En
Abstract
Objective: This study was designed to investigate the haemodynamic response and pharmacokinetics of a low-dose propofol continuous infusion in providing sedation in patients who required mechanical ventilation after coronary artery bypass grafting surgery.
Patients: 22 male patients, aged between 45 and 65 years, were evaluated in an open, uncontrolled study.
Interventions: At the end of the surgical procedure, a low-dose (1 mg/kg/h) propofol infusion was started and adjusted to optimise sedation according to the Ramsay scale. The mean propofol infusion rate was 1.42 ± 0.4 mg/kg/h.
Main Outcome Measures: Electrocardiogram, systemic and pulmonary arterial pressure, and central venous pressure were monitored continuously. Left ventricular shortening fraction was calculated by transoesophageal echocardiography. Propofol plasma levels were calculated in 10 patients to evaluate the pharmacokinetics.
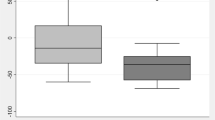
Results: Throughout the duration of the study all patients were haemodynamically stable. Sedation was maintained for 363 ± 244 minutes and was adequate in all patients. The clinical recovery time (postsedation responsiveness) was 15.7 ± 6.2 minutes, after infusion suspension. There was no correlation between propofol plasma levels or propofol infusion rate and the depth of sedation (respectively, r = 0.39 and r = 0.23), while there was a good correlation (r = 0.62) between propofol infusion rate and plasma levels. Open two-compartment model pharmacokinetics were demonstrated.
Conclusion: Low-dose propofol infusion (1 to 2 mg/kg/h) proved to be well tolerated and effective in maintaining sedation after cardiac surgery. Sedation was quickly obtained without a propofol loading dose; steady-state plasma concentrations of 0.6 to 0.8 mg/L were rapidly achieved. Propofol pharmacokinetics ensure rapid clearance with rapid clinical recovery.
Similar content being viewed by others
References
Mangano DT. Perioperative cardiac morbidity. Anesthesiology 1990; 72: 153–84
Veselis RA, Reinsel RA, Marino P, et al. Propofol in sedative doses is an amnesic agent. Anesthesiology 1991; 75Suppl. 3A: A1023
Cockshott ID. Propofol (’Diprivan’) pharmacokinetics and metabolism — an overview. Postgrad Med J 1985; 61Suppl. 3: 45–50
Coppel DL, Johnston JR. The use of propofol as a total intravenous anaesthetic agent for thoracic surgery. Anaesthesia 1988; 43 Suppl.: 118
Glen JB. Animal studies of the anaesthetic activity of ICI 35868. Br J Anaesth 1980; 52: 731–41
Kox W, Brydon C. Effect of sedation with alfentanil, midazolam or propofol on oxygen transport variables in the critically ill. Br J Anaesth 1990; 65: 278P
Laycock GJA, Alston RP. Propofol during hypothermic cardiopulmonary bypass: effects on haemodynamics and metabolism. J Cardiothorac Anesth 1990; 4Suppl. 3: 105
Morgan M. Post cardiac surgery sedation. J Drug Dev 1989; 2Suppl. 2: 119–24
Ramsay MAE, Savege TM, Simpson BRJ, et al. Controlled sedation with alphaxalone-alphadolone. BMJ 1974; 2: 656–59
Kappagoda CT, Linden RJ. The use of SI units in cardiovascular studies. Cardiovasc Res 1976; 10: 141–8
Plummer GF. Improved method for the determination of propofol in blood by high-performance liquid chromatography with fluorescence detection. J Chromatogr 1987; 421: 171–6
Higgins T. Pro: early extubation is preferable to late extubation in patients following coronary artery surgery. J Cardiothor Vasc Anesth 1992; 6: 488–93
Higgins TL, Yared JP, Estafanous FG, et al. Propofol versus midazolam for intensive care unit sedation after coronary artery bypass grafting. Crit Care Med 1994; 22: 1415–23
Slogoff S, Keats AS. Does perioperative myocardial ischemia lead to postoperative myocardial infarction? Anesthesiology 1985; 62: 107–14
Smith RC, Leung JM, Mangano DT, et al. Postoperative myocardial ischemia in patients undergoing coronary artery bypass graft surgery. Anesthesiology 1991; 74: 464–73
Roekaerts PM, Huygen FJ, de Lange S. Infusion of a propofol versus midazolam for sedation in the intensive care unit following coronary artery surgery. J Cardiothor Vasc Anesth 1993; 7: 142–7
Bion JF, Logan BK, Newman PM, et al. Sedation in intensive care: morphine and renal function. Intensive Care Med 1986; 12(5): 359–65
Coates DP, Monk CR, Prys-Roberts C, et al. Haemodynamic effect of infusions of the emulsion formulation of propofol during nitrous oxide anaesthesia in humans. Anesth Analg 1987; 66: 64–70
Chang K, Davis R. Propofol produces endothelium-independent vasodilation and may act as a Ca2+ channel blocker. Anesth Analg 1993; 76: 24–32
Brüssel T, Theissen JL, Vigfusson G, et al. Haemodynamic effects of propofol and etomidate. Negative inotropic properties of propofol. Anesth Anaig 1989; 68: 35–40
Coetzee A, Fourie P, Coetzee J, et al. Effect of various propofol plasma concentrations on regional myocardial contractility and left ventricular overload. Anesth Analg 1989; 69: 573–83
Lepage J, Pinaud ML, Helias JH, et al. Left ventricular function during propofol and fentanyl anaesthesia in patients with coronary artery disease: assessment with a radionuclide approach. Anesth Analg 1988; 67: 949–55
Park WK, Linch P. Propofol and thiopental depression of myocardial contractility: a comparative study of mechanical and electrophysiologic effects in isolated guinea pig ventricular muscle. Anesth Analg 1992; 74: 395
Sherry KM, Sartain J, Bell JH, et al. Comparison of the use of a propofol infusion in cardiac surgical patients with normal and low cardiac output states. J Cardiothor Vasc Anesth 1995; 4: 368–72
Airaksinen KEJ, Ikäheimo MJ, Takkunen JT. Heart rate after coronary artery bypass grafting. Am J Cardiol 1987; 60: 1395–7
McMurray TJ, Collier PS, Carson IW, et al. Propofol sedation after open heart surgery. A clinical and pharmacokinetic study. Anaesthesia 1990; 45: 322–6
Shafer SL. Advances in propofol pharmacokinetics and pharmacodynamics. J Clin Anesth 1993; 5Suppl. 1: 14S–21S
Ben-Shlomo I, Finger J, Bar-Av E, et al. Propofol and fentanyl act additively for induction of anaesthesia. Anaesthesia 1993; 48: 111–3
Hilton P, Dev VJ, Major E. Intravenous anaesthesia with propofol and alfentanil. The influence of age and weight. Anaesthesia 1986; 41: 640–3
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Sorbara, C., Armellin, G., Bonato, R. et al. Postoperative Sedation with Propofol Infusion. Clin. Drug Investig. 16, 431–439 (1998). https://doi.org/10.2165/00044011-199816060-00003
Published:
Issue Date:
DOI: https://doi.org/10.2165/00044011-199816060-00003