Recent advances in rib fracture fixation
Introduction
Thoracic trauma is the main source of mortality and morbidity in patients with blunt trauma of the trunk. Rib fractures accounted for up to 10% of the total number of traumatic hospitalizations (1-3). Surgical stabilization of rib fractures (SSRF) can avoid rib shortening and displacement, relieve fracture pain, and reduce the risk of nonunion. Importantly, as recognized in much of the relevant literature related to patients with flail chest, it can improve ventilation, while reducing dependence on ventilators and the incidence of complications such as pneumonia, length of stay, mortality, and disability rates (4,5). Traditional SSRF with a large incision has been a controversial approach due to extensive injury and several complications. However, with the recent development of new materials and technologies, SSRF has become relatively simple, and the complications associated with it have been significantly reduced. This paper gives a brief introduction regarding this approach.
Evolution of the surgical approach
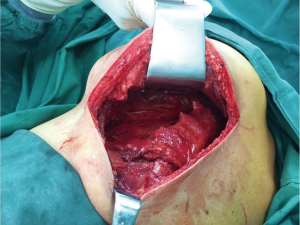
Rib fractures are the most common type of injury and occur in many places, and are mostly seen in patients with chest wall trauma. The chest wall muscles are covered in many layers, which can lead to a traditional posterolateral incision that is good for the exposure of rib fractures but is often a life-altering injury (Figure 1). The choice of incision should be based on the principles of full exposure, minimal injury, and aesthetic appearance, which can make it difficult to unify and standardize the choice of surgical incision. Preoperative fracture location is considered the premise of surgical incision design and the confirmation of treatment options. Generally, the choice of SSRF incision location is based on patient chest signs (concave/dislocated/broken ends) and rough CT measurement. Preoperative CT scanning combined with three-dimensional reconstruction technology can provide visual fracture location, which thus determines the choice of surgical position and incision (Figure 2A). However, there might be still influences of postural changes and subjective judgment. After the actual incision is made, at times it is found that a part of the fracture location is not near the incision that is made, resulting in extended incision. Ultrasound examination further provides more accurate information regarding the incision design, and can also detect the fine fracture and fracture hematoma. Ultrasound examination should be performed after the induction of anesthesia, and then followed by deciding upon the surgical position. The rib fracture is characterized by the discontinuity of rib cortical bone, a sharp fracture line across the rib cortical bone, the interruption of strong echo of rib cortical bone, discontinuity and dislocation in the state of muscle relaxation, and fluctuation of the fracture end (Figure 2B). Preoperative use of ultrasound assists in locating the rib fractures on the body surface and determining the surgical incision for SSRF to accurately locate the fracture. This subsequently reduces surgical trauma of patients, reduces the difficulty of operation, shortens the operative time, and helps the postoperative rehabilitation in patients. Thoracoscopy is also a good method for locating rib fractures in patients with intrathoracic injuries, which requires further thoracoscopic exploration (Figure 2C) (6).

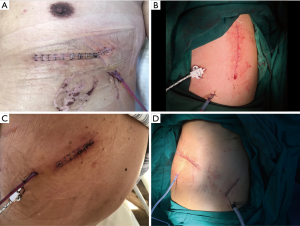
The rib fracture types can be roughly divided into anterior (anterior axillary line), lateral (between anterior axillary line and posterior axillary line), and posterior (posterior axillary line). All these can be accomplished by minimal muscle dissociation or scapular distraction. de Campos and White (7), in their study, described the choice of incision and the technique of muscle protection during exposure in detail. This can be summarized as follows: the patient is placed in supine position to expose the anterior fracture and is exposed through an oblique incision along the submammary fold. The subpectoralis major myocutaneous flaps are then made to expose the anterior ribs 4–6 (Figure 3A). The anterior fracture of the third rib can be exposed through a small transverse incision directly above the fracture, requiring splitting of the pectoralis major and pectoralis minor muscles. When a lateral fracture occurs, the patient should be placed in a lateral decubitus position, and a 7–9 cm longitudinal incision is made along the previous edge of the latissimus dorsi muscle (Figure 3B). After that, the previous edge is sharply dissociated and then the flaps are lifted below the muscles, so that they can be retracted backwards, exposing the muscular branches of the serratus anterior muscle and split muscles to present the rib fractures. Care must be taken to avoid damage to the long thoracic nerve that descends along the anterior axillary line and is present above the serratus anterior muscle. Because of the proximity to the processus transversus, costal angle and subscapularis, the posterior fractures are considered as the most difficult to repair. The patient can take a prone position for these fractures, where the ipsilateral arm is supported on a lower rack of the operating table. This can help in the movement of the scapula outward to expose the deep fracture of the posterior scapula. Then a longitudinal incision is made at the medial end of the scapula to expose the triangle of auscultation (Figure 3C) and the subtrapezius and latissimus dorsi flaps. Patients with multiple rib fractures (flail chest) usually have anterior and posterior fractures or lateral and posterior fractures. Fractures can be exposed by using the above two incisions (Figure 3D). Alternatively, traditional posterolateral thoracotomy can be performed. In short, for less than three adjacent rib fractures in the lateral chest walls, incisions can be made along the direction of ribs, which is conducive to expose the fracture end and reduce the scar formation; for more than three adjacent rib fractures, incisions can be connected by fracture points; for multiple fractures scattered in the fracture site, deep muscular tunnels can be made by separating and retracting muscles to expose the fracture site, and the right angle fixation device can be used for fracture fixation. Multiple small incisions can also be made to selectively fix the unstable fractures.
