Abstract
Bone mass increases progressively during childhood, but mainly during adolescence when approximately 40% of total bone mass is accumulated. Peak bone mass is reached in late adolescence, and is a well recognised risk factor for osteoporosis later in life. Thus, increasing peak bone mass can prevent osteoporosis.
The critical interpretation of bone mass measurements is a crucial factor for the diagnosis of osteopenia/osteoporosis in children and adolescents. To date, there are insufficient data to formally define osteopenia/osteoporosis in this patient group, and the guidelines used for adult patients are not applicable. In males and females aged <20 years the terminology ‘low bone density for chronologic age’ may be used if the Z-score is less than −2. For children and adolescents, this terminology is more appropriate than osteopenia/osteoporosis. Moreover, the T-score should not be used in children and adolescents.
Many disorders, by various mechanisms, may affect the acquisition of bone mass during childhood and adolescence. Indeed, the number of disorders that have been identified as affecting bone mass in this age group is increasing as a consequence of the wide use of bone mass measurements. The increased survival of children and adolescents with chronic diseases or malignancies, as well as the use of some treatment regimens has resulted in an increase in the incidence of reduced bone mass in this age group.
Experience in treating the various disorders associated with osteoporosis in childhood is limited at present. The first approach to osteoporosis management in children and adolescents should be aimed at treating the underlying disease. The use of bisphosphonates in children and adolescents with osteoporosis is increasing and their positive effect in improving bone mineral density is encouraging. Osteoporosis prevention is a key factor and it should begin in childhood. Pediatricians should have a fundamental role in the prevention of osteoporosis, suggesting strategies to achieve an optimal peak bone mass.







Similar content being viewed by others
Notes
The use of trade names is for product identification purposes only and does not imply endorsement.
References
Leonard MB, Zemel BS. Current concepts in pediatric bone disease. Pediatr Clin North Am 2002; 49: 143–73
Heaney RP, Abrams S, Dawson-Hughes B, et al. Peak bone mass. Osteoporos Int 2000; 11: 985–1009
Lindsay R, Meunier PJ. Osteoporosis: review of the evidence for prevention, diagnosis and treatment and cost-effectiveness analysis. Osteoporos Int 1998; 8Suppl. 4: S1–88
Dent CE. Problems in metabolic bone disease. In: Frame B, Parfitt MA, Duncan H, editors. Clinical aspects of metabolic bone disease. Amsterdam: Exerpta Medica, 1973: 1–7
Brown JP, Josse RG, on behalf of Scientific Advisory Council of the Osteoporosis Society of Canada. 2002 clinical practice guidelines for the diagnosis and management of osteoporosis in Canada. CMAJ 2002; 167Suppl. 10: S1–34
Consensus development conference: diagnosis, prophylaxis and treatment of osteoporosis. Am J Med 1993; 94: 646–50
NIH Consensus Development Program. Osteoporosis prevention, diagnosis, and therapy: NIH consensus development conference statement 2000 [online]. Available from URL: http://www.consensus.nih.gov/cons/111/111_intro.htm [Accessed 2005 Oct 3]
Frost HM, Schonau E. The ‘muscle-bone unit’ in children and adolescents: a 2000 overview. J Pediatr Endocrinol Metab 2000; 13: 571–90
Faulkner KG. The tale of the T-score: review and perspective. Osteoporosis Int 2005; 16: 347–52
Cassidy JT. Osteopenia and osteoporosis in children. Clin Exp Rheumatol 1999; 17: 245–50
Chan YY, Bishop NJ. Clinical management of childhood osteoporosis. Int J Clin Pract 2002; 56: 280–6
Dumas R. Bases physiologiques: regulation du remodellage osseux. Arch Pédiatr 2002; 9Suppl. 2: 95–6
Saggese G, Baroncelli GI, Bertelloni S. Osteoporosis in children and adolescents: diagnosis, risk factors, and prevention. J Pediatr Endocrinol Metab 2001; 12: 833–59
Apkon SD. Osteoporosis in children who have disabilities. Phys Med Rehabil Clin N Am 2002; 13: 839–55
Kanis JA. Diagnosis of osteoporosis and assessment of fracture risk. Lancet 2002; 359: 1929–36
Goulding A, Jones IE, Taylor RW, et al. More broken bones: a 4-year double cohort study of young girls with and without distal forearm fractures. J Bone Miner Res 2000; 15: 2011–8
Ma D, Jones G. The association between bone mineral density, metacarpal morphometry, and upper limb fractures in children: a population-based case-control study. J Clin Endocrinol Metab 2003; 88: 1486–91
Gafni RI, McCarthy EF, Hatcher T, et al. Recovery from osteoporosis through skeletal growth: early bone mass acquisition has little effect on adult bone density. FASEB J 2002; 16: 736–8
Lewiecki EM, Watts NB, McClung MR, et al. Official positions of the International Society for Clinical Densitometry. J Clin Endocrinol Metab 2004; 89: 3651–5
The Writing Group for the ISCD Position Development Conference. Diagnosis of osteoporosis in men, premenopausal women, and children. J Clin Densitom 2004; 7: 17–26
Lewiecki EM, Kendler DL, Kiebzak GM, et al. Special report on the official positions of the International Society for Clinical Densitometry. Osteoporos Int 2004; 15: 779–84
Fewtrell MS, British Paediatric and Adolescent Bone Group. Bone densitometry in children assessed by dual x-ray absorptiometry: uses and pitfalls. Arch Dis Child 2003; 88: 795–8
Gafni RI, Baron J. Overdiagnosis of osteoporosis in children due to misinterpretation of dual-energy x-ray absorptiometry (DEXA). J Pediatr 2004; 144: 253–7
Schonau E. Problems of bone analysis in childhood and adolescence. Pediatr Nephrol 1998; 12: 420–9
Njeh FC, Fuerst T, Hans D, et al. Radiation exposure in bone mineral density assessment. Appl Radiat Isot 1999; 50: 215–36
Wang J, Thornton JC, Horlick M, et al. Dual x-ray absorptiometry in pediatric studies: changing scan modes alters bone and body composition measurements. J Clin Densitom 1999; 2: 135–41
Seeman E. Pathogenesis of bone fragility in women and men. Lancet 2002; 359: 1841–50
Baroncelli GI, Saggese G. Critical ages and stages of puberty in the accumulation of spinal and femoral bone mass: the validity of bone mass measurements. Horm Res 2000; 51Suppl. 1: 2–8
Soyka LA, Fairfield WP, Klibanski A. Hormonal determinants and disorders of peak bone mass in children. J Clin Endocrinol Metab 2000; 85: 3951–63
Katzman DK, Bachrach LK, Carter DR, et al. Clinical and anthropometric correlates of bone mineral acquisition in healthy adolescent girls. J Clin Endocrinol Metab 1991; 73: 1332–9
Carter DR, Bouxsein ML, Marcus R. New approaches for interpreting projected bone densitometry data. J Bone Miner Res 1992; 7: 137–45
Kroger H, Kotaniemi A, Kroger L, et al. Development of bone mass and bone density of the spine and femoral neck: a prospective study of 65 children and adolescents. Bone Miner 1993; 23: 171–82
Lu PW, Cowell CT, Lloyd-Jones SA, et al. Volumetric bone mineral density in normal subjects, aged 5–27 years. J Clin Endocrinol Metab 1996; 81: 1586–90
Baroncelli GI, Bertelloni S, Ceccarelli C, et al. Measurement of volumetric bone mineral density accurately determines degree of lumbar undermineralization in children with growth hormone deficiency. J Clin Endocrinol Metab 1998; 83: 3150–4
Peel NFA, Eastell R. Diagnostic value of estimated volumetric bone mineral density of the lumbar spine in osteoporosis. J Bone Miner Res 1994; 9: 317–20
Kroger H, Vainio P, Nieminen J, et al. Comparison of different models for interpreting bone mineral density measurements using DXA and MRI technology. Bone 1995; 17: 157–9
Van der Sluis IM, de Muinck Keizer-Schrama SMPF. Osteoporosis in childhood: bone density of children in health and disease. J Pediatr Endocrinol Metab 2001; 12: 817–32
Del Rio L, Carrascosa A, Pons F, et al. Bone mineral density of the lumbar spine in white Mediterranean Spanish children and adolescents: changes related to age, sex, and puberty. Pediatr Res 1994; 35: 362–6
