Abstract
Venous thromboembolism (VTE) is a common complication and a leading cause of death in oncological patients. Recent guidelines have been established for the treatment and prevention of VTE in oncological patients in various clinical situations. These guidelines recommend: (a) prophylactic anticoagulation in all hospitalized oncological patients in whom there are no contraindications; (b) prophylactic anticoagulation in patients scheduled for major oncological surgery in whom there are no contraindications; (c) prolonged (≥6 months) anticoagulant therapy in oncological patients with manifest VTE in order to prevent a new episode; (d) no routine prophylactic anticoagulation in ambulatory patients without VTE receiving chemotherapy, except when they are receiving treatment with anti-cancer agents with a high risk of thrombogenicity, such as thalidomide- or lenalidomide-based chemotherapeutic regimens; and (e) no use of prophylactic anticoagulants to improve survival in patients with cancer without manifest VTE.
Although vitamin K antagonists, unfractionated heparin and in some cases fondaparinux sodium could be used for the treatment of VTE, low molecular weight heparins are recommended for initial and continuous anticoagulant treatment in oncological patients with VTE, as well as for its prevention.


Similar content being viewed by others
References
Khorana AA, Francis CW, Culakova E, et al. Thromboembolism is a leading cause of death in cancer patients receiving outpatient chemotherapy. J Thromb Haemost 2007; 5: 632–4
Stein PD, Beemath A, Meyers FA, et al. Incidence of venous thromboembolism in patients hospitalized with cancer. Am J Med 2006; 119: 60–8
Khorana AA, Francis CW, Culakova E, et al. Thromboembolism in hospitalized neutropenic cancer patients. J Clin Oncol 2006; 24: 484–90
Heit JA, Silverstein MD, Mohr DN, et al. Risk factors for deep vein thrombosis and pulmonary embolism: a population-based case-control study. Arch Intern Med 2000; 160: 809–15
Kroger K, Weiland D, Ose C, et al. Risk factors for venous thromboembolic events in cancer patients. Ann Oncol 2006; 17: 297–303
Sousou T, Khorana AA. New insights into cancer-associated thrombosis. Arterioscler Thromb Vasc Biol 2009; 29: 316–20
Khorana AA, Francis CW, Culakova E, et al. Risk factors for chemotherapy-associated venous thromboembolism in a prospective observational study. Cancer 2005; 104: 2822–9
Blom JW, Vanderschoot JP, Oostindier MJ, et al. Incidence of venous thrombosis in a large cohort of 66 329 cancer patients: results of a record linkage study. J Thromb Haemost 2006; 4: 529–35
Zangari M, Anaissie E, Barlogie B, et al. Increased risk of deep-vein thrombosis in patients with multiple myeloma receiving thalidomide and chemotherapy. Blood 2001; 98: 1614–5
Nalluri SR, Chu D, Keresztes R, et al. Risk of venous thromboembolism with the angiogenesis inhibitor bevacizumab in cancer patients: a meta-analysis. JAMA 2008; 300: 2277–85
Agnelli G, Bolis G, Capussotti L, et al. A clinical outcome-based prospective study on venous thromboembolism after cancer surgery: the @RISTOS project. Ann Surg 2006; 243: 89–95
Gallus AS. Prevention of post-operative deep leg vein thrombosis in patients with cancer. Thromb Haemost 1997; 78: 126–32
Prandoni P, Lensing AW, Piccioli A, et al. Recurrent venous thromboembolism and bleeding complications during anticoagulant treatment in patients with cancer and venous thrombosis. Blood 2002; 100: 3484–8
Elting LS, Escalante CP, Cooksley C, et al. Outcomes and cost of deep venous thrombosis among patients with cancer. Arch Intern Med 2004; 164: 1653–61
Leonardi MJ, McGory ML, Ko CY. A systematic review of deep venous thrombosis prophylaxis in cancer patients: implications for improving quality. Ann Surg Oncol 2007; 14: 929–36
van Doormaal FF, Buller HR, Middeldorp S. Development in anticoagulant therapy. Crit Rev Oncol Hematol 2008; 66: 145–54
Levine M, Hirsh J, Gent M, et al. Double-blind randomised trial of a very-low-dose warfarin for prevention of thromboembolism in stage IV breast cancer. Lancet 1994; 343: 886–9
Smorenburg SM, Vink R, Otten HM, et al. The effects of vitamin K-antagonists on survival of patients with malignancy: a systematic analysis. Thromb Haemost 2001; 86: 1586–7
Siragusa S, Cosmi B, Piovella F, et al. Low-molecular-weight heparins and unfractionated heparin in the treatment of patients with acute venous thromboembolism: results of a meta-analysis. Am J Med 1996; 100: 269–77
Lyman GH, Khorana AA, Falanga A, et al. American Society of Clinical Oncology guideline: recommendations for venous thromboembolism prophylaxis and treatment in patients with cancer. J Clin Oncol 2007; 25: 5490–505
