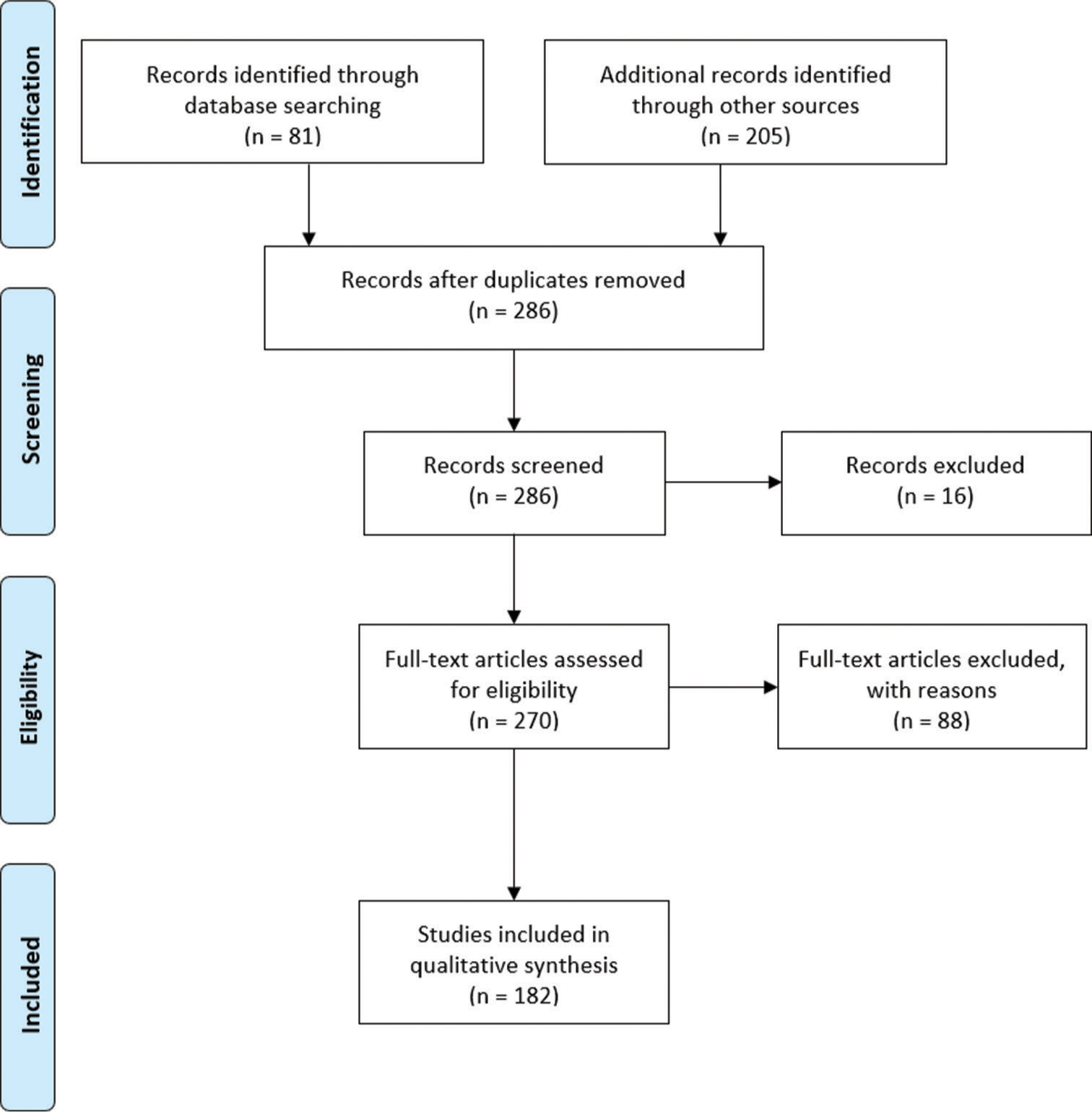
Methods: We queried the MEDLINE (EBSCO) database using the terms “unruptured IA” and (“small” or “medium” or “large”) and filtered based on publication date, language, and scholarly journals. The resulting articles and their references were further screened for eligibility. This identified 286 records, of which 104 were excluded, leaving 182 articles for analysis. The review found several different IA size classifications and neck classifications.
