Abstract
Background: Postherpetic neuralgia (PHN) is a common, debilitating complication of herpes zoster that has a major impact on patients’ quality of life. PHN prevalence increases with advancing age. One treatment option is the topical analgesic 5% lidocaine (lignocaine) medicated plaster (Versatis®), which has been proven to be efficacious and well tolerated in a number of randomized clinical studies.
Objective: The aim of this analysis was to assess the use of the lidocaine medicated plaster under clinical practice conditions in a patient population whose previous PHN treatment with antidepressant and/or antiepileptic agents was inadequate or was not tolerated, or for whom such treatment was contraindicated or not recommended.
Methods: This was a prospective, multicentre, non-interventional observation conducted in private and public health centres in France under a compassionate use programme (CUP). To obtain this new — and, at the time, unauthorized — PHN treatment alternative, physicians (in accordance with French guidelines) had to complete standardized case report forms for each patient before his/her inclusion in the CUP. As it was a CUP and therefore a non-interventional observation, returning documented information on follow-up visits to the medication provider was voluntary, and only a limited number of physicians returned completed forms. Documentation was, however, mandatory for adverse events (AEs) occurrence. Depending on the size of the painful skin area, up to three lidocaine plasters daily were applied for a maximum of 12 hours with plaster-free intervals of at least 12 hours. The study assessed changes in the prescription of concomitant PHN medication from the start of lidocaine plaster treatment to the last follow-up visit, both in terms of the sum of all concomitant PHN treatments and stratified by type of treatment: antiepileptic drugs, tricyclic antidepressants (TCAs), serotonin reuptake inhibitors (SRIs), classical analgesics (classified as step 1, 2 or 3 according to the WHO cancer pain ladder), transcutaneous electrical nerve stimulation, and others (mainly NSAIDs). AEs were monitored for safety.
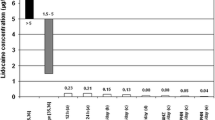
Results: A total of 625 patients were included in the CUP and permitted to receive lidocaine plaster treatment. Physicians returned 273 documented follow-up visit report forms. The mean ± SD CUP duration (i.e. duration of lidocaine plaster treatment) was 2.4 ± 2.5 months (median 1 month). Efficacy was assessed in the group of patients with documented follow-up visits (n = 273; mean ± SD age 73.6 ± 11.2 years), of whom 184 were aged ≥70 years (elderly efficacy population). The safety analysis included 625 patients (mean ± SD age 73.2 ± 11.9 years). Lidocaine plaster treatment resulted in a significant mean reduction of one concomitant PHN treatment per patient in the overall efficacy population analysed at the end of the observation (p < 0.001). In both populations (overall efficacy and elderly efficacy population), significantly fewer patients received TCAs (p = 0.003 and p = 0.001, respectively), step 3 analgesics (p =0.001 and p =0.005, respectively), and other miscellaneous treatments (p <0.001 for both populations); there was also a significant reduction in the proportion of patients who took step 2 analgesics (p = 0.009) in the overall efficacy group. AEs (mainly related to local plaster application) were documented for 2.6% of the patients in the safety population; none were considered serious.
Conclusions: In day-to-day clinical practice management of PHN, treatment with the 5% lidocaine medicated plaster permitted a significant quantitative reduction in concomitant treatments for neuropathic pain in the overall efficacy population. In the subgroup aged ≥70 years, the quantitative reduction was non-significant. However, in both populations, 5% lidocaine medicated plaster reduced use of TCAs and step 3 analgesics. An improved polymedication status and good tolerability in this likely multimorbid age group indicate that the plaster is a new therapeutic alternative for patients suffering from PHN in France.




Similar content being viewed by others
References
Bouhassira D, Lantéri-Minet M, Attal N, et al. Prevalence of chronic pain with neuropathic characteristics in the general population. Pain 2008; 136(3): 380–7
Johnson RW, Wasner G, Saddier P, et al. Herpes zoster and postherpetic neuralgia: optimizing management in the elderly patient. Drugs Aging 2008; 25(12): 991–1006
Dworkin RH, Gnann Jr JW, Oaklander AL, et al. Diagnosis and assessment of pain associated with herpes zoster and postherpetic neuralgia. J Pain 2008 Jan; 9Suppl.1: S37–44
Johnson RW, McElhaney J. Postherpetic neuralgia in the elderly. Int J Clin Pract 2009 Sep; 63(9): 1386–91
Sadosky A, McDermott AM, Brandenburg NA, et al. A review of the epidemiology of painful diabetic neuropathy, postherpetic neuralgia, and less commonly studied neuropathic pain conditions. Pain Practice 2008 Mar; 8(1): 45–56
Dworkin RH, Malone DC, Panarites CJ, et al. Impact of post-herpetic neuralgia and painful diabetic peripheral neuropathy on health care costs. J Pain 2010 Apr; 11(4): 360–8
Gauthier A, Breuer J, Carrington D, et al. Epidemiology and cost of herpes zoster and post-herpetic neuralgia in the United Kingdom. Epidemiol Infect 2009 Jan; 137(1): 38–47
Yawn BP, Saddier P, Wollan PC, et al. A population-based study of the incidence and complication rates of herpes zoster before zoster vaccine introduction. Mayo Clin Proc 2007 Nov; 82(11): 1341–9