Van der Sluis IM, de Ridder MAJ, Boot AM, et al. Reference data for bone density and body composition measured with dual energy x-ray absorptiometry in white children and young adults. Arch Dis Child 2002; 87: 341–7
Southard RN, Morris JD, Mahan JD, et al. Bone mass in healthy children: measurement with quantitative DXA. Radiology 1991; 179: 735–8
Bonjour J, Theintz G, Buchs B, et al. Critical years and stages of puberty for spinal and femoral bone mass accumulation during adolescence. J Clin Endocrinol Metab 1991; 73: 555–63
Henderson RC, Madsen CD. Bone density in children and adolescents with cystic fibrosis. J Pediatr 1996; 128: 28–34
Faulkner RA, Bailey DA, Drinkwater DT, et al. Bone densitometry in Canadian children 8–17 years of age. Calcif Tissue Int 1996; 59: 344–51
Fournier PE, Rizzoli R, Slosman DO, et al. Asynchrony between the rates of standing height gain and bone mass accumulation during puberty. Osteoporos Int 1997; 7: 525–32
Zanchetta JR, Plotkin H, Alvarez Filgueira ML. Bone mass in children: normative values for the 2–20 year-old population. Bone 1995; 16Suppl. 4: 393S–9S
Schonau E, Neu CM, Rauch F, et al. The development of bone strength at the proximal radius during childhood and adolescence. J Clin Endocrinol Metab 2001; 86: 613–8
Neu CM, Rauch F, Manz F, et al. Modeling of cross-sectional bone size, mass and geometry at the proximal radius: a study of normal bone development using peripheral quantitative computed tomography. Osteoporos Int 2001; 12: 538–47
Neu CM, Manz F, Rauch F, et al. Bone densities and bone size at the distal radius in healthy children and adolescents: a study using peripheral quantitative computed tomography. Bone 2001; 28: 227–32
Njeh CF, Boivin CM, Langton CM. The role of ultrasound in the assessment of osteoporosis: a review. Osteoporos Int 1997; 7: 7–22
Gonnelli S, Cepollaro C. The use of ultrasound in the assessment of bone status. J Endocrinol Invest 2002; 25: 389–97
Schonau E, Radermacher A, Wentzlik U, et al. The determination of ultrasound velocity in the os calcis, thumb and patella during childhood. Eur J Pediatr 1994; 153: 252–6
Van den Berg JPW, Noordam C, Ozyilmaz A, et al. Calcaneal ultrasound imaging in healthy children and adolescents: relation of the ultrasound parameters BUA and SOS to age, body weight, height, foot dimensions and pubertal stage. Osteoporos Int 2000; 11: 967–76
van den Bergh JP, Noordam C, Thijssen JM, et al. Measuring skeletal changes with calcaneal ultrasound imaging in healthy children and adults: the influence of size and location of the region of interest. Osteoporos Int 2001; 12: 970–9
Baroncelli GI, Federico G, Bertelloni S, et al. Bone quality assessment by quantitative ultrasound of proximal phalanxes of the hand in healthy subjects aged 3–21 years. Pediatr Res 2001; 49: 713–8
Barkmann R, Rohrschneider W, Vierling M, et al. German pediatric reference data for quantitative transverse transmission ultrasound of finger phalanges. Osteo-poros Int 2002; 13: 55–61
Vignolo M, Brignone A, Mascagni A, et al. Influence of age, sex, and growth variables on phalangeal quantitative ultrasound measures: a study in healthy children and adolescents. Calcif Tissue Int 2003; 72: 681–8
Lequin MH, van Rijn RR, Robben SGF, et al. Normal values for tibial quantitative ultrasonometry in Caucasian children and adolescents (aged 6 to 19 years). Calcif Tissue Int 2000; 67: 101–5
Jaworski M, Lebiedowski M, Lorenc RS, et al. Ultrasound bone measurement in pediatric subjects. Calcif Tissue Int 1995; 56: 368–71
Baroncelli GI, Federico G, Bertelloni S, et al. Assessment of bone quality by quantitative ultrasound of proximal phalanges of the hand and fracture rate in children and adolescents with bone and mineral disorders. Pediatr Res 2003; 54: 125–36
Leonard MB, Propert KJ, Zemel BS, et al. Discrepancies in pediatric bone mineral density reference data: potential for misdiagnosis of osteopenia. J Pediatr 1999; 135: 182–8
Khan AA, Brown JP, Kendler DL, et al. The 2002 Canadian bone densitometry recommendations: take-home messages. CMAJ 2002; 167: 1141–5
Taback SP. Osteoporosis in children: 2002 guidelines do not apply. CMAJ 2003; 168: 675–6
de Ridder CM, Delemarre-van de Waal HA. Clinical utility of markers of bone turnover in children and adolescents. Curr Opin Pediatr 1998; 10: 441–8
Saggese G, Baroncelli GI, Bertelloni S, et al. Twenty-four-hour osteocalcin, carboxyterminal propeptide of type I procollagen, and aminoterminal propeptide of type III procollagen rhythms in normal and growth-retarded children. Pediatr Res 1994; 35: 409–15
Szulc P, Seeman E, Delmas PD. Biochemical measurements of bone turnover in children and adolescents. Osteoporos Int 2000; 11: 281–94
Weaver CM, Peacock M, Martin BR, et al. Quantification of biochemical markers of bone turnover by kinetic measures of bone formation and resorption in young healthy females. J Bone Miner Res 1997; 12: 1714–20
Sillence DO, Senn A, Danks DM. Genetic heterogeneity in osteogenesis imperfecta. J Med Genet 1979; 16: 101–16
Roughley PJ, Rauch F, Glorieux FH. Osteogenesis imperfecta: clinical and molecular diversity. Eur Cell Mater 2003; 5: 41–7
Antoniazzi F, Mottes M, Fraschini P, et al. Osteogenesis imperfecta: practical treatment guidelines. Paediatr Drugs 2000; 2: 465–88
Rauch F, Travers R, Parfitt AM, et al. Static and dynamic bone histomorphometry in children with osteogenesis imperfecta. Bone 2000; 26: 581–9
Glorieux FH, Rauch F, Plotkin H, et al. Type V osteogenesis imperfecta: a new form of brittle bone disease. J Bone Miner Res 2000; 15: 1650–8
Glorieux FH, Ward LM, Rauch F, et al. Osteogenesis imperfecta type VI: a form of brittle bone disease with a mineralization defect. J Bone Miner Res 2002; 17: 30–8
Ward LM, Rauch F, Travers R, et al. Osteogenesis imperfecta type VII: an autosomal recessive form of brittle bone disease. Bone 2002; 31(1): 12–8
Labuda M, Morissette J, Ward LM, et al. Osteogenesis imperfecta type VII maps to the short arm of chromosome 3. Bone 2002; 31: 19–25
Orwoll ES, Klein RF. Osteoporosis in men. Endocr Rev 1995; 16: 87–116
Saggese G, Bertelloni S, Baroncelli GI. Sex steroids and the acquisition of bone mass. Horm Res 1997; 48Suppl. 5: 65–71
Orlic ZC, Raisz LG. Causes of secondary osteoporosis. J Clin Densitom 1998; 2: 79–92
Ross JL, Long LM, Feuillan P, et al. Normal bone density of the wrist and spine and increased wrist fractures in girls with Turner’s syndrome. J Clin Endocrinol Metab 1991; 73: 355–9
Davies MC, Gulekli B, Jacobs HS. Osteoporosis in Turner’s syndrome and other forms of primary amenorrhoea. Clin Endocrinol (Oxf) 1995; 43: 741–6
Gravholt CH, Juul S, Naeraa RW, et al. Morbidity in Turner syndrome. J Clin Epidemiol 1998; 51: 147–58
Landin-Wilhelmsen K, Bryman I, Windh M, et al. Osteoporosis and fractures in Turner syndrome: importance of growth promoting and oestrogen therapy. Clin Endocrinol (Oxf) 1999; 51: 497–502
Bakalov VK, Chen ML, Baron J, et al. Bone mineral density and fractures in Turner syndrome. Am J Med 2003; 115: 259–64
Bechtold S, Rauch F, Noelle V, et al. Musculoskeletal analyses of the forearm in young women with Turner syndrome: a study using peripheral quantitative computed tomography. J Clin Endocrinol Metab 2001; 86: 5819–23
Gravholt CH, Lauridsen AL, Brixen K, et al. Marked disproportionality in bone size and mineral, and distinct abnormalities in bone markers and calcitropic hormones in adult Turner syndrome: a cross-sectional study. J Clin Endocrinol Metab 2002; 87: 2798–808
Breuil V, Euller-Ziegler L. Gonadal dysgenesis and bone metabolism. J Bone Spine 2001; 68: 26–33
Luisetto G, Mastrogiacomo I, Bonanni G, et al. Bone mass and mineral metabolism in Klinefelter’s syndrome. Osteoporos Int 1995; 5: 455–61
Wong FHW, Pun KK, Wang C. Loss of bone mass in patients with Klinefelter’s syndrome despite sufficient testosterone replacement. Osteoporos Int 1993; 3: 3–7
Baptista F, Varela A, Sardinha LB. Bone mineral mass in males and females with and without Down syndrome. Osteoporos Int 2005; 16: 380–8