Evolution of internal fixation materials
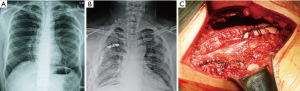
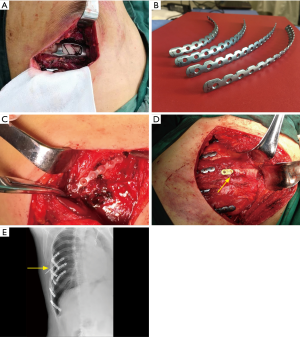
Each of the 12 pairs of ribs present in the human body has its own unique geometric shape (different curvature, uneven thickness), and each also bears about 20,000 breathing exercises every day, making the design of the fracture fixation materials adaptive to this biomechanical challenge (8). Before the advent of rib fixation, thoracic surgeons used anything they could use, such as non-rib steel wires, various bone fracture plates, and other internal fixation materials (Figure 4), which remained significant obstacles to surgery. Without appropriate tools, it is difficult to perform a job proficiently, which is why there has been little enthusiasm for rib fixation for a long time. Now that there are special bone fracture plates and intramedullary fixation devices for rib fixation available, there is no need to use instruments that are not specially designed for ribs. The use of rib internal fixation has spread rapidly. The advantage of a memory alloy embracing device (9) is that it can be fixed immediately and firmly and is relatively cheap. The disadvantage is that it inevitably destroys the blood supply of ribs and damages blood vessels and nerves, leading to poor bone healing and chest pain due to intercostal nerve entrapment or tight sensation at the internal fixation (Figure 5A). Moreover, as the formed products cannot accurately adapt to the curvature of ribs, the fracture of special parts cannot be fixed. It is operatively inconvenient, detaches easily, and stress fractures of the rib plate can occur. Therefore, the bone fracture plate is the mainstream product that is currently used, especially the rib-like internal fixation system which is designed according to the biomechanical characteristics of the rib introduced by Bottlang (10). This is preformed according to the anatomical morphology of the rib. These plates are easy to use for rib fractures from the top to the third rib and from the bottom to the tenth rib. The advantages of these include good biocompatibility, conformity to the physiological curvature of the rib, along with the ability to completely attach to the rib surface, fix on the rib surface without removing the periosteum, avoid injury to the vascular nerve bundles at the lower edge of the rib, fix the fracture end with sufficient length, and match the internal threads between bone fracture plates so that screws cannot be easily prolapsed and displace the implant after locking the screw (Figure 5B). The disadvantage is that the operation requires sufficient operating space. The angle of the screw and bone fracture plate should be maintained at 90 degrees, otherwise the screw may come out. Absorbable polymers such as poly-L-lactic acid plates and rib nails have been successfully used for the fixation of maxillofacial, tibial, and rib fractures, as well as for the rib closure after non-traumatic thoracotomy (11-13) (Figure 5C). These implants have sufficient stiffness to retain their form until the fractures are fully healed, and the absorption rate can slowly transfer the mechanical loads to the skeleton, minimizing the problem of stress shielding while preventing the need for repeated surgical removal. The disadvantage of these is that the use of rib nails is limited for patients with anterior rib fractures or comminuted fractures, narrow ribs, and small bone marrow cavities. Another disadvantage includes an insufficient strength of the rib plate along with the risk of re-fracture, especially posterior rib fracture (14). The main advantage of the intramedullary fixation devices is that it causes relatively small surgical trauma as it makes a relatively small incision, and avoids peeling of the periosteum. At the same time, it is easy to displace the broken end of the fracture and the needle itself, making the operation relatively complex and involving long operative time. Therefore, it has been less often used in clinical practice (Figure 5D,E). At present, there are many kinds of SSRF materials, but each of them has their own shortcomings. The ideal materials should have the following characteristics: good histocompatibility, no rejection reaction, plasticity, the ability to be shaped according to the anatomical shape of the ribs, sufficient strength, and biomechanical elasticity that can meet the elasticity and compliance requirements of the thorax itself and the penetration of radiation, without affecting inspections of other tissues. In the long run, absorbable internal fixation materials are the main direction for future development.