Results: A review of the existing literature describing size and neck classifications revealed 13 size classifications for small aneurysms, four classifications for medium aneurysms, 15 classifications for large aneurysms, and one classification for giant aneurysms. There were also seven different wide-neck classifications found.
Conclusion: It is imperative that a standardization in classification be implemented to help interventionalists make the most informed decisions regarding emerging treatment options as new endovascular technologies and devices are emerging with indications based around these classifications. Based on the database findings, this article recommends standardized quantitative measurement ranges for IA size and neck classifications.
Keywords: Intracranial aneurysm, Neurovascular anatomy, Aneurysm size, Aneurysm morphology
INTRODUCTION
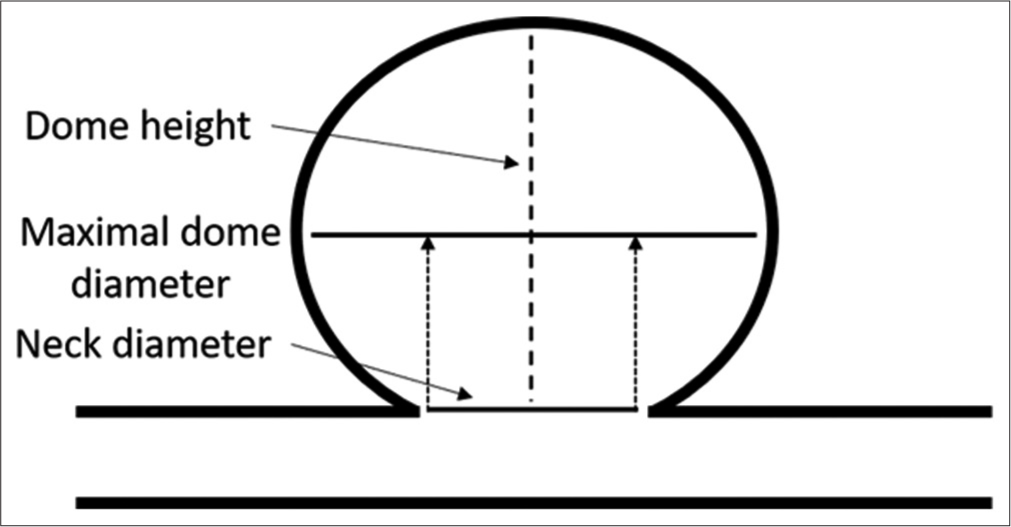
Recent advances in endovascular treatment options for intracranial aneurysms (IAs) have brought increased attention to the various morphological characteristics of IAs and how these characteristics may affect endovascular device selection and the safety and efficacy of treatment. IA classification has typically been based on maximal dome diameter (size) in combination with other parameters such as maximal dome diameter to neck diameter ratio (DNR) and neck diameter [
A wide variety of definitions for both IA size and neck type have been reported, but the optimal definitions for IA size remain unclear. Existing definitions for IA size have been based around the large natural history of IA studies performed, including in the International Study of Unruptured IAs (ISUIA) and The Natural Course of Unruptured Cerebral Aneurysms in a Japanese Cohort (UCAS) study. These studies analyzed varying factors that contribute to IA growth and rupture, to better understand the progression of the disease. A major finding was that the size of the IA correlated to rupture risk and attempted to stratify rupture risk based on IA diameter. The first ISUIA was published in 1998, which was a retrospective study, initially classified aneurysms by the following size definitions based on risk of rupture: small (<10 mm), large (10 mm–25 mm), and giant (>25 mm). The second ISUIA was published in 2003, which was a prospective study, further stratified the aneurysm sizes by including a 4th classification based on risk of rupture: small (<7 mm), medium (7 mm–12 mm), large (12 mm–25 mm), and giant (>25 mm). However, clinicians and researchers in Japan and Finland noticed that they were observing ruptures in small aneurysms much more frequently than what was reported by the ISUIA. To better understand this disparity, the UCAS study was performed and published in 2012. UCAS stratified aneurysms by size based upon rates of rupture: small (<5 mm), medium (5 mm–10 mm), large (10 mm–25 mm), and giant (>25 mm).