Lee PA, Witchel SF. The influence of estrogen on growth. Curr Opin Pediatr 1997; 9: 431–6
Marcus R. New perspectives on the skeletal role of estrogen. J Clin Endocrinol Metab 1998; 83: 2236–8
Riggs BL, Khosla S, Melton LJ. Sex steroids and the construction and conservation of adult skeleton. Endocr Rev 2002; 23: 279–302
Marcus R, Leary D, Schneider DL, et al. The contribution of testosterone to skeletal development and maintenance: lessons from the androgen insensitivity syndrome. J Clin Endocrinol Metab 2000; 85: 1032–7
Khosla S, Melton LJ, Riggs BL. Estrogen and the male skeleton. J Clin Endocrinol Metab 2002; 87: 1443–50
Cowell CT, Woodhead H, Brody J. Bone markers and bone mineral density during growth hormone treatment in children with growth hormone deficiency. Horm Res 2000; 54Suppl. 1: 44–51
Baroncelli GI, Bertelloni S, Ceccarelli C, et al. Dynamics of bone turnover in children with GH deficiency treated with GH until final height. Eur J Endocrinol 2000; 142: 549–56
Baroncelli GI, Bertelloni S, Sodini F, et al. Acquisition of bone mass in normal subjects and in patients with growth hormone deficiency. J Pediatr Endocrinol Metab 2003; 16: 327–35
Van der Sluis IM, Boot AM, Hop WC, et al. Long-term effects of growth hormone therapy on bone mineral density, body composition, and serum lipid levels in growth hormone deficient children: a 6-year follow-up study. Horm Res 2002; 58: 207–14
Kandemir N, Gonc EN, Yordam N. Responses of bone turnover markers and bone mineral density to growth hormone therapy in children with isolated growth hormone deficiency and multiple pituitary hormone deficiencies. J Pediatr Endocrinol Metab 2002; 15(6): 809–16
Baroncelli GI, Bertelloni S, Sodini F, et al. Lumbar bone mineral density at final height and prevalence of fractures in treated children with growth hormone deficiency. J Clin Endocrinol Metab 2002; 87: 3624–31
Faber J, Galloe AM. Changes in bone mass during prolonged subclinical hyperthy-roidism due to L-thyroxine treatment: a meta-analysis. Eur J Endocrinol 1994; 130: 350–6
Fitzpatrick LA. Secondary causes of osteoporosis. Mayo Clin Proc 2002; 77: 453–68
Cummings SR, Nevitt MC, Browner WS, et al. Risk factors for hip fracture in white women: study of Osteoporotic Fractures Research Group. N Engl J Med 1995; 332: 767–73
Saggese G, Bertelloni S, Baroncelli GI. Bone mineralization and calciotropic hormones in children with hyperthyroidism: effects of methimazole therapy. J Endocrinol Invest 1990; 13: 587–92
Mora S, Weber G, Marenzi K, et al. Longitudinal changes of bone density and bone resorption in hyperthyroid girls during treatment. J Bone Miner Res 1999; 14: 1971–7
Lucidarme N, Ruiz JC, Czernichow P, et al. Reduced bone mineral density at diagnosis and bone mineral recovery during treatment in children with Graves’ disease. J Pediatr 2000; 137: 56–62
Khosla S, Melton III LJ, Wermers RA, et al. Primary hyperparathyroidism and the risk of fracture: a population-based study. J Bone Miner Res 1999; 14: 1700–7
Damiani D, Aguiar CH, Crivellaro CE, et al. Pituitary macroadenoma and Cushing’s disease in pediatric patients: patient report and review of the literature. J Pediatr Endocrinol Metab 1998; 11: 665–9
Di Somma C, Pivonello R, Loche S, et al. Severe impairment of bone mass and turnover in Cushing’s disease: comparison between childhood-onset and adulthood-onset disease. Clin Endocrinol (Oxf) 2002; 56: 153–8
Duntas LH. Prolactinomas in children and adolescents: consequences in adult life. J Pediatr Endocrinol Metab 2001; 14Suppl. 5: 1227–32
Stiegler C, Leb G, Kleinert R, et al. Plasma levels of parathyroid hormone-related peptide are elevated in hyperprolactinemia and correlated to bone density status. J Bone Miner Res 1995; 10: 751–9
Pivonello R, Colao A, Di Somma C, et al. Impairment of bone status in patients with central diabetes insipidus. J Clin Endocrinol Metab 1998; 83: 2275–80
Pivonello R, Faggiano A, Di Somma C, et al. Effect of a short-term treatment with alendronate on bone density and bone markers in patients with central diabetes insipidus. J Clin Endocrinol Metab 1999; 84: 2349–52
Lala R, Matarazzo P, Bertelloni S, et al. Pamidronate treatment of bone fibrous dysplasia in nine children with McCune-Albright syndrome. Acta Paediatr 2000; 89: 188–93
Schonau E, Rauch F. Fibrous dysplasia. Horm Res 2002; 57Suppl. 2: 79–82
Chapurlat RD, Meunier PJ. Fibrous dysplasia of bone. Baillieres Best Pract Res Clin Rheumatol 2000; 14: 385–98
Fraser WD, Walsh CA, Birch MA, et al. Parathyroid hormone-related protein in the aetiology of fibrous dysplasia of bone in the McCune Albright syndrome. Clin Endocrinol (Oxf) 2000; 53: 621–8
Corsi A, Collins MT, Riminucci M, et al. Osteomalacic and hyperparathyroid changes in fibrous dysplasia of bone: core biopsy studies and clinical correlations. J Bone Miner Res 2003; 18: 1235–46
Terpstra L, Rauch F, Plotkin H, et al. Bone mineralization in polyostotic fibrous dysplasia: histomorphometric analysis. J Bone Miner Res 2002; 17: 1949–53
Hannon TS, Noonan K, Steinmetz R, et al. Is McCune-Albright syndrome overlooked in subjects with fibrous dysplasia of bone? J Pediatr 2003; 142: 532–8
Valerio G, del Puente A, Esposito-del Puente A, et al. The lumbar bone mineral density is affected by long-term poor metabolic control in adolescents with type 1 diabetes mellitus. Horm Res 2002; 58: 266–72
Heap J, Murray MA, Miller SC, et al. Alterations in bone characteristics associated with glycemic control in adolescents with type 1 diabetes mellitus. J Pediatr 2004; 144: 56–62
De Schepper J, Smitz J, Rosseneu S, et al. Lumbar spine bone mineral density in diabetic children with recent onset. Horm Res 1998; 50: 193–6
Pascual J, Argente J, Lopez MB, et al. Bone mineral density in children and adolescents with diabetes mellitus type 1 of recent onset. Calcif Tissue Int 1998; 62: 31–5
Mushtaq T, Ahmed SF. The impact of corticosteroids on growth and bone health. Arch Dis Child 2002; 87: 93–6
Ledford D, Apter A, Brenner AM, et al. Osteoporosis in the corticosteroid-treated patients with asthma. J Allergy Clin Immunol 1998; 102: 353–62
Van Staa TP, Leufkens HGM, Cooper C. The epidemiology of corticosteroid-induced osteoporosis: a meta-analysis. Osteoporos Int 2002; 13: 777–87
Canalis E, Pereira RC, Delany AM. Effects of glucocorticoids on the skeleton. J Pediatr Endocrinol Metab 2002; 15: 1341–5
Canalis E, Bilezikian JP, Angeli A, et al. Perspectives on glucocorticoid-induced osteoporosis. Bone 2004; 34: 593–8
van Staa TP, Bishop N, Leufkens HG, et al. Are inhaled corticosteroids associated with an increased risk of fracture in children? Osteoporos Int 2004; 15: 785–91
Kruse K. On the pathogenesis of anticonvulsant-drug-induced alterations of calcium metabolism. Eur J Pediatr 1982; 138: 202–5
Sheth RD, Wesolowski CA, Jacob JC, et al. Effect of carbamazepine and valproate on bone mineral density. J Pediatr 1995; 127: 256–62
Guo C-Y, Ronen GM, Atkinson SA. Long-term valproate and lamotrigine treatment may be a marker for reduced growth and bone mass in children with epilepsy. Epilepsia 2001; 42: 1141–7
Tsukahara H, Kimura K, Todoroki Y, et al. Bone mineral status in ambulatory pediatric patients on long-term anti-epileptic drug therapy. Pediatr Int 2002; 44: 247–53
Sheth RD. Bone health in pediatric epilepsy. Epilepsy Behav 2004; 5Suppl. 2: S30–5
Oner N, Kaya M, Karasalihoglu S, et al. Bone mineral metabolism changes in epileptic children receiving valproic acid. J Paediatr Child Health 2004; 40: 470–3
Ecevit C, Aydogan A, Kavakli T, et al. Effect of carbamazepine and valproate on bone mineral density. Pediatr Neurol 2004; 31: 279–82
Nishiyama S, Kuwahara T, Matsuda I. Decreased bone density in severely handicapped children and adults, with reference to the influence of limited mobility and anticonvulsant medication. Eur J Pediatr 1986; 144: 457–63
Van der Sluis IM, van den Heuvel-Eibrink MM, Hahlen K, et al. Altered bone mineral density and body composition, and increased fracture risk in childhood acute lymphoblastic leukemia. J Pediatr 2002; 141: 204–10
Arikoski P, Voutilainen R, Kroger H, et al. Bone mineral density in long-term survivors of childhood cancer. J Pediatr Endocrinol Metab 2003; 16: 343–53
Azcona C, Burghard E, Ruza E, et al. Reduced bone mineralization in adolescent survivors of malignant bone tumors: comparison of quantitative ultrasound and dual-energy x-ray absorptiometry. J Pediatr Hematol Oncol 2003; 25: 297–302
Ross DS. Monitoring L-thyroxine therapy: lessons from the effects of L-thyroxine on bone density. Am J Med 1991; 91: 1–4
Radetti G, Castellan C, Tato L, et al. Bone mineral density in children and adolescent females treated with high doses of L-thyroxine. Horm Res 1993; 39: 127–31
Kooh SW, Brnjac L, Ehrlich RM, et al. Bone mass in children with congenital hypothyroidism treated with thyroxine since birth. J Pediatr Endocrinol Metab 1996; 9: 59–62
Leger J, Ruiz JC, Guibourdenche J, et al. Bone mineral density and metabolism in children with congenital hypothyroidism after prolonged L-thyroxine therapy. Acta Paediatr 1997; 86: 704–10
Pitukcheewanont P, Safani D, Gilsanz V, et al. Quantitative computed tomography measurements of bone mineral density in prepubertal children with congenital hypothyroidism treated with L-thyroxine. J Pediatr Endocrinol Metab 2004; 17: 889–93
Tumer L, Hasanoglu A, Cinaz P, et al. Bone mineral density and metabolism in children treated with L-thyroxine. J Pediatr Endocrinol Metab 1999; 12: 519–23
Saggese G, Bertelloni S, Baroncelli GI, et al. Bone mineral density in adolescent females treated with L-thyroxine: a longitudinal study. Eur J Pediatr 1996; 155: 452–7
Verrotti A, Chiarelli F, Montanaro AF, et al. Bone mineral content in girls with precocious puberty treated with gonadotropin-releasing hormone analog. Gynecol Endocrinol 1995; 9: 277–81
Yanovski JA, Rose SR, Municchi G, et al. Treatment with a luteinizing hormone-releasing hormone agonist in adolescents with short stature. N Engl J Med 2003; 348: 908–17
Unal O, Berberoglu M, Evliyaoglu O, et al. Effects on bone mineral density of gonadotropin releasing hormone analogs used in the treatment of central precocious puberty. J Pediatr Endocrinol Metab 2003; 16: 407–11
Bertelloni S, Baroncelli GI, Sorrentino MC, et al. Effect of central precocious puberty and gonadotropin-releasing hormone analogue treatment on peak bone mass and final height in females. Eur J Pediatr 1998; 157: 363–7
Bertelloni S, Baroncelli GI, Ferdeghini M, et al. Final height, gonadal function and bone mineral density of adolescent males with central precocious puberty after therapy with gonadotropin-releasing hormone analogues. Eur J Pediatr 2000; 159: 369–74
Cromer B, Harel Z. Adolescents: at increased risk for osteoporosis? Clin Pediatr 2000; 39: 565–74
Paton NIJ, Macallan DC, Griffin GE, et al. Bone mineral density in patients with human immunodeficiency virus infection. Calcif Tissue Int 1997; 61: 30–2
Tebas P, Powderly WG, Claxton S, et al. Accelerated bone mineral loss in HIV-infected patients receiving potent antiretroviral therapy. AIDS 2000; 14: F63–7
Arpadi SM, Horlick M, Thornton J, et al. Bone mineral content is lower in prepubertal HIV-infected children. J Acquir Immune Defic Syndr 2002; 29: 450–4
Arpadi S, Horlick M, Shane E. Metabolic bone disease in human immunodeficiency virus-infected children. J Clin Endocrinol Metab 2004; 89: 21–3
Mora S, Zamproni I, Beccio S, et al. Longitudinal changes of bone mineral density and metabolism in antiretroviral-treated human immunodeficiency virus-infected children. J Clin Endocrinol Metab 2004; 89: 24–8
Zamboni G, Antoniazzi F, Bertoldo F, et al. Altered bone metabolism in children infected with human immunodeficiency virus. Acta Paediatr 2003; 92: 12–6
Goodman WG, Leite Duarte ME. Aluminum: effects on bone and role in the pathogenesis of renal osteodystrophy. Miner Electrolyte Metab 1991; 17: 221–32
Frame B, Jackson CE, Reynolds WA, et al. Hypercalcemia and skeletal effects in chronic hypervitaminosis A. Ann Intern Med 1974; 1: 44–8
Ruby LK, Mital MA. Skeletal deformities following chronic hypervitaminosis A. J Bone Joint Surg Am 1974; 56(6): 1283–7
Cointin M, Sommelet-Olive D, Cuny JF, et al. Complications osseuses de l’intoxication chronique par l’étrétinate chez l’enfant [English abstract available]. Ann Pediatr 1990; 37: 458–60
Mascarenhas MR, Tershakovec AM, Stettler N. Nutrition interventions in childhood for the prevention of chronic diseases in adulthood. Curr Opin Pediatr 1999; 11: 598–604
Weaver CM, Peacock M, Johnston CC. Adolescent nutrition in the prevention of postmenopausal osteoporosis. J Clin Endocrinol Metab 1999; 84: 1839–43
Sarazin M, Alexandre C, Thomas T. Influence on bone metabolism of dietary trace elements, protein, fat, carbohydrates, and vitamins. Joint Bone Spine 2000; 67: 408–18
Quint EH, Harel Z. Osteoporosis in teenagers. J Pediatr Adolesc Gynecol 2002; 15: 241–3
Bonjour JP, Ammann P, Chevalley T, et al. Protein intake and bone growth. Can J Appl Physiol 2001; 26 Suppl.: S153–66
Bell NH. Bone loss and gastric bypass surgery for morbid obesity. J Clin Endocrinol Metab 2004; 89: 1059–60
Coates PS, Fernstrom JD, Fernstrom MH, et al. Gastric bypass surgery for morbid obesity leads to an increase in bone turnover and a decrease in bone mass. J Clin Endocrinol Metab 2004; 89: 1061–5
Rude RK, Olerich M. Magnesium deficiency: possible role in osteoporosis associated gluten-sensitive enteropathy. Osteoporos Int 1996; 6: 453–61
Molteni N, Caraceni MP, Bardella MT, et al. Bone mineral density in adult celiac patients and the effect of gluten-free diet from childhood. Am J Gastroenterol 1990; 85: 51–3
Walters JR, Banks LM, Butcher GP, et al. Detection of low bone mineral density by dual energy x-ray absorptiometry in unsuspected suboptimally treated coeliac disease. Gut 1995; 37: 220–4
Corazza GR, Di Sario A, Cecchetti L, et al. Influence of pattern of clinical presentation and of gluten-free diet on bone mass and metabolism in adult coeliac disease. Bone 1996; 18: 525–30
Stenson WF, Newberry R, Lorenz R, et al. Increased prevalence of celiac disease and need for routine screening among patients with osteoporosis. Arch Intern Med 2005; 165: 393–9
Mora S, Weber G, Barera G, et al. Effect of gluten-free diet on bone mineral content in growing patients with celiac disease. Am J Clin Nutr 1993; 57: 224–8
Mora S, Barera G, Ricotti A, et al. Reversal of low bone density with a gluten-free diet in children and adolescents with celiac disease. Am J Clin Nutr 1998; 67: 477–81
Kavak US, Yuce A, Kocak N, et al. Bone mineral density in children with untreated and treated celiac disease. J Pediatr Gastroenterol Nutr 2003; 37: 434–6
Hartman C, Hino B, Lerner A, et al. Bone quantitative ultrasound and bone mineral density in children with celiac disease. J Pediatr Gastroenterol Nutr 2004; 39: 504–10
Barera G, Beccio S, Proverbio MC, et al. Consumption of a gluten-free diet. Am J Clin Nutr 2004; 79: 148–54
Cellier C, Flobert C, Cormier C, et al. Severe osteopenia in symptom-free adults with a childhood diagnosis of coeliac disease [letter]. Lancet 2000; 355: 806
Mora S, Barera G, Beccio S, et al. Bone density and bone metabolism are normal after long-term gluten-free diet in young celiac patients. Am J Gastroenterol 1999; 94: 398–403
Tucker KL. Does milk intake in childhood protect against later osteoporosis? Am J Clin Nutr 2003; 77: 10–1
Sandler RB, Slemenda CW, LaPorte RE, et al. Postmenopausal bone density and milk consumption in childhood and adolescence. Am J Clin Nutr 1985; 42: 270–4
Kalkwarf HJ, Khoury JC, Lanphear BP. Milk intake during childhood and adolescence, adult bone density, and osteoporotic fractures in US women. Am J Clin Nutr 2003; 77: 257–65
Saggese G, Baroncelli GI. Nutritional aspects of calcium and vitamin D from infancy to adolescence. Ann Ist Super Sanità 1995; 31: 461–79
Infante D, Tormo R. Risk of inadequate bone mineralization in diseases involving long-term suppression of dairy products. J Pediatr Gastroenterol Nutr 2000; 30: 310–3
Chan GM, Hess M, Hollis J, et al. Bone mineral status in childhood accidental fractures. Am J Dis Child 1984; 138: 569–70
Goulding A, Cannan R, Williams SM, et al. Bone mineral density in girls with forearm fractures. J Bone Miner Res 1998; 13: 143–8
American Academy of Pediatrics, Committee on Nutrition. Calcium requirements of infants, children, and adolescents. Pediatrics 1999; 104: 1152–7
Bonjour JP, Chevalley T, Ammann P, et al. Gain in bone mineral mass in prepubertal girls 3.5 years after discontinuation of calcium supplementation: a follow-up study. Lancet 2001; 358: 1208–12
Holick MF. Vitamin D: a millenium perspective. J Cell Biochem 2003; 88: 296–307
Baroncelli GI, Bertelloni S, Ceccarelli C, et al. Bone turnover in children with vitamin D deficiency rickets before and during treatment. Acta Paediatr 2000; 89: 513–8
Holick MF. Sunlight ‘D’ilemma: risk of cancer or bone disease and muscle weakness. Lancet 2001; 357: 4–5
Zamora SA, Rizzoli R, Belli DC, et al. Vitamin D supplementation during infancy is associated with higher bone mineral mass in prepubertal girls. J Clin Endocrinol Metab 1999; 84: 4541–4
Hochberg Z, Bereket A, Davenport M, et al. Consensus development for the supplementation of vitamin D in childhood and adolescence. Horm Res 2002; 58: 39–51
Saggese G, Bertelloni S, Baroncelli GI, et al. Mineral homeostasis in osteoporosis of anorexia nervosa. Minerva Pediatr 1989; 41: 61–5
Bachrach LK, Katzman DK, Litt IF, et al. Recovery from osteopenia in adolescent girls with anorexia nervosa. J Clin Endocrinol Metab 1991; 72: 602–6
Biller BM, Saxe V, Herzog DB, et al. Mechanisms of osteoporosis in adult and adolescent women with anorexia nervosa. J Clin Endocrinol Metab 1989; 68: 548–54
Soyka LA, Grinspoon S, Levitsky LL, et al. The effects of anorexia nervosa on bone metabolism in female adolescents. J Clin Endocrinol Metab 1999; 84: 4489–96
Misra M, Miller KK, Bjornson J, et al. Alterations in growth hormone secretory dynamics in adolescent girls with anorexia nervosa and effects on bone metabolism. J Clin Endocrinol Metab 2003; 88: 5615–23
Audi L, Vargas DM, Gussinyé M, et al. Clinical and biochemical determinants of bone metabolism and bone mass in adolescent female patients with anorexia nervosa. Pediatr Res 2002; 51: 497–504
Soyka LA, Misra M, Frenchman A, et al. Abnormal bone mineral accrual in adolescent girls with anorexia nervosa. J Clin Endocrinol Metab 2002; 87: 4177–85
Seeman E, Karlsson MK, Duan Y. On exposure to anorexia nervosa, the temporal variation in axial and appendicular skeletal development predisposes to site-specific deficits in bone size and density: a cross-sectional study. J Bone Miner Res 2000; 15: 2259–65
Vermeer C, Gijsbers BL, Cracium AM, et al. Effects of vitamin K on bone mass and bone metabolism. J Nutr 1996; 126: 1187S
Wyshak G, Frisch RE. Carbonated beverages, dietary calcium, the dietary calcium/phosphorus ratio, and bone fractures in girls and boys. J Adolesc Health 1994; 15: 210–5
Petridou E, Karpathios T, Dessypris N, et al. The role of dairy products and nonalcoholic beverages in bone fractures among schoolage children. Scand J Soc Med 1997; 25: 119–25
Wyshak G. Teenaged girls, carbonated beverages consumption, and bone fractures. Arch Pediatr Adolesc Med 2000; 154: 610–3
Kinney MAO. Does consumption of cola beverages cause bone fractures in children? Mayo Clin Proc 2002; 77: 1005–6
Whiting SJ, Healey A, Psiuk S, et al. Relationship between carbonated and other low nutrient dense beverages and bone mineral content of adolescence. Nutr Res 2001; 21: 1107–15
McGartland C, Robson PJ, Murray L, et al. Carbonated soft drink consumption and bone mineral density in adolescence: the Northern Ireland Young Hearts Project. J Bone Miner Res 2003; 18: 1563–9
Mazariegos-Ramos E, Guerrero-Romero F, Rodriguez-Moran M, et al. Consumption of soft drinks with phosphoric acid as a risk factor for the development of hypocalcemia in children: a case-control study. J Pediatr 1995; 126: 940–2
Harnack L, Stang J, Story M. Soft drink consumption among US children and adolescents: nutritional consequences. J Am Diet Assoc 1999; 99: 436–41
Fitzpatrick L, Heaney RP. Got soda? J Bone Miner Res 2003; 18: 1570–2
Cavadini C, Siega-Riz AM, Popkin BM. US adolescent food intake trends from 1965 to 1996. Arch Dis Child 2000; 83: 18–24
American Academy of Pediatrics Committee on School Health. Soft drinks in schools. Pediatrics 2004; 113: 152–4
Moukarzel A. Metabolic bone disease in total parenteral nutrition. In: Lifshitz F, editor. Pediatric endocrinology. 3rd ed. New York: Marcel Dekker, 1996: 535–45
Buchman AL, Moukarzel A. Metabolic bone disease associated with total parenteral nutrition. Clin Nutr 2000; 19: 217–31
Bishop NJ, Dahlenburg SL, Fewtrell MS, et al. Early diet of preterm infants and bone mineralization at age five years. Acta Paediatr 1996; 85: 230–6
Miller ME. The bone disease of preterm birth: a biomechanical perspective. Pediatr Res 2003; 52: 1–6
Fewtrell MS, Prentice A, Jones SC, et al. Bone mineralization and turnover in preterm infants at 8–12 years of age: the effect of early diet. J Bone Miner Res 1999; 14: 810–20
Cooper C, Javaid MK, Taylor P, et al. The fetal origins of osteoporotic fracture. Calcif Tissue Int 2002; 70: 391–4
Jones G, Dwyer T. Birth weight, birth length, and bone density in prepubertal children: evidence for an association that may be mediated by genetic factors. Calcif Tissue Int 2000; 67: 304–8
Zamora SA, Belli DC, Rizzoli R, et al. Lower femoral neck bone mineral density in prepubertal former preterm infants. Bone 2001; 29: 424–7
Daci E, van Cromphaut S, Bouillon R. Mechanisms influencing bone metabolism in chronic illness. Horm Res 2002; 58Suppl. 1: 44–51
McDonagh JE. Osteoporosis in juvenile idiopathic arthritis. Curr Opin Rheumatol 2001; 13: 399–404
Cimaz R. Osteoporosis in childhood rheumatic diseases: prevention and therapy. Best Pract Res Clin Rheumatol 2002; 16: 397–409
Rabinovich CE. Bone metabolism in childhood rheumatic disease. Rheum Dis Clin N Am 2002; 28: 655–67
Alsufyani KA, Ortiz-Alvarez O, Cabral DA, et al. Bone mineral density in children and adolescents with systemic lupus erythematosus, juvenile dermatomyositis, and systemic vasculitis: relationship to disease duration, cumulative corticosteroid dose, calcium intake, and exercise. J Rheumatol 2005; 32: 729–33
Lien G, Selvaag AM, Flato B, et al. A two-year prospective controlled study of bone mass and bone turnover in children with early juvenile idiopathic arthritis. Arthritis Rheum 2005; 52: 833–40
Goodman WG, Coburn JW, Slatopolsky E, et al. Renal osteodystrophy in adults and children. In: Favus MJ, editor. Primer on the metabolic bone diseases and disorders of mineral metabolism. 4th ed. Philadelphia (PA): Lippincott Williams & Wilkins, 1999: 347–63
Matteini M, Cotrozzi G. Bicarbonate renal diabetes (proximal or type II renal tubular acidosis) as a cause of marked hypercalciuria, nephrolithiasis, osteoporotic rickets and delayed somatogenital and skeletal development. Minerva Pediatr 1973; 25: 1215–8
Freundlich M, Alonzo E, Bellorin-Font E, et al. Reduced bone mass in children with idiopathic hypercalciuria and in their asymptomatic mothers. Nephrol Dial Transplant 2002; 17: 1396–401
Penido MG, Lima EM, Marino VS, et al. Bone alterations in children with idiopathic hypercalciuria at the time of diagnosis. Pediatr Nephrol 2003; 18: 133–9
Polito C, Iolascon G, Nappi B, et al. Growth and bone mineral density in long-lasting idiopathic hypercalciuria. Pediatr Neprhol 2003; 18: 545–7
Skalova S, Palicka V, Kutilek S. Bone mineral density and urinary N-acetyl-beta-D-glucosaminidase activity in paediatric patients with idiopathic hypercalciuria. Nephrology 2005; 10: 99–102
Issenman RM, Atkinson SA, Radoja C, et al. Longitudinal assessment of growth, mineral metabolism, and bone mass in pediatric Crohn’s disease. J Pediatr Gastroenterol Nutr 1993; 17: 401–6
Cowan FJ, Warner JT, Dunstan FD, et al. Inflammatory bowel disease and predisposition to osteopenia. Arch Dis Child 1997; 76: 325–9