Agencia Española del Medicamento (Spanish Drug Agency) [online]. Available from URL: http://www.agemed.es/www. agemed.es [Accessed 2009 Mar 10]
Enoxaparin sodium injection (Lovenox®) for subcutaneous and intravenous use: prescribing information, 2007 [online]. Available from URL: http://www.accessdata.fda. gov/drugsatfda_docs/label/2007/022138,020164s075lbl.pdf [Accessed 2007 May 16]
Tinzaparinsodium injection [Innohep]: prescribing information, 2008 [online]. Available from URL: http://www. accessdata.fda.gov/drugsatfda_docs/label/2008/020484s011lbl. pdf [Accessed 2009 May 21]
Cheer SM, Dunn CJ, Foster R. Tinzaparin sodium: a review of its pharmacology and clinical use in the prophylaxis and treatment of thromboembolic disease. Drugs 2004; 64: 1479–502
Dalteparin (Fragmin): prescribing information, 2009 [online]. Available from URL: http://www.accessdata.fda.gov/ drugsatfda_docs/label/2007/020287s035lbl.pdf [Accessed 2009 May 15]
Dunn CJ, Jarvis B. Dalteparin: an update of its pharmacological properties and clinical efficacy in the prophylaxis and treatment of thromboembolic disease. Drugs 2000; 60: 203–37
Lee AY, Levine MN, Baker RI, et al. Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer. N Engl J Med 2003; 349: 146–53
Fraxiparine, Fraxiparine Forte (nadroparin calcium) product monograph (Canada). GlaxoSmithKline, 2008 [online]. Available from URL: http://www.gsk.ca/english/docs-pdf/ Fraxiparine_Forte_PM_20080916_EN.pdf [Accessed 2009 Jul 20]
Agnelli G, Gussoni G, Bianchini C, et al. A randomized double-blind placebo-controlled study on nadroparin for prophylaxis of thromboembolic events in cancer patients receiving chemotherapy: the PROTECHT study [abstract]. Blood 2008; 112: 6
Martinez-Gonzalez J, Vila L, Rodriguez C. Bemiparin: second-generation, low-molecular-weight heparin for treatment and prophylaxis of venous thromboembolism. Expert Rev Cardiovasc Ther 2008; 6: 793–802
Chapman TM, Goa KL. Bemiparin: a review of its use in the prevention of venous thromboembolism and treatment of deep vein thrombosis. Drugs 2003; 63: 2357–77
Adjuvant BEmiparin in Small Cell Lung Carcinoma (ABEL STUDY) [NCT00324558], 2009 [online]. Available from URL: http://clinicaltrials.gov/ct2/show/NCT00324558 [Accessed 2009 May 21]
CANBESURE STUDY (Cancer, Bemiparin and Surgery Evaluation) [ClinicalTrials.gov identifier NCT00219973], US National Institutes of Health, ClinicalTrials.gov [online]. Available from URL: http://clinicaltrials.gov/ [Accessed 2009 May 21]
Gomez-Outes A, Rocha E, Martinez-Gonzalez J, et al. Cost effectiveness of bemiparin sodium versus unfractionated heparin and oral anticoagulants in the acute and long-term treatment of deep vein thrombosis. Pharmacoeconomics 2006; 24: 81–92
Schadlich PK, Kentsch M, Weber M, et al. Cost effectiveness of enoxaparin as prophylaxis against venous thrombo-embolic complications in acutely ill medical inpatients: modelling study from the hospital perspective in Germany. Pharmacoeconomics 2006; 24: 571–91
Heerey A, Suri S. Cost effectiveness of dalteparin for preventing venous thromboembolism in abdominal surgery. Pharmacoeconomics 2005; 23: 927–44
Caro JJ, Getsios D, Caro I, et al. Cost effectiveness of tinzaparin sodium versus unfractionated heparin in the treatment of proximal deep vein thrombosis. Pharmacoeconomics 2002; 20: 593–602
Mousa SA. Role of current and emerging antithrombotics in thrombosis and cancer. Drugs Today (Barc) 2006; 42: 331–50
Fondaparinux sodium (Arixtra): prescribing information, 2009 [online]. Available from URL: http://www.accessdata.fda. gov/drugsatfda_docs/label/2005/021345s010lbl.pdf [Accessed 2009 May 21]
Dhillon S, Plosker GL. Fondaparinux: use in thrombo-prophylaxis of acute medical patients. Drugs Aging 2008; 25: 81–8
Robinson DM, Wellington K. Fondaparinux sodium: a review of its use in the treatment of acute venous thromboembolism. Am J Cardiovasc Drugs 2005; 5: 335–46
Wong CK, White HD. Direct antithrombins: mechanisms, trials, and role in contemporary interventional medicine. Am J Cardiovasc Drugs 2007; 7: 249–57
Eriksson BI, Borris LC, Friedman RJ, et al. Rivaroxaban versus enoxaparin for thromboprophylaxis after hip arthroplasty. N Engl J Med 2008; 358: 2765–75
Mandala M, Falanga A, Piccioli A, et al. Venous thromboembolism and cancer: guidelines of the Italian Association of Medical Oncology (AIOM). Crit Rev Oncol Hematol 2006; 59: 194–204
Wagman LD, Baird MF, Bennett CL, et al. Venous thromboembolic disease. NCCN. Clinical practice guidelines in oncology. J Natl Compr Canc Netw 2008; 6: 716–53