As additional research articles and case studies have been published, there has not been a uniform adoption of any single size classification definition system. These inconsistencies in definitions can be a major limitation, as current FDA indications for use include specific IA size and neck size classifications, such as in the expanded small/ medium aneurysm indication for Medtronic’s Pipeline Embolization Device.[
METHODS
This literature review was performed by identifying applicable articles and screening them for eligibility [
RESULTS
The reviewed articles consistently classified IAs as “small”, “medium”, “large”, or “giant”. However, the authors did not consistently describe how the measurements were performed (i.e., maximal sac diameter, and midline dome diameter) and measurement ranges for each classification were inconsistent, affecting the ability to compare classifications between articles.
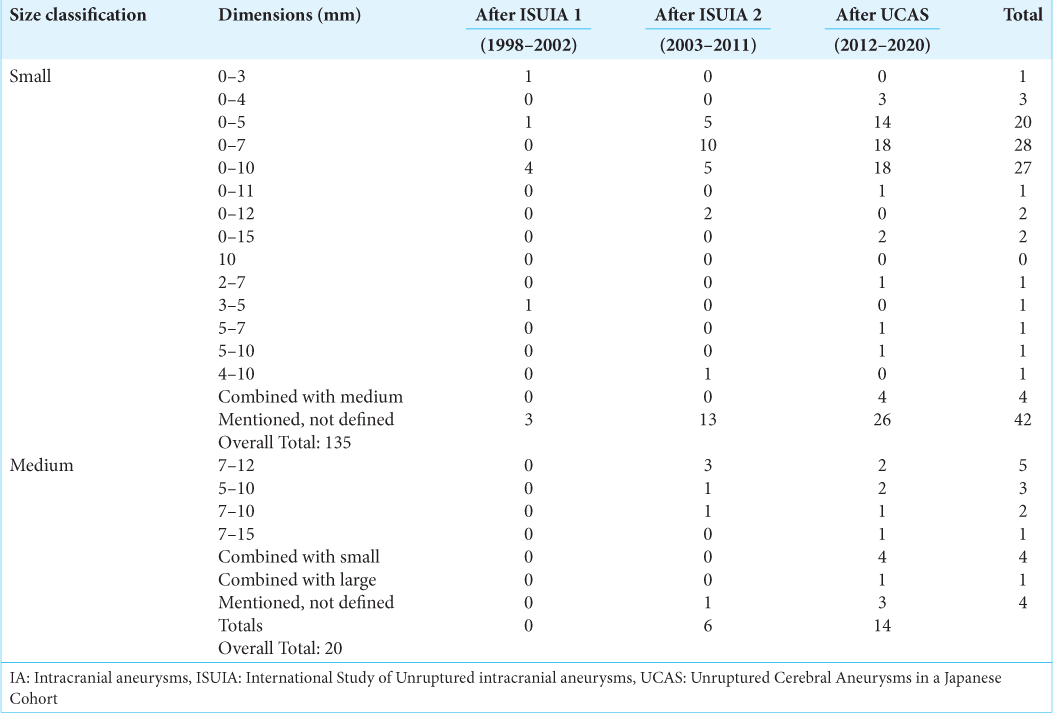
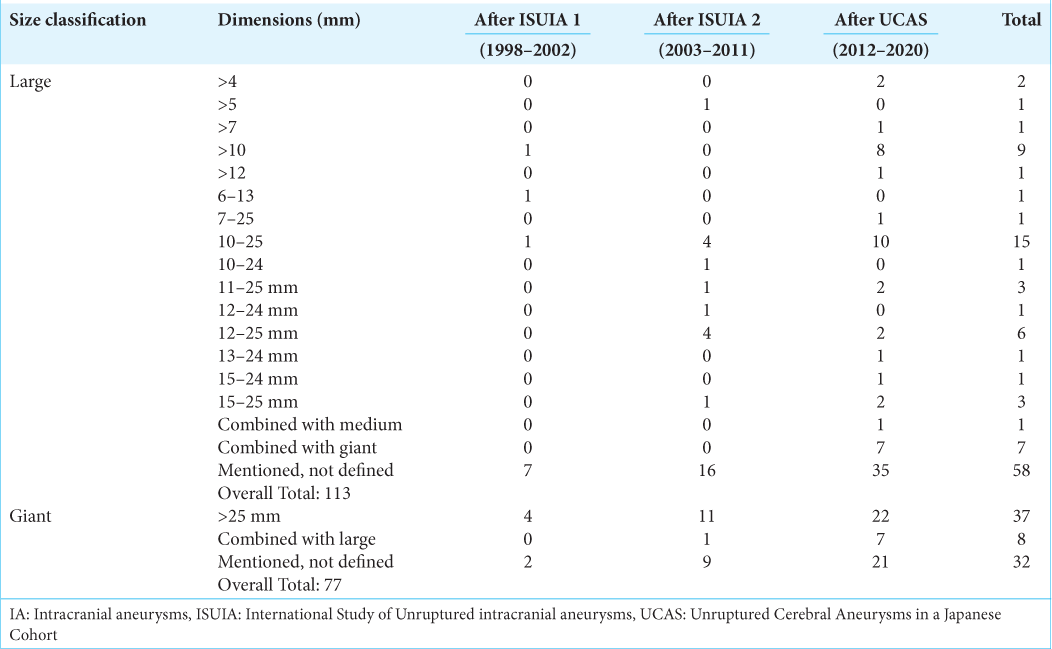
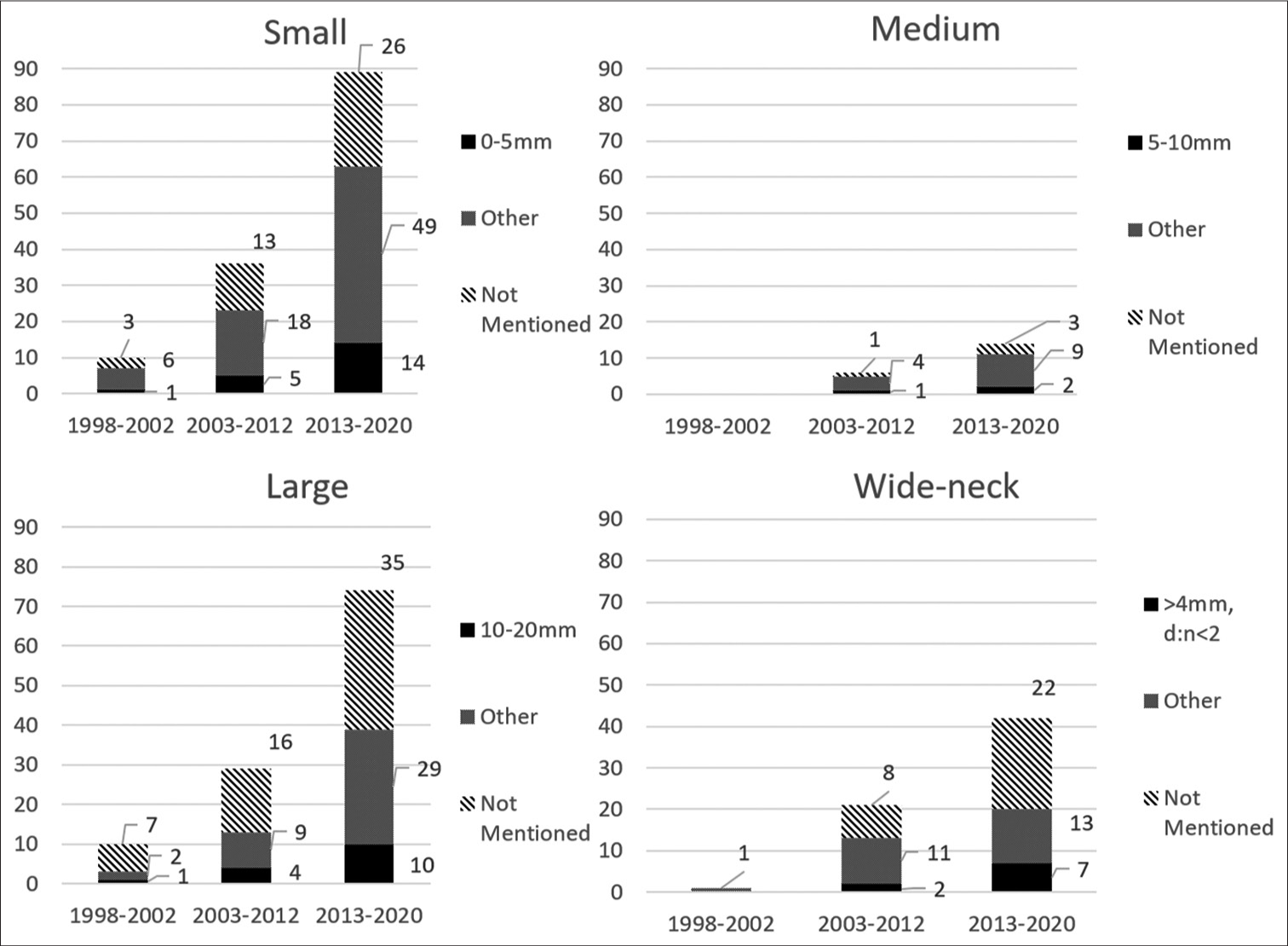
The review identified several different size classifications for IAs. There were 13 quantitative size classification definitions (i.e., 0mm – 5 mm diameter) for “small” aneurysms, 4 classification definitions for “medium” aneurysms, 15 classification definitions for “large” aneurysms, and one classification for giant aneurysms. There were seven wide-neck classification definitions and one very wide-neck classification definition. Articles that mentioned an IA size classification but failed to define/quantify this classification were also noted. The differing classification definitions are listed in [
In total, small IAs were mentioned in 135 articles (74.2%), medium in 20 articles (10.9%), large in 113 articles (62.1%), and giant in 77 articles (42.3%). Wide-neck IAs were mentioned in 64 articles (35.2%), and very wide-neck IAs in two articles (1.1%). Giant IAs were defined the most consistently with all definitions stating IAs >25 mm in maximal diameter.