Boot AM, Bouquet J, Krenning EP, et al. Bone mineral density and nutritional status in children with chronic inflammatory bowel disease. Gut 1998; 42: 188–94
Semeao EJ, Jawad AF, Stouffer NO, et al. Risk factors for low bone mineral density in children and young adults with Crohn’s disease. J Pediatr 1999; 135: 593–600
Gupta A, Paski S, Issenman R, et al. Lumbar spine bone mineral density at diagnosis and during follow-up in children with IBD. J Clin Densitom 2004; 7: 290–5
Burnham JM, Shults J, Semeao E, et al. Whole body BMC in pediatric Crohn disease: independent effects of altered growth, maturation, and body composition. J Bone Miner Res 2004; 19: 1961–8
Harpavat M, Greenspan SL, O’Brien C, et al. Altered bone mass in children at diagnosis of Crohn disease: a pilot study. J Pediatr Gastroenterol Nutr 2005; 40: 295–300
Mendeloff AI, Calkins BM. The epidemiology of idiopathic inflammatory bowel disease. In: Kirsner JB, Shorter RG, editors. Inflammatory bowel disease. Philadelphia (PA): Lea and Febiger, 1988: 3–34
Bernstein CN, Blanchard JF, Leslie W, et al. The incidence of fracture among patients with inflammatory bowel disease: a population-based cohort study. Ann Intern Med 2000; 133: 795–9
Klaus J, Armbrecht G, Steinkamp M, et al. High prevalence of osteoporotic vertebral fractures in patients with Crohn’s disease. Gut 2002; 51: 654–8
Loftus EV, Crowson CS, Sandborn WJ, et al. Long-term fracture risk in patients with Crohn’s disease: a population-based study in Olmsted County, Minnesota. Gastroenterology 2002; 123: 468–75
Kobayashi A, Kawai S, Utsunomiya T, et al. Bone disease in infants and children with hepatobiliary disease. Arch Dis Child 1974; 49: 641–6
Heubi JE, Hollis BW, Specker B, et al. Bone disease in chronic childhood cholestasis: I. Vitamin D absorption and metabolism. Hepatology 1989; 9: 258–64
Tokita A, Nittono H, Mori T, et al. Vitamin D metabolism in pre-operative extrahepatic biliary atresia. Acta Paediatr Scand 1991; 80: 634–9
Argao EA, Specker BL, Heubi JE. Bone mineral content in infants and children with chronic cholestatic liver disease. Pediatrics 1993; 91: 1151–4
Almdal T, Schaadt O, Vesterdad Jorgensen J, et al. Vitamin D, parathyroid hormone, and bone mineral content of lumbar spine and femur in primary biliary cirrhosis. J Intern Med 1989; 225: 207–13
Isaia G, Di Stefano M, Roggia C, et al. Bone disorders in cholestatic liver diseases. Forum 1998; 8: 28–38
Floreani A, Fries W, Luisetto G, et al. Bone metabolism in orthotopic liver transplantation: a prospective study. Liver Transpl Surg 1998; 4: 311–9
Trautwein C, Possienke M, Schlitt HJ, et al. Bone density and metabolism in patients with viral hepatitis and cholestatic liver diseases before and after liver transplantation. Am J Gastroenterol 2000; 95: 2343–51
Newton J, Francis R, Prince M, et al. Osteoporosis in primary biliary cirrhosis revisited. Gut 2001; 49: 282–7
Chongsrisawat V, Ruttanamongkol P, Chaiwatanarat T, et al. Bone density and 25-hydroxyvitamin D level in extrahepatic biliary atresia. Pediatr Surg Int 2001; 17: 604–8
Argao EA, Heubi JE, Hollis BW, et al. D-Alpha-tocopheryl polyethylene glycol-1000 succinate enhances the absorption of vitamin D in chronic cholestatic liver disease of infancy and childhood. Pediatr Res 1992; 31: 146–50
Hodgson SF, Dickson ER, Wahner HW, et al. Bone loss and reduced osteoblast function in primary biliary cirrhosis. Ann Intern Med 1985; 103: 855–60
Sylvester FA. Bone abnormalities in gastrointestinal and hepatic disease. Rev Endocr Metab Disord 2001; 2: 75–80
Heubi JE, Higgins JV, Argao EA, et al. The role of magnesium in the pathogenesis of bone disease in childhood cholestatic liver disease: a preliminary report. J Pediatr Gastroenterol Nutr 1997; 25: 301–6
Shane E, Mancini D, Aaronson K, et al. Bone mass, vitamin D deficiency, and hyperparathyroidism in congestive heart failure. Am J Med 1997; 103: 197–207
Rego C, Guerra A, Guardiano M, et al. Bony density in adolescents after surgical repair of tetralogy of Fallot: a comparative study with healthy adolescents. Cardiol Young 2002; 12: 531–6
De Sanctis V, Pinamonti A, Di Palma A, et al. Growth and development in thalassaemia major patients with severe bone lesions due to desferrioxamine. Eur J Paediatr 1996; 155: 368–72
Benigno V, Bertelloni S, Baroncelli GI, et al. Effects of thalassemia major on bone mineral density in late adolescence. J Pediatr Endocrinol Metab 2003; 16Suppl. 2: 337–42
Mahachoklertwattana P, Chuansumrit A, Sirisriro R, et al. Bone mineral density, biochemical and hormonal profiles in suboptimally treated children and adolescents with β-thalassemia disease. Clin Endocrinol (Oxf) 2003; 58: 273–9
Domrongkitchaiporn S, Sirikulchayanonta V, Angchaisuksiri P, et al. Abnormalities in bone mineral density and bone histology in thalassemia. J Bone Miner Res 2003; 18: 1682–8
Hershkovitz I, Rothschild BM, Latimer B, et al. Recognition of sickle cell anemia in skeletal remains of children. Am J Phys Anthropol 1997; 104: 213–26
Gallacher SJ, Deighan C, Wallace AM, et al. Association of severe haemophilia A with osteoporosis: a densitometric and biochemical study. Q J Med 1994; 87: 181–6
Barnes C, Wong P, Egan B, et al. Reduced bone density among children with severe hemophilia. Pediatrics 2004; 114: e177–81
Yakisan E, Schirg E, Zeidler C, et al. High incidence of significant bone loss in patients with severe congenital neutropenia (Kostmann’s syndrome). J Pediatr 1997; 131: 592–7
Zeidler C, Welte K. Kostmann syndrome and severe congenital neutropenia. Semin Hematol 2002; 39: 82–8
Elhasid R, Hofbauer LC, Ish-Shalom S, et al. Familial severe congenital neutropenia associated with infantile osteoporosis: a new entity. Am J Hematol 2003; 72: 34–7
Dale DC, Cottle TE, Fier CJ, et al. Severe chronic neutropenia: treatment and follow-up of patients in the Severe Chronic Neutropenia International Registry. Am J Hematol 2003; 72: 82–93
Leung DY, Geha RS. Clinical and immunologic aspects of the hyperimmunoglobulin E syndrome. Hematol Oncol Clin North Am 1988; 2: 81–100
Kilic SS, Sanal O, Tezcan I, et al. Osteochondritis dissecans in a patient with hyperimmunoglobulin E syndrome. Turk J Pediatr 2002; 44: 357–9
Chamlin SL, McCalmont TH, Cunningham BB, et al. Cutaneous manifestations of hyper-IgE syndrome in infants and children. J Pediatr 2002; 141: 572–5
Kaste SC, Chesney RW, Hudson MM, et al. Bone mineral status during and after therapy of childhood cancer: an increasing population with multiple risk factors for impaired bone health. J Bone Miner Res 1999; 14: 2010–4
Hesseling PB, Hough SF, Nel ED, et al. Bone mineral density in long-term survivors of childhood cancer. Int J Cancer 1998; 11 Suppl.: 44–7
Vassilopoulou-Sellin R, Brosnan P, Delpassand A, et al. Osteopenia in young adult survivors of childhood cancer. Med Pediatr Oncol 1999; 32: 272–8
Zerwech JE, Ruml LA, Gottschalk F, et al. The effects of twelve weeks of bed rest on bone histology, biochemical markers of bone turnover, and calcium homeostasis in eleven normal subjects. J Bone Miner Res 1998; 13: 1594–601
Donaldson CL, Hulley SB, Vogel JM, et al. Effect of prolonged bed rest on bone mineral. Metabolism 1970; 19: 1071–84
Holick MF. Perspective on the impact of weightlessness on calcium and bone metabolism. Bone 1998; 22 Suppl.: 105S–11S
Shaw NJ, White CP, Fraser WD, et al. Osteopenia in cerebral palsy. Arch Dis Child 1994; 71: 235–8
Wilmshurst S, Ward K, Adams JE, et al. Mobility status and bone density in cerebral palsy. Arch Dis Child 1996; 75: 164–5
Dauty M, Perrouin Verbe B, Maugars Y, et al. Supralesional and sublesional bone mineral density in spinal cord-injured patients. Bone 2000; 27: 305–9
Henderson RC, Lark RK, Gurka MJ, et al. Bone density and metabolism in children and adolescents with moderate to severe cerebral palsy. Pediatrics 2002; 110: 1–10
King W, Levin R, Schmidt R, et al. Prevalence of reduced bone mass in children and adults with spastic quadriplegia. Dev Med Child Neurol 2003; 45: 12–6
