Abstract
Background: Fluoroquinolones are widely used both in primary care and in hospital settings. Since the last comparison performed in Italy on the safety profiles of different fluoroquinolones, a new molecule, prulifloxacin, has been introduced into the market and several warnings concerning this class of drugs have been released. The aim of this study was to reassess the safety profiles of fluoroquinolones using the database of the Italian Interregional Group of Pharmacovigilance (IGP) and the administrative data of fluoroquinolone prescriptions.
Methods: All adverse drug reactions (ADRs) reported in four Italian regions (Lombardy, Veneto, Emilia Romagna and Tuscany) were retrieved from the IGP database. Consumption data (defined daily dose [DDD]/1000 inhabitants/ day) were used as denominators. Both single reports and all ADRs (classified by System Organ Classes and MedDRA® Preferred Term [PT]) due to fluoroquinolones were considered as numerators of each analysis, comparing two periods (2005 vs 2006). All fluoroquinolones with at least ten reports per year were included in the analysis.
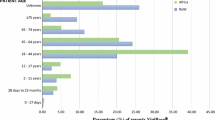
Results: On the basis of 272 reports (532 single ADRs or PTs), patients did not show any statistically significant differences between 2005 and 2006 in terms of sex, age and number of concurrent medications. After adjustment for drug consumption, moxifloxacin showed the highest reporting rate (84.6 reports/ DDD/1000 inhabitants/day; 15.4 serious reports/DDD/1000 inhabitants/day) followed by prulifloxacin (72.2; 22.2 serious) and levofloxacin (55.3; 30.6 serious) in 2005. An increment of ADR/report rates was observed over the 2 years for all fluoroquinolones except prulifloxacin, which had the lowest ADR reporting rate in 2006 (25.0; 12.5 serious). In 2006, the rate of serious ADRs associated with prulifloxacin was lower than with ciprofloxacin, while in 2005 serious events were almost equal for both compounds (55.6 vs 47.6 serious ADRs/DDD/1000 inhabitants/day). Ciprofloxacin showed the highest proportion of cutaneous PTs (e.g. rash, exanthema). Tendinopathies were mainly due to levofloxacin.
Conclusions: These data suggest that different fluoroquinolones are characterized by different rates and types of ADRs. Among them, prulifloxacin was associated with more ADRs than other fluoroquinolones in 2005 but with fewer ADRs in 2006, when its consumption increased. Although these findings may represent an encouraging perspective towards a more appropriate use of fluoroquinolones because of their individual safety profiles, further pharmacoepidemiological studies must be performed to substantiate these results.







Similar content being viewed by others
References
Osservatorio Nazionale sull’Impiego dei Medicinali. L’uso dei farmaci in Italia. Rapporto Nazionale. Rome: Direzione Generale della Valutazione dei medicinali e della Farmacovigilanza, 2004
Osservatorio Nazionale sull’Impiego dei Medicinali. L’uso dei farmaci in Italia. Rapporto Nazionale. Rome: Direzione Generale della Valutazione dei medicinali e della Farmacovigilanza, 2005
Osservatorio Nazionale sull’Impiego dei Medicinali. L’uso dei farmaci in Italia. Rapporto Nazionale. Rome: Direzione Generale della Valutazione dei medicinali e della Farmacovigilanza, 2006
Osservatorio Nazionale sull’Impiego dei Medicinali. L’uso dei farmaci in Italia. Rapporto Nazionale. Rome: Direzione Generale della Valutazione dei medicinali e della Farmacovigilanza, 2007
Mehlhorn AJ, Brown DA. Safety concerns with fluoroquinolones. Ann Pharmacother 2007; 41(11): 1859–66
Owens Jr RC, Ambrose PG. Clinical use of the fluoroquinolones. Med Clin North Am 2000; 84(6): 1447–69
Mohr JF, McKinnon PS, Peymann PJ, et al. A retrospective, comparative evaluation of dysglycemias in hospitalized patients receiving gatifloxacin, levofloxacin, ciprofloxacin, or ceftriaxone. Pharmacotherapy 2005; 25(10): 1303–9
Owens Jr RC, Ambrose PG. Antimicrobial safety: focus on fluoroquinolones. Clin Infect Dis 2005; 41 Suppl. 2: S144–57
Leone R, Venegoni M, Motola D, et al. Adverse drug reactions related to the use of fluoroquinolone antimicrobials: an analysis of spontaneous reports and fluoroquinolone consumption data from three Italian regions. Drug Saf 2003; 26(2): 109–20
Gruppo Interregionale di Farmacovigilanza (GIF) [online]. Available from URL: http://www.gruppogif.org [Accessed 2009 Mar 30]
Gazzetta Ufficiale della Repubblica Italiana n∘ 101 03 Maggio 2003. Rome: Decreto Legislativo n∘ 95, 2003 Apr 8
Keam SJ, Perry CM. Prulifloxacin. Drugs 2004; 64(19): 2221–34
Rossi M, Lusini G, Biasella A, et al. Prulifloxacin as a trigger of myasthenia gravis. J Neurol Sci 2009; 280(1–2): 109–10
Gallelli L, Gallelli A, Vero G, et al. Acute renal failure probably induced by prulifloxacin in an elderly woman: a first case report. Clin Drug Investig 2006; 26(1): 49–53
Pierfitte C, Begaud B, Lagnaoui R, et al. Is reporting rate a good predictor of risks associated with drugs? Br J Clin Pharmacol 1999; 47(3): 329–31