Small IA dimensions, ranging from 0–5 mm to 0–10 mm, were mentioned in 56% of the references. In 31% of the references, no dimension was associated with the small classification [
Large IA dimensions, ranging from > 10 mm to 10–25 mm, were mentioned in 21% of the references. In 51% of the references, no dimension was associated with the large classification [
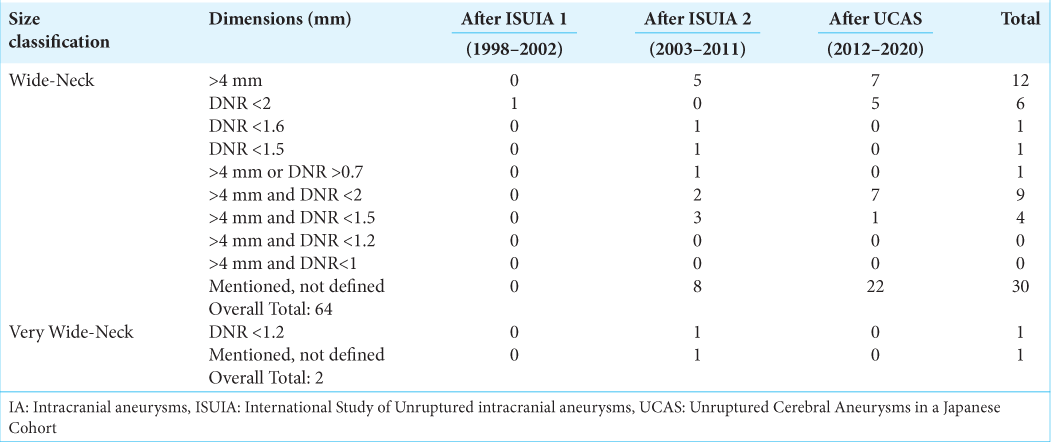
Wide-neck IA dimensions, defining a neck width >4 mm, was mentioned in 44% of the references. DNR values were highly variable, but a wide-neck associated with a DNR <2 was most prevalent (30% of the references). In 47% of the references, no dimension was associated with the wide-neck classification [
DISCUSSION
Existing classifications for IA size have been derived from large natural history studies of unruptured IAs and are derived from risk of rupture. The results from the first ISUIA study (retrospective group) in 1998, the second ISUIA trial (prospective group) in 2003, and The Natural Course of UCAS study in 2012 largely influenced current definitions for IA size classification.[
As new morphology definitions were adopted from these studies, this has led to more variability as many articles continue to use definitions from prior studies. This lack of consistency in size definition is an issue considering that many articles mention IA size classifications without actually defining them (in total, 91.2% of size classifications were not defined) [
It is also important to note the differences between maximal dome diameter and height. Maximum dome diameter is properly defined as the widest IA measurement perpendicular to the aneurysm height.[
Small IAs
Small IAs are mentioned the most in the reviewed literature. This is likely due to the extensive research performed on small IAs and the implication of their size on risk of rupture.[
Medium IAs
Medium IAs are mentioned the least in the reviewed literature. They are often included in either small or large IA classifications (i.e., “small and medium aneurysms [<10 mm in diameter]”), or are not defined at all. When medium aneurysms were included in small or large IA classifications, it was tallied as “combined.” There were several articles that had a data range for what could have been classified as a medium IA, but the medium classification was not mentioned (surrounding size data ranges were classified as small and large, but no mention of medium IA was made). The medium IA classification was not used in the first ISUIA study but has been adopted in later studies.[
Large IAs
Large IAs were mentioned but left undefined 51% of the time, more than any other classification in the reviewed literature. In many references that focused on small IAs, the large classification was used as a catch-all for anything that fell outside the small IA classification.
Giant IAs
Giant IAs were classified most consistently in the reviewed literature. This could be because the giant IA classification is one of the oldest, dating back to 1969.[
Wide-neck IAs
Wide-neck IAs were first defined in 1994 as an IA with a neck ≥4 mm.[
Recently, Hendricks et al. (2019) performed a focused systematic review of the neurosurgical literature directed at wide-neck IA definition and clinical implication. This review also found a lack of consistency and identified seven unique definitions for wide-neck aneurysms. The most commonly found definition for wide-neck IA was a neck diameter >4 mm or DNR < 2.[
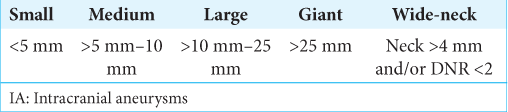
Taking into account the evolution of the IA size and IA neck classification trends in the literature, and the fact that unclassified aneurysms are still prevalent in the literature, we recommend the following standardized classification for aneurysm geometry: maximal dome diameter classifications, and wide neck classification [
A major limitation of the ISUIA studies and their resulting size classification systems was that the cohorts evaluated were over 90% Caucasian and did not sufficiently include demographics that demonstrate higher rates of aneurysm rupture such as Japanese and Finnish patients.[
Aspect ratio, defined as the ratio between IA height and neck diameter, has also been shown to have clinical implications on both treatment outcome and risk of rupture. This ratio has not been studied as extensively but may represent an additional important morphological parameter for predicting treatment outcomes of IAs.[
Limitations
This literature review was not intended to be a comprehensive analysis of every paper that has classified an aneurysm by size, but rather a structured sampling of the literature to highlight the inconsistencies and trends in the definitions for IA size classification.
CONCLUSION
There is tremendous variability in the existing definitions for IA size and neck classification. Flexibility in size definition was more acceptable when it mainly related to statistical stratification of IA rupture risk in studies. With new endovascular technologies emerging with indications based around these size classifications, it is imperative that standardization in classification definition is implemented. Standardizing the definitions of IA size and neck classifications would help eliminate inconsistencies and potential misunderstandings. We hope that this review spurs further discussion that results in a more consistent, standardized intracranial classification system that allows surgeons, regulatory bodies, and medical device developers to quickly identify suitable treatment devices for patient-specific IA dimensions and morphologies.