Quan A, Adams R, Ekmark E, et al. Bone mineral density in children with myelomeningocele: effect of hydrochlorothiazide. Pediatr Nephrol 2003; 18: 929–33
Larson CM, Henderson RC. Bone mineral density and fractures in boys with Duchenne muscular dystrophy. J Pediatr Orthop 2000; 20: 71–4
Aparicio LF, Jurkovic M, DeLullo J. Decreased bone density in ambulatory patients with Duchenne muscular dystrophy. J Pediatr Orthop 2002; 22: 179–81
Bianchi ML, Mazzanti A, Galbiati E, et al. Bone mineral density and bone metabolism in Duchenne muscular dystrophy. Osteoporos Int 2003; 14: 761–7
Cizza G, Ravn P, Chrousos GP, et al. Depression: a major, unrecognized risk factor for osteoporosis? Trends Endocrinol Metab 2001; 12: 198–203
Vrkljan M, Thaller V, Lovricevic I, et al. Depressive disorder as possible risk factor of osteoporosis. Coll Anthropol 2001; 25: 485–92
Lyles KW. Osteoporosis and depression: shedding more light upon a complex relationship. J Am Geriatr Soc 2001; 49: 827–8
Irwin CE, Shafer M-A, Ryan SA. The adolescent patient. In: Rudoph AM, Hoffman JIE, Rudolph CD, editors. Rudolph’s Pediatrics. London: Prentice Hall Int., 1996: 42–3
Klein L, Herndon DN, Langman CB, et al. Long-term reduction in bone mass after severe burn injury in children. J Pediatr 1995; 126: 252–6
Berger MM, Rothen C, Cavadini C, et al. Exudative mineral losses after serious burns: a clue to the alterations of magnesium and phosphate metabolism. Am J Clin Nutr 1997; 65: 1473–81
Klein L, Langman CB, Herndon DN. Vitamin D depletion following burn injury in children: a possible factor in post-burn osteopenia. J Trauma 2002; 52: 346–50
Klein GL, Chen TC, Holick MF, et al. Synthesis of vitamin D in skin after burns. Lancet 2004; 363: 291–2
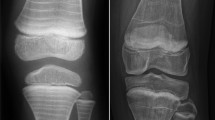
Jergas MD, Genant HK. Radiology of osteoporosis. In: Favus MJ, editor. Primer on the metabolic bone diseases and disorders of mineral metabolism. 4th ed. Philadelphia (PA): Lippincott Williams & Wilkins, 1999: 160–9
Herbold NH, Frates SE. Update of nutrition guidelines for the teen: trends and concerns. Curr Opin Pediatr 2000; 12: 303–9
Bachrach LK. Making an impact on pediatric bone health. J Pediatr 2000; 136: 137–9
American College of Sport Medicine. The female athlete triad. Med Sci Sports Exerc 1997; 229: 1–9
American Psychiatric Association. Practice guidelines for the treatment of patients with eating disorders. Am J Phychiatry 2000; 157Suppl. 1: 1–36
Rodino MA, Shane E. Osteoporosis after organ transplantation. Am J Med 1998; 104: 459–69
Cohen A, Shane E. Osteoporosis after solid organ and bone marrow transplantation. Osteoporos Int 2003; 14: 617–30
Daniels MW, Wilson DM, Paguntalan HG, et al. Bone mineral density in pediatric transplant recipients. Transplantation 2003; 76: 673–8
Acott PD, Crocker JF, Wong JA, et al. Decreased bone mineral density in the pediatric renal transplant population. Pediatr Transplant 2003; 7: 358–63
Schulte C, Beelen DW, Schaefer UW, et al. Bone loss in long-term survivors after transplantation of hematopoietic stem cells: a prospective study. Osteoporos Int 2000; 11: 344–53
Giannini S, Nobile M, Ciuffreda M, et al. Long-term persistence of low bone density in orthotopic liver transplantation. Osteoporos Int 2000; 11: 417–24
Segal E, Baruch Y, Kramsky R, et al. Predominant factors associated with bone loss in liver transplant patients after prolonged post-transplantation period. Clin Transplant 2003; 17: 13–9
Nysom K, Holm K, Michaelsen KF, et al. Bone mass after allogeneic BMT for childhood leukaemia or lymphoma. Bone Marrow Transplant 2000; 25: 191–6
Cook SD, Harding AF, Morgan EL, et al. Trabecular bone mineral density in idiopathic scoliosis. J Pediatr Orthop 1987; 7: 168–74
Thomas KA, Cook SD, Skalley TC, et al. Lumbar spine and femoral neck bone mineral density in idiopathic scoliosis: a follow-up study. J Pediatr Orthop 1992; 12: 235–40
Cheng JC, Qin L, Cheung CS, et al. Generalized low areal and volumetric bone mineral density in adolescent idiopathic scoliosis. J Bone Miner Res 2000; 15: 1587–95
Cheng JC, Tang SP, Guo X, et al. Osteopenia in adolescent idiopathic scoliosis: a histomorphometric study. Spine 2001; 26: E19–23
Castells S. Metabolic bone disease. In: Lifshitz F, editor. Pediatric endocrinology. 3rd ed. New York: Marcel Dekker, 1996: 521–34
Moen C. Orthopedic aspects of progeria. J Bone Joint Surg Am 1982; 64: 542–6
De Paula Rodrigues GH, das Eiras Tamega I, Duque G, et al. Severe bone changes in a case of Hutchinson-Gilford syndrome. Ann Genet 2002; 45: 151–5
Uitto J. Searching for clues to premature aging. Trends Endocrinol Metab 2002; 13: 140–1
Maayan C, Bar-On E, Foldes AJ, et al. Bone mineral density and metabolism in familial dysautonomia. Osteoporos Int 2002; 13: 429–33
Haas RH, Dixon SD, Sartoris D, et al. Osteopenia in Rett syndrome. J Pediatr 1997; 13: 771–4
Leonard H, Thomson MR, Glasson EJ, et al. A population based approach to the investigation of osteopenia in Rett syndrome. J Dev Med Child Neurol 1999; 41: 323–8
Cepollaro C, Gonnelli S, Bruni D, et al. Dual x-ray absorptiometry and bone ultrasonography in patients with Rett syndrome. Calcif Tissue Int 2001; 69: 259–62
Budden SS, Gunness ME. Bone histomorphometry in three females with Rett syndrome. Brain Dev 2001; 23: S133–57
Julu POO, Kerr AM, Hansen S, et al. Functional evidence of brain stem immaturity in Rett syndrome. Eur Child Adolesc Psychiatry 1997; 6Suppl. 1: 47–54
Illes T, Halmai V, de Jonge T, et al. Decreased bone mineral density in neurofibro-matosis-1 patients with spinal deformities. Osteoporos Int 2001; 12: 823–7
Kuorilehto T, Poyhonen M, Bloigu R, et al. Decreased bone mineral density and content in neurofibromatosis type 1: lowest local values are located in the load-carrying parts of the body. Osteoporos Int. In press
Abes M, Sarihan H, Madenci E. Evaluation of bone mineral density with dual x-ray absorptiometry for osteoporosis in children with bladder augmentation. J Pediatr Surg 2003; 38: 230–2
Mingin G, Maroni P, Gerharz EW, et al. Linear growth after enterocystoplasty in children and adolescents: a review. World J Urol 2004; 22: 196–9
Behr FD, Bangert JL, Hansen RC. Atypical pityriasis rubra pilaris associated with arthropathy and osteoporosis: a case report with 15-year follow-up. Pediatr Dermatol 2002; 19: 46–51
Dundaroz MR, Sarici SU, Turkbay T, et al. Evaluation of bone mineral density in chronic glue sniffers. Turk J Pediatr 2002; 44: 326–9
Lakhanpal S, Ginsburg WW, Luthra HS, et al. Transient regional osteoporosis: a study of 56 cases and review of the literature. Ann Intern Med 1987; 106: 444–50
Lorenc RS. Idiopathic juvenile osteoporosis. Calcif Tissue Int 2002; 70: 395–7
Saggese G, Bertelloni S, Baroncelli GI, et al. Mineral metabolism and calcitriol therapy in idiopathic juvenile osteoporosis. Am J Dis Child 1991; 145: 457–62
Krassas GE. Idiopathic juvenile osteoporosis. Ann N Y Acad Sci 2000; 900: 409–12
Smith R. Idiopathic juvenile osteoporosis: experience of twenty-one patients. Br J Rheumatol 1995; 34: 68–77
Bertelloni S, Baroncelli GI, Di Nero G, et al. Idiopathic juvenile osteoporosis: evidence of normal osteoblast function by 1,25-dihydroxy vitamin D3 stimulation test. Calcif Tissue Int 1992; 51: 20–3
Rauch F, Travers R, Norman ME, et al. Deficient bone formation in idiopathic juvenile osteoporosis: a histomorphometric study of cancellous iliac bone. J Bone Miner Res 2000; 15: 957–63
Rauch F, Travers R, Norman ME, et al. The bone formation defect in idiopathic juvenile osteoporosis is surface-specific. Bone 2002; 31: 85–9
Norman ME. Juvenile osteoporosis. In: Favus MJ, editor. Primer on the metabolic bone diseases and disorders of mineral metabolism. 4th ed. Philadelphia (PA): Lippincott Williams & Wilkins, 1999: 302–5
Loro ML, Sayre J, Roe TF, et al. Early identification of children predisposed to low peak bone mass and osteoporosis later in life. J Clin Endocrinol Metab 2000; 85: 3908–18
Brown JP. Osteoporosis in children: 2002 guidelines do not apply [letter]. CMAJ 2003; 168: 676