Application of 3D printing technology
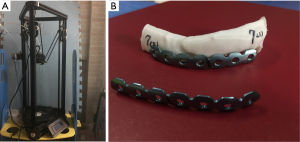
The shape of each rib is different due to the bending and twisting of the rib surface, making it difficult to shape the internal fixation materials for rib fractures. The specific rib fracture sites (parasternal fracture, anterior rib and costal cartilage fracture, paraspinal fracture, fracture of 1, 2, 10–12 ribs), comminuted fractures, and nearly two or more fractures, are difficult to shape. This is because the fixation device should be repeatedly adjusted during the operation, prolonging the operative time, damaging the tissues, and forcing extension of the incision. Failing to fix the ribs or poor adherence of ribs and bone fracture plates results in the removal of internal fixation devices after operation. The intraoperative forced fixation of bone fracture plates and ribs lead to increased stress, and is the main reason for the displacement and removal of bone fracture screws after operation. Surgical programs designed by 3D printing technology before operation, pre-plastic prosthesis, and other measures have been applied in many disciplines (15). According to one study, the error of 3D printing technology ranged between 0.1 and 0.3 mm (16). Zhang et al. (17) reported that the error of cross-sectional data of ribs was less than 0.2 mm, and the accuracy of this model can meet the requirements of clinical application. Establishing anatomical model of ribs by three-dimensional reconstruction technology can accurately reproduce the anatomical shape of the fracture site under in vitro conditions before operation. With this the model, the three-dimensional shaping of the bone fracture plate can be made to improve the suitability of the bone fracture plate to the rib, or the appropriate type of embracing device can be chosen to improve the success rate of operation, shortening the operative time and reducing the probability of internal fixation failure (Figure 6). In the long run, 3D printing technology can be used to make detailed preoperative planning, pre-bending, and tailoring of the internal fixation materials in order to make more precise individualized rib fixation devices.
Evolution of the surgical methods
In the traditional SSRF, only making large incisions can obtain satisfactory exposure results. However, the need to cut off part of the chest wall muscles and nerves (thoracodorsal, long thoracic nerves) and injury to some blood vessels below the incision, causes a high incision infection rate and postoperative scarring in the upper limb, shoulder, while inducing back functional limitation, as well as a long period of chest numbness. However, recent innovations in materials and techniques suitable for SSRF, especially the invention of minimally invasive rib internal fixation tools, have allowed minimally invasive SSRF to become a reality. For internal fixation of the chest wall, thoracoscopic-assisted internal fixation of the chest wall should, in particular, be performed (4,18). For patients in procedures with small surgical incisions, high incision position, insufficient exposure, and poor visual field, thoracoscopy is used as an assistant operation for rib fracture, especially for deep scapular fracture, and can provide a good visual field and aid in thoracic exploration. The basic operation method involves making of a 5–7 cm incision at the center of the fracture or under the scapula, cutting the skin and subcutaneous tissue, dissecting along the muscle gap and muscle texture, separating along the direction of different layers of muscle fibers, protecting the muscle tissue and periosteum as far as possible, and avoiding the transection of the muscle. This method is able to reduce the impact on the formation of fracture callus and fracture healing, reduce surgical trauