Abstract
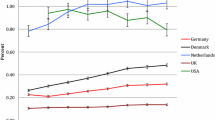
Background: Antipsychotic prescribing in children has risen in many countries; however, the safety of these agents in the young has not yet been fully established. Potentially fatal antipsychotic-related adverse events include cardiac complications and neuroleptic malignant syndrome.
Objective: The objective of this study was to investigate mortality in children and adolescents taking antipsychotic medication.
Methods: The General Practice Research Database (GPRD) was used as a data source for this study. Cases were identified from a cohort of patients previously studied. The study population encompassed all patients aged 18 years and under who received at least one prescription for an antipsychotic from 1 January 1992 to 31 December 2005. Patients were followed from the date of the first antipsychotic drug prescription until the earliest occurrence of a code of death, age >18 years or the end of the study period. Cases of death were identified by screening patients’ medical records for clinical or referral events with events indicating death, or if a transferred-out patient has a ‘transfer out reason’ specified as ‘death’. Confirmation of cases was carried out by examining individual patient profiles and from questionnaires sent to GPs. If necessary, the death certificates and/or post mortem reports were obtained by the source data verification service the GPRD provide. Once cases of death were identified, crude mortality rate (CMR) and standardized mortality ratio (SMR) were calculated. Baseline mortality rates were obtained from the Office for National Statistics. A modified WHO causality assessment was conducted to determine the likelihood of a relationship between the drug and an event of death.
Results: The cohort contained 2767 patients who received at least one antipsychotic prescription. There were 30 deceased cases in the cohort. The GP questionnaire response rate was 97%. Of the 30 cases, 24 were related to preexisting medical conditions, including neoplastic diseases and HIV. After excluding these patients, six cases of death from 5963 person-years and 1958 treatment-years remained. The median age of death was 17 years (interquartile range 14–17.75). The overall CMR was 1.01 per 1000 person-years at risk (95% CI 0.20, 1.81) and SMR was 4.03 (95% CI 1.48, 8.76). Of the six cases, only one was deemed possibly associated with antipsychotic therapy, based on the causality assessment analysis conducted; CMR based on this case was 0.51 per 1000 treatment-years (95% CI 0.09, 2.89). The remaining five cases of death were unlikely to be associated with antipsychotic therapy.
Conclusions: Our study demonstrated an elevated SMR in patients exposed to antipsychotics. However, the elevated SMR was unlikely caused by antipsychotic treatment, but would suggest the possibility of inadequate management or poor control of patients’ underlying medical conditions prior to death.


Similar content being viewed by others
References
Cooper WO, Hickson GB, Fuchs C, et al. New users of antipsychotic medications among children enrolled in TennCare. Arch Pediatr Adolesc Med 2004; 158: 753–9
Crystal S, Olfson M, Huang C, et al. Broadened use of atypical antipsychotics: safety, effectiveness, and policy challenges. Health Aff (Millwood) 2009; 28: w770–81
Olfson M, Blanco C, Liu L, et al. National trends in the outpatient treatment of children and adolescents with antipsychotic drugs. Arch Gen Psychiatry 2006; 63(6): 679–85
Schirm E, Tobi H, Zito JM, et al. Psychotropic medication in children: a study from the Netherlands. Pediatrics 2001; 108(2): e25 [online]. Available from URL: http://www.pediatrics.org/cgi/content/full/108/2/e25 [Accessed 2011 May 23]
Rani F, Murray ML, Byrne PJ, et al. Epidemiologic features of antipsychotic prescribing to children and adolescents in primary care in the United Kingdom. Pediatrics 2008; 121(5): 1002–9
Risperdal (risperidone): prescribing information [online]. Available from URL: http://www.risperdal.com/sites/default/files/shared/pi/risperdal.pdf [Accessed 2011 Jan 9]
Zyprexa (olanzapine): prescribing information [online]. Available from URL: http://pi.lilly.com/us/zyprexa-pi.pdf [Accessed 2011 Jan 9]
Risperdal tablets, liquid and quicklet: summary of product characteristics [online]. Available from URL: http://www.medicines.org.uk/EMC/medicine/12818/SPC/Risperdal+Tablets%2c+Liquid+%26+Quicklet/#INDICATIONS [Accessed 2011 Jan 9]
Paediatric Formulary Committee. British national formulary for children 2009. BMJ Group, RPS Publishing, and RCPCH Publications Ltd, 2009
Cheng-Shannon J, McGough J, Pataki C, et al. Second-generation antipsychotic medications in children and adolescents. J Child Adolesc Psychopharmacol 2004; 14(3): 372–94
Armenteros JL, Davies M. Antipsychotics in early onset schizophrenia: systematic review and meta-analysis. Eur Child Adolesc Psych 2006; 15(3): 141–8
Lader M. Lethal complications of antipsychotic drug complication. Clin Risk 2006; 12(3): 113–7
Straus SMJM, Bleumink GS, Dieleman JP, et al. Antipsychotics and the risk of sudden cardiac death. Arch Intern Med 2004; 164: 1293–7
Rani FA, Byrne PJ, Murray ML, et al. Paediatric Atypical Antipsychotic Monitoring Safety (PAMS) study: pilot study in children and adolescents in secondary- and tertiarycare settings. Drug Saf 2009; 32(4): 325–33
Wood L, Martinez C. The general practice research database: role in pharmacovigilance. Drug Saf 2004; 27(12): 871–81
Wong IC, Murray ML. The potential of UK clinical databases in enhancing paediatric medication research. Br J Clin Pharmacol 2005; 59(6): 750–5
Medicines and Healthcare Products Regulatory Agency. The General Practice Research Database [online]. Available from URL: http://www.gprd.com [Accessed 2009 Aug 23]
Murray ML, de Vries CS, Wong ICK. A drug utilisation study of antidepressants in children and adolescents using the general practice research database. Arch Dis Child 2004; 89: 1098–102
Ackers R, Murray ML, Besag FMC, et al. Prioritising children’s medicines for research: a pharmacoepidemiological study on antiepileptic drugs. Br J Clin Pharmacol 2007; 63(6): 689–97
McCarthy S, Asherson P, Coghill D, et al. Attention-deficit hyperactivity disorder: treatment discontinuation in adolescents and young adults. Br J Psychiatry 2009; 194(3): 273–7
Thompson PL, Gilbert RE, Long PF, et al. Effect of antibiotics for otitis media on mastoiditis in children: a retrospective cohort study using the UK General Practice Research Database. Pediatrics 2009; 123(2): 424–30
Ackers R, Besag F, Hughes E, et al. Mortality rates and causes of death in children with epilepsy prescribed antiepileptic drugs: a retrospective cohort study using the UK General Practice Research Database. Drug Saf 2011; 34(5): 403–13
McCarthy S, Cranswick N, Potts L, et al. Mortality associated with attention-deficit hyperactivity disorder (ADHD) drug treatment: a retrospective cohort study of children, adolescents and young adults using the general practice research database. Drug Saf 2009; 32(11): 1089–96
Bland M. An introduction to medical statistics. Oxford: Oxford University Press, 1993
World Health Organization, Uppsala Monitoring Centre. The use of the WHO-UMC system for standardized case causality assessment [online]. Available from URL: http://who-umc.org/graphics/4409.pdf [Accessed 2011 Jun 1]
Baldessarini RJ, Tarazi FI. In: Hardman JG, Limbird LE, editors. Goodman s Gilman’s the pharmacological basis of therapeutics. 10th ed. New York (NY): McGraw-Hill Companies, 2001: 492
Clarkson A, Choonara I. Surveillance for fatal suspected adverse drug reactions in the UK. Arch Dis Child 2002; 87: 462–7
Vetter VL, Elia J, Erickson C, et al. Cardiovascular monitoring of children and adolescents with heart disease receiving medications for attention deficit/hyperactivity disorder: a scientific statement from the American Heart Association Council on cardiovascular disease in the Young Congenital Cardiac Defects Committee and the Council on Cardiovascular Nursing. Circulation 2008; 117: 2407–23
Ray WA, Meredith S, Thapa PB, et al. Antipsychotics and the risk of sudden cardiac death. Arch Gen Psychiat 2001; 58: 1161–7
Baldessarini RJ. Atypical antipsychotic drugs and the risk of sudden cardiac death. N Engl J Med 2009; 360(20): 2136–7
MHRA. Prescribing information for thioridazine [online]. Available from URL: http://www.mhra.gov.uk/home/idcplg?IdcService=GET_FILE·DocName=CON019553&RevisionSelectionMethod=LatestReleased [Accessed 2008 Jun 13]
Woods SW, Martin A, Spector SG, et al. Effects of development on olanzapine-associated adverse events. J Am Acad Child Adolesc 2002; 41(12): 1439–46
Allbeck P. Schizophrenia: a life-shortening disease. Schizophr Bull 1989; 15(1): 81–9
Osby U, Correia N, Brandt L, et al. Mortality and causes of death in schizophrenia in Stockholm County, Sweden. Schizophr Res 2000; 45: 21–8
Ruschena D, Mullen PE, Burgess P, et al. Sudden death in psychiatric patients. Br J Psychiatry 1998; 172: 331–6
Harris EC, Barraclough B. Excess mortality of mental disorder. Br J Psychiatry 1998; 176: 11–53
Acknowledgements
The authors would like to sincerely thank the GPRD verification team and staff at the ONS for providing the additional data for this study. We also thank all the GPs who contributed data to the GPRD, and those who contributed data to this study.
Funding: The license for the GPRD was funded by the European Commission via the Taskforce European Drug Development for the Young (TEDDY) network of Excellence European Commission Framework 6 Programme (2005–10). Professor Wong was supported by a Department of Health Public Health Career Scientist Award in England. Dr Rani was supported by a scholarship from the Ministry of Higher Education of Malaysia. The study was conducted independently from the above funding providers.
Contributors: Ian C.K. Wong, Fariz A. Rani and Macey L. Murray conceived the idea of the study. All authors were involved in the study design. Fariz A. Rani, Patrick Byrne, Noel Cranswick and Ian C.K. Wong analysed the data. All authors were involved in the interpretation of the data, had full access to the study data and take responsibility for the integrity of the data and accuracy of the data analysis. All authors drafted, revised and approved the final manuscript. Ian C.K. Wong is the guarantor.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rani, F.A., Byrne, P., Cranswick, N. et al. Mortality in Children and Adolescents Prescribed Antipsychotic Medication. Drug-Safety 34, 773–781 (2011). https://doi.org/10.2165/11591120-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11591120-000000000-00000