Khorana AA. The NCCN clinical practice guidelines on venous thromboembolic disease: strategies for improving VTE prophylaxis in hospitalized cancer patients. Oncologist 2007; 12: 1361–70
Mandala M, Falanga A, Roila F. Management of venous thromboembolism in cancer patients: ESMO clinical recommendations. Ann Oncol 2008; 19Suppl. 2: ii126–7
Samama MM, Cohen AT, Darmon JY, et al. A comparison of enoxaparin with placebo for the prevention of venous thromboembolism in acutely ill medical patients. Prophylaxis in Medical Patients with Enoxaparin Study Group. N Engl J Med 1999; 341: 793–800
Leizorovicz A, Cohen AT, Turpie AG, et al. Randomized, placebo-controlled trial of dalteparin for the prevention of venous thromboembolism in acutely ill medical patients. Circulation 2004; 110: 874–9
Cohen AT, Davidson BL, Gallus AS, et al. Efficacy and safety of fondaparinux for the prevention of venous thromboembolism in older acute medical patients: randomised placebo controlled trial. BMJ 2006; 332: 325–9
Mismetti P, Laporte-Simitsidis S, Tardy B, et al. Prevention of venous thromboembolism in internal medicine with unfractionated or low-molecular-weight heparins: a metaanalysis of randomised clinical trials. Thromb Haemost 2000; 83: 14–9
ENOXACAN Study Group. Efficacy and safety of enoxaparin versus unfractionated heparin for prevention of deep vein thrombosis in elective cancer surgery: a double-blind randomized multicentre trial with venographic assessment. Br J Surg 1997; 84: 1099–103
Bergqvist D, Burmark US, Flordal PA, et al. Low molecular weight heparin started before surgery as prophylaxis against deep vein thrombosis: 2500 versus 5000 XaI units in 2070 patients. Br J Surg 1995; 82: 496–501
McLeod RS, Geerts WH, Sniderman KW, et al. Subcutaneous heparin versus low-molecular-weight heparin as thromboprophylaxis in patients undergoing colorectal surgery: results of the Canadian Colorectal DVT Prophylaxis Trial. A randomized, double-blind trial. Ann Surg 2001; 233: 438–44
Bergqvist D, Agnelli G, Cohen AT, et al. Duration of prophylaxis against venous thromboembolism with enoxaparin after surgery for cancer. N Engl J Med 2002; 346: 975–80
Rasmussen MS, Jorgensen LN, Wille-Jorgensen P, et al. Prolonged prophylaxis with dalteparin to prevent late thromboembolic complications in patients undergoing major abdominal surgery: a multicenter randomized openlabel study. J Thromb Haemost 2006; 4: 2384–90
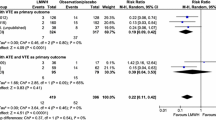
Kuderer NM, Khorana AA, Lyman GH, et al. A metaanalysis and systematic review of the efficacy and safety of anticoagulants as cancer treatment: impact on survival and bleeding complications. Cancer 2007; 110: 1149–61
Tsai AW, Cushman M, Rosamond WD, et al. Coagulation factors, inflammation markers, and venous thromboembolism: the Longitudinal Investigation of Thromboembolism Etiology (LITE). Am J Med 2002; 113: 636–42
Deitcher SR, Kessler CM, Merli G, et al. Secondary prevention of venous thromboembolic events in patients with active cancer: enoxaparin alone versus initial enoxaparin followed by warfarin for a 180-day period. Clin Appl Thromb Hemost 2006; 12: 389–96
Hull RD, Pineo GF, Brant RF, et al. Long-term low-molecular-weight heparin versus usual care in proximal-vein thrombosis patients with cancer. Am J Med 2006; 119: 1062–72
Meyer G, Marjanovic Z, Valcke J, et al. Comparison of low-molecular-weight heparin and warfarin for the secondary prevention of venous thromboembolism in patients with cancer: a randomized controlled study. Arch Intern Med 2002; 162: 1729–35
Cohen AT, Tapson VF, Bergmann JF, et al. Venous thromboembolism risk and prophylaxis in the acute hospital care setting (ENDORSE study): a multinational cross-sectional study. Lancet 2008; 371: 387–94
Mandala M, Barni S, Floriani I, et al. Incidence and clinical implications of venous thromboembolism in advanced colorectal cancer patients: the ‘GISCAD-alternating schedule’ study findings. Eur J Cancer 2009; 45: 65–73
Acknowledgements
We thank Monique Curran of Wolters Kluwer Health Medical Communications who provided assistance with technical revisions after peer review. This assistance was provided on behalf of Rovi Pharmaceuticals, Spain. Parhan Khosravi-Shahi and Gumersindo Pérez-Manga have received honoraria for presentations from Rovi Pharmaceuticals.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Khosravi-Shahi, P., Pérez-Manga, G. International Recommendations for the Prevention and Treatment of Venous Thromboembolism Associated with Cancer. Clin. Drug Investig. 29, 625–633 (2009). https://doi.org/10.2165/11315310-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11315310-000000000-00000