The general trend can be seen in IA size classification moving towards the following definitions: small <5 mm, medium >5 mm-10 mm, large >10 mm–25 mm, and giant >25 mm, which follows the Japanese UCAS study size classifications.[
With the current natural history of IA data available, this size classification system represents the most inclusive of higher-risk demographics and thus is recommended as the most appropriate size classification to adopt. The data also suggest that definition of a wide-neck aneurysm be an IA with a neck diameter >4 mm or DNR <2 be adopted as a standard until data can support reducing the DNR to a lower value. Whether, these definitions comprise the most appropriate system for IA size classification is yet to be determined and is a subject for future discussion and research.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Barrow DL, Alleyne C. Natural history of giant intracranial aneurysms and indications for intervention. Clin Neurosurg. 1995. 42: 214-44
2. Brinjikji W, Cloft HJ, Kallmes DF. Difficult aneurysms for endovascular treatment: Overwide or undertall?. AJNR Am J Neuroradiol. 2009. 30: 1513-7
3. Chen J, Liu J, Zhang Y, Tian Z, Wang K, Zhang Y. China intracranial aneurysm project (CIAP): Protocol for a registry study on a multidimensional prediction model for rupture risk of unruptured intracranial aneurysms. J Transl Med. 2018. 16: 1-9
4. Debrun GM, Aletich VA, Kehrli P, Misra M, Ausman JI, Fady C. Selection of cerebral aneurysms for treatment using guglielmi detachable coils: The Preliminary University of illinois at Chicago experience. Neurosurgery. 1998. 43: 1281-95
5. Duan Z, Li Y, Guan S, Ma C, Han Y, Ren X. Morphological parameters and anatomical locations associated with rupture status of small intracranial aneurysms. Sci Rep. 2018. 8: 1-7
6. Hanel RA, Kallmes DF, Lopes DK, Nelson PK, Siddiqui A, Jabbour P. Prospective study on embolization of intracranial aneurysms with the pipeline device: The PREMIER study 1 year results. J Neurointerv Surg. 2020. 12: 62-6
7. Hendricks BK, Yoon JS, Yaeger K, Kellner CP, Mocco J, de Leacy RA. Wide-neck aneurysms: Systematic review of the neurosurgical literature with a focus on definition and clinical implications. J Neurosurg. 2019. 133: 159-165
8. Morita A, Kirino T, Hashi K, Aoki N. The natural course of unruptured cerebral aneurysms. N Engl J Med. 2012. 366: 2474-82
9. Morley TP, Barr HW. Giant intracranial aneurysms: Diagnosis, course, and management. Neurosurgery. 1969. 16: 73-94
10. Parlea L, Fahrig R, Holdsworth DW, Lownie SP. An analysis of the geometery of saccular intracranial aneurysms. AJNR Am J Neuroradiol. 1999. 20: 1079-89
11. Raghavan ML, Ma B, Harbaugh RE. Quantified aneurysm shape and rupture risk. J Neurosurg. 2005. 102: 355-62
12. Ujiie H, Tamano Y, Sasaki K, Hori T. Is the aspect ratio a reliable index for predicting the rupture of a saccular aneurysm?. Neurosurgery. 2001. 48: 495-503
13. Wiebers D, Whisnant J, Forbes G, Meissner I, Brown R. Unruptured intracranial aneurysms-risk of rupture and risks of surgical intervention. N Engl J Med. 1998. 339: 1725-33
14. Wiebers D, Whisnant J, Huston J, Meissner I, Brown RD, Piepgras DG. Unruptured intracranial aneurysms: Natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet. 2003. 12: 103-10
15. Zubillaga F, Guglielmi G, Vinuela F, Duckwiler GR. Endovascular occlusion of intracranial aneurysms with electrically detachable coils: Correlation of aneurysm neck size and treatment results. AJNR Am J Neuroradiol. 1994. 15: 815-20