Johnson RW, Bouhassira D, Kassianos G, et al. The impact of herpes zoster and post-herpetic neuralgia on quality-of-life. BMC Med 2010 Jun 21; 8(1): 37
Oster G, Harding G, Dukes E, et al. Pain, medication use, and health-related quality of life in older persons with postherpetic neuralgia: results from a population-based survey. J Pain 2005 Jun; 6(6): 356–63
Baron R, Binder A, Wasner G. Neuropathic pain: diagnosis, pathophysiological mechanisms, and treatment. Lancet Neurol 2010 Aug; 9: 807–19
Baron R, Tölle TR, Gockel U, et al. A cross-sectional cohort survey in 2100 patients with painful neuropathy and post-herpetic neuralgia: differences in demographic data and sensory symptoms. Pain 2009 Nov; 146(1–2): 34–40
Finnerup NB, Otto M, Jensen TS, et al. An evidence-based algorithm for the treatment of neuropathic pain. Med-GenMed 2007 May 15; 9(2): 36
Dworkin RH, O’Connor AB, Audette J, et al. Recommendations for the pharmacological management of neuropathic pain: an overview and literature update. Mayo Clin Proc 2010 Mar; 85 (3 Suppl.): S3–14
Rowbotham MC, Davies PS, Verkempinck C, et al. Lidocaine patch: double-blind controlled study of a new treatment method for post-herpetic neuralgia. Pain 1996 Apr; 65(1): 39–44
Galer BS, Rowbotham MC, Perander J, et al. Topical lidocaine patch relieves postherpetic neuralgia more effectively than a vehicle topical patch: results of an enriched enrollment study. Pain 1999 Apr; 80(3): 533–8
Baron R, Mayoral V, Leijon G, et al. 5% lidocaine medicated plaster versus pregabalin in post-herpetic neuralgia and diabetic polyneuropathy: an open-label, non-inferiority two-stage RCT study. Curr Med Res Opin 2009 Jul; 25(7): 1663–76
Binder A, Bruxelle J, Rogers P, et al. Topical 5% lidocaine (lignocaine) medicated plaster treatment for post-herpetic neuralgia: results of a double-blind, placebo-controlled, multinational efficacy and safety trial. Clin Drug Investig 2009; 29(6): 393–408
Rehm S, Binder A, Baron R. Post-herpetic neuralgia — 5% lidocaine medicated plaster, pregabalin, or a combination of both? A randomized, open, clinical effectiveness study. Curr Med Res Opin 2010 Jul; 26(7): 1607–19
Galer BS, Gammaitoni AR. More than 7 years of consistent neuropathic pain relief in geriatric patients. Arch Intern Med 2003 Mar 10; 163(5): 628
Hans G, Sabatowski R, Binder A, et al. Efficacy and tolerability of a 5% lidocaine medicated plaster for the topical treatment of post-herpetic neuralgia: results of a long-term study. Curr Med Res Opin 2009 May; 25(5): 1295–305
Agence Francaise de Sécurité Sanitaire des Produits de Santé (AFSSAPS). Notice to applicants for Temporary Authorisation for Use (ATU) [in French]. 2007 Nov [online]. Available from URL: http://www.afssaps.fr/Activites/Autorisations-temporaires-d-utilisation [Accessed 2011 Jun 1]
World Health Organisation. Cancer pain ladder [online]. Available from URL: http://www.who.int/cancer/palliative/painladder/en/ [Accessed 2010 Jul 15]
International Federation of Pharmaceutical Manufacturers and Associations (IFPMA). Medical dictionary for regulatory activities (MedDRA). Version 11. Chantilly (VA): MedDRA MSSO, 2008
Attal N, Cruccu G, Baron R, et al. EFNS guidelines on the pharmacological treatment of neuropathic pain: 2010 revision. Eur J Neurol 2010; 17(9): 1113–e88
Douglas MW, Johnson RW, Cunningham AL. Tolerability of treatments for postherpetic neuralgia. Drug Saf 2004; 27: 1217–33
Zin CS, Nissen LM, Smith MT. An update on the pharmacological management of post-herpetic neuralgia and painful diabetic neuropathy. CNS Drugs 2008; 22(5): 714–42
McKeage K, Keam SJ. Pregabalin: in the treatment of postherpetic neuralgia. Drugs Aging 2009; 26(10): 883–92
Gammaitoni AR, Alvarez NA, Galer BS. Safety and tolerability of the lidocaine patch 5%, a targeted peripheral analgesic: a review of the literature. J Clin Pharmacol 2003 Feb; 43(2): 111–7
Chidiac C, Bruxelle J, Daures J-P, et al. Characteristics of patients with herpes zoster on presentation to practitioners in France. Clin Infect Dis 2001 July; 33: 62–9
Van Seventer R, Sadosky A, Lucero M, et al. A crosssectional survey of heath state impairment and treatment patterns in patients with postherpetic neuralgia. Age Ageing 2006; 35: 132–7
Burt CW, Woodwell D. Tests of methods to improve response to physician surveys [online]. Available from URL: http://www.fcsm.gov/05papers/Burt_Woodwell_VIIB.pdf [Accessed 2011 Mar 1]
Acknowledgements
The study was sponsored by Grünenthal GmbH, Aachen, Germany. The sponsor was involved in the study design, the collection, analysis and interpretation of data, and the writing of the manuscript, and made the decision to submit the paper for publication.
Florentin Clère, Claire Delorme-Morin, Brigitte George, Malou Navez, Bruno Rioult and Florence Tiberghien-Chatelain were contracted as study investigators. Hervé Ganry is an employee of the sponsor. The authors thank Elke Grosselindemann (Brett Medical Writing, Bibra Lake, Australia) and Birgit Brett (Brett Medical Writing, Pulheim, Germany) for editorial assistance and publication coordination. All costs associated with the development and publication of the present manuscript were met by the sponsor.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Clère, F., Delorme-Morin, C., George, B. et al. 5% Lidocaine Medicated Plaster in Elderly Patients with Postherpetic Neuralgia. Drugs Aging 28, 693–702 (2011). https://doi.org/10.2165/11595600-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11595600-000000000-00000