Brown EG. Effects of coding dictionary on signal generation: a consideration of use of MedDRA compared with WHO-ART. Drug Saf 2002; 25(6): 445–52
Giezen TJ, Mantel-Teeuwisse AK, Leufkens HG. Pharmacovigilance of biopharmaceuticals: challenges remain. Drug Saf 2009; 32(10): 811–7
WHO technical report no. 498 1972 [online]. Available from URL: http://www.who-umc.org/DynPage.aspx?id=22676 [Accessed 2006 Dec 1]
Olsson S. The role of the WHO programme on International Drug Monitoring in coordinating worldwide drug safety efforts. Drug Saf 1998; 19(1): 1–10
Weber JCP. Epidemiology of adverse reactions to non-steroidal anti-inflammatory drugs. In: Rainford KD, Velo GP, editors. Advances in information research 6. New York: Raven Press, 1984: 1–7
de Graaf L, Fabius MA, Diemont WL, et al. The Webercurve pitfall: effects of a forced introduction on reporting rates and reported adverse reaction profiles. Pharm World Sci 2003; 25(6): 260–3
Autorizzazione all’immissione in commercio della specialita’ medicinale per uso umano «Keraflox». Decreto A.I.C. n. 310 del 21 giugno 2004. Rome: Gazzetta Ufficiale della Repubblica Italiana, 2004
Van Bambeke F, Michot JM, Van Eldere J, et al. Quinolones in 2005: an update. Clin Microbiol Infect 2005; 11(4): 256–80
Salas M, Hofman A, Stricker BH. Confounding by indication: an example of variation in the use of epidemiologic terminology. Am J Epidemiol 1999; 149(11): 981–3
Khaliq Y, Zhanel GG. Fluoroquinolone-associated tendinopathy: a critical review of the literature. Clin Infect Dis 2003; 36(11): 1404–10
van der Linden PD, Sturkenboom MC, Herings RM, et al. Fluoroquinolones and risk of Achilles tendon disorders: case-control study. BMJ 2002; 324(7349): 1306–7
van der Linden PD, Sturkenboom MC, Herings RM, et al. Increased risk of Achilles tendon rupture with quinolone antibacterial use, especially in elderly patients taking oral corticosteroids. Arch Intern Med 2003; 163(15): 1801–7
Ambrose PG, Owens Jr RC, Quintiliani R, et al. New generations of quinolones: with particular attention to levofloxacin. Conn Med 1997; 61(5): 269–72
Nori S, Nebesio C, Brashear R, et al. Moxifloxacin-associated drug hypersensitivity syndrome with toxic epidermal necrolysis and fulminant hepatic failure. Arch Dermatol 2004; 140(12): 1537–8
Johannes CB, Ziyadeh N, Seeger JD, et al. Incidence of allergic reactions associated with antibacterial use in a large, managed care organisation. Drug Saf 2007; 30(8): 705–13
Van Bambeke F, Tulkens PM. Safety profile of the respiratory fluoroquinolone moxifloxacin: comparison with other fluoroquinolones and other antibacterial classes. Drug Saf 2009; 32(5): 359–78
Shehab N, Patel PR, Srinivasan A, et al. Emergency department visits for antibiotic-associated adverse events. Clin Infect Dis 2008; 47(6): 735–43
Hauben M, Aronson JK. Defining ‘signal’ and its subtypes in pharmacovigilance based on a systematic review of previous definitions. Drug Saf 2009; 32(2): 99–110
Goossens H, Ferech M, Vander SR, et al. Outpatient antibiotic use in Europe and association with resistance: a cross-national database study. Lancet 2005; 365(9459): 579–87
Ferech M, Coenen S, Malhotra-Kumar S, et al. European Surveillance of Antimicrobial Consumption (ESAC): outpatient quinolone use in Europe. J Antimicrob Chemother 2006; 58(2): 423–7
Coenen S, Ferech M, Haaijer-Ruskamp FM, et al. European Surveillance of Antimicrobial Consumption (ESAC): quality indicators for outpatient antibiotic use in Europe. Qual Saf Health Care 2007; 16(6): 440–5
Elseviers MM, Ferech M, Vander Stichele RH, et al. Antibiotic use in ambulatory care in Europe (ESAC data 1997–2002): trends, regional differences and seasonal fluctuations. Pharmacoepidemiol Drug Saf 2007; 16(1): 115–23
Goossens H, Ferech M, Coenen S, et al. Comparison of outpatient systemic antibacterial use in 2004 in the United States and 27 European countries. Clin Infect Dis 2007; 44(8): 1091–5
Vander Stichele RH, Elseviers MM, Ferech M, et al. European surveillance of antimicrobial consumption (ESAC): data collection performance and methodological approach. Br J Clin Pharmacol 2004; 58(4): 419–28
Tubert-Bitter P, Begaud B, Moride Y, et al. Comparing the toxicity of two drugs in the framework of spontaneous reporting: a confidence interval approach. J Clin Epidemiol 1996; 49(1): 121–3
Acknowledgements
We are very grateful to the Pharmaceutical Departments of Emilia Romagna, Lombardy, Tuscany and Veneto regions, and their Local Health Authorities, for supplying consumption data and collecting the adverse reaction forms. No sources of funding were used to assist in the preparation of this study. The authors have no conflicts of interest that are directly relevant to the content of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lapi, F., Tuccori, M., Motola, D. et al. Safety Profile of the Fluoroquinolones. Drug-Safety 33, 789–799 (2010). https://doi.org/10.2165/11536810-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11536810-000000000-00000