Batch JA, Couper JJ, Rodda C, et al. Use of bisphosphonate therapy for osteoporosis in childhood and adolescence. J Pediatr Child Health 2003; 39: 88–92
Reed A, Haugen M, Pachman LM, et al. 25-hydroxyvitamin D therapy in children with active juvenile rheumatoid arthritis: short-term effects on serum osteocalcin levels and bone density. J Pediatr 1991; 119: 657–60
Warady B, Lindsley C, Robinson R, et al. Effects of nutritional supplementation on bone mineral status in children with rheumatic disease receiving corticosteroid therapy. J Rheumatol 1994; 21: 530–5
Bianchi ML, Bardare M, Galbiati E, et al. Bone development in juvenile rheumatoid arthritis. In: Schonau E, Matkovic V, editors. Paediatric osteology: prevention of osteoporosis: a paediatric task? Singapore: Elsevier Science, 1998: 173–81
Eastell R, Reid DM, Compston J, et al. A UK consensus group on management of glucocorticoid-induced osteoporosis: an update. J Intern Med 1998; 244: 271–92
American College of Rheumatology Ad Hoc Committee on Glucocorticoid-In-duced Osteoporosis. Recommendations for the prevention and treatment of glucocorticoid-induced osteoporosis: 2001 update. Arthritis Rheum 2001; 44: 1496–503
Fischer MH, Adkins WN, Liebl BH, et al. Bone status in non-ambulant, epileptic, institutionalized youth. Clin Pediatr 1988; 27: 499–505
Hunt PA, Wu-Chen ML, Handal NJ, et al. Bone disease induced by anticonvulsant therapy and treatment with calcitriol (1,25-dihydroxyvitamin D3). Am J Dis Child 1986; 140: 715–8
Jekovec-Vrhovsek M, Kocijancic A, Prezelj J. Effect of vitamin D and calcium on bone mineral density in children with cerebral palsy and epilepsy in full-time care. Dev Med Child Neurol 2000; 42: 403–5
Bischoff HA, Stahelin HB, Dick W, et al. Effects of vitamin D and calcium supplementation on falls: a randomized controlled trial. J Bone Miner Res 2003; 18: 343–51
Nishioka T, Kurayama H, Yasuda T, et al. Nasal administration of salmon calcitonin for prevention of glucocorticoid-induced osteoporosis in children with nephrosis. J Pediatr 1991; 118: 703–7
Rebelo I, da Silva LP, Blanco JC, et al. Effects of synthetic salmon calcitonin therapy in children with osteogenesis imperfecta. J Int Med Res 1989; 17: 401–5
Nishi Y, Hamamoto K, Kajiyama M, et al. Effect of long-term calcitonin therapy by injection and nasal spray on the incidence of fractures in osteogenesis imperfecta. J Pediatr 1992; 121: 477–80
Tuysuz B, Mercimek S, Ungur S, et al. Calcitonin treatment in osteoectasia with hyperphosphatasia (juvenile Paget’s disease): radiographic changes after treatment. Pediatr Radiol 1999; 29: 838–41
Canatan D, Akar N, Arcasoy A. Effects of calcitonin therapy on osteoporosis in patients with thalassemia. Acta Haematol 1995; 93: 20–4
Vichinsky EP. The morbidity of bone disease in thalassemia. Ann N Y Acad Sci 1998; 850: 344–8
Jackson EC, Strife F, Tsang RC, et al. Effect of calcitonin replacement therapy in idiopathic juvenile osteoporosis. Am J Dis Child 1988; 142: 1237–9
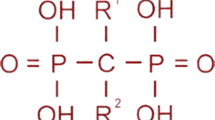
Russell RGG, Croucher PI, Rogers MJ. Bisphosphonates: pharmacology, mechanisms of action and clinical uses. Osteoporos Int 1999; 9Suppl. 1: S66–80
Allgrove J. Use of bisphosphonates in children and adolescents. J Pediatr Endocrinol Metab 2002; 15: 921–8
Koné Paut I, Gennari JM, Retornaz K, et al. Les biphosphonates chez l’enfant: présent et avenir. Arch Pédiatr 2002; 8: 836–42
Glorieux FH, Bishop NJ, Plotkin H, et al. Cyclic administration of pamidronate in children with severe osteogenesis imperfecta. N Engl J Med 1998; 39: 947–52
Astrom E, Soderhall S. Beneficial effect of long term intravenous bisphosphonate treatment of osteogenesis imperfecta. Arch Dis Child 2002; 86: 356–64
Devogelaer JP. New uses of bisphosphonates: osteogenesis imperfecta. Curr Opin Pharamcol 2002; 2: 748–53
Giraud F, Meunier PJ. Effect of cyclical intravenous pamidronate therapy in children with osteogenesis imperfecta: open-label study in seven patients. Joint Bone Spine 2002; 69: 486–90
Zeitlin L, Rauch F, Plotkin H, et al. Height and weight development during fouryears of therapy with cyclical intravenous pamidronate in children and adolescents with osteogenesis imperfecta types I, III, and IV. Pediatrics 2003; 111: 1030–6
Van Persijn van Meerten EL, Kroon HM, Papapoulos SE. Epi- and metaphyseal changes in children caused by administration of bisphosphonates. Radiology 1992; 184: 249–54
Bianchi ML, Cimaz R, Bardare M, et al. Efficacy and safety of alendronate for the treatment of osteoporosis in diffuse connective tissue disease in children. Arthritis Rheum 2000; 43: 1960–6
Wright NM. Just taller or more bone? The impact of growth hormone on osteogen-esis imperfecta and idiopathic juvenile osteoporosis. J Pediatr Endocrinol Metab 2000; 13: 999–1002
Antoniazzi F, Bertoldo F, Mottes M, et al. Growth hormone treatment in osteogen-esis imperfecta with quantitative defect of type I collagen synthesis. J Pediatr 1996; 129: 432–9
Marini JC, Hopkins E, Glorieux FH, et al. Positive linear growth and bone responses to growth hormone treatment in children with types III and IV osteogenesis imperfecta: high predictive value of the carboxylterminal propeptide of type I procollagen. J Bone Miner Res 2003; 18: 237–43
Rooney M, Davies UM, Reeve J, et al. Bone mineral content and bone mineral metabolism: changes after growth hormone treatment in juvenile chronic arthritis. J Rheumatol 2000; 27: 1073–81
Touati G, Ruiz J-C, Porquet D, et al. Effects on bone metabolism of one year recombinant human growth hormone administration to children with juvenile chronic arthritis undergoing chronic steroid therapy. J Rheumatol 2000; 27: 1287–93
Simon D, Lucidarme N, Prieur AM, et al. Effects on growth and body composition of growth hormone treatment in children with juvenile idiopathic arthritis requiring steroid therapy. J Rheumatol 2003; 30: 2492–9
Bechtold S, Ripperger P, Bonfig W, et al. Bone mass development and bone metabolism in juvenile idiopathic arthritis: treatment with growth hormone for 4 years. J Rheumatol 2004; 31: 1407–12
Bechtold S, Ripperger P, Bonfig W, et al. Growth hormone changes bone geometry and body composition in patients with juvenile idiopathic arthritis requiring glucocorticoid treatment: a controlled study using peripheral quantitative computed tomography. J Clin Endocrinol Metab 2005; 90: 3168–73
Marcus R. Exercise: moving in the right direction. J Bone Miner Res 1998; 13: 1793–6
Janz KF, Burns TL, Torner JC, et al. Physical activity and bone measures in young children: the Iowa Bone Development Study. Pediatrics 2001; 107: 1387–93
Cassell C, Benedict M, Specker B. Bone mineral density in elite 7- to 9-yr-old female gymnasts and swimmers. Med Sci Sports Exerc 1996; 28: 1243–6
Courteix D, Lespessailles E, Loiseau Peres S, et al. Effect of physical training on bone mineral density in prepubertal girls: a comparative study between impact-loading and non-impact-loading sports. Osteoporos Int 1998; 8: 152–8
Bonner FJ, Sinaki M, Grabois M, et al. Health professional’s guide to rehabilitation of the patient with osteoporosis. Osteoporos Int 2003; 14Suppl. 2: S1–22
Fleming R, Patrick K. Osteoporosis prevention: pediatricians’ knowledge, attitudes, and counseling practices. Prev Med 2002; 34: 411–21
Boreham C, Riddoch C. The physical activity, fitness and health of children. J Sports Sci 2001; 19: 915–29
Metzl JD. Strength training and nutritional supplement use in adolescents. Curr Opin Pediatr 1999; 11: 292–6
Shaw NJ. Management of childhood osteoporosis [letter]. Arch Dis Child 2003; 88: 91
Acknowledgments
The authors have no conflicts of interest that are directly relevant to the content of this study. The authors received the Research National Project no. 2003064547003, granted by the Italian Ministry of Health.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Baroncelli, G.I., Bertelloni, S., Sodini, F. et al. Osteoporosis in Children and Adolescents. Pediatr-Drugs 7, 295–323 (2005). https://doi.org/10.2165/00148581-200507050-00003
Published:
Issue Date:
DOI: https://doi.org/10.2165/00148581-200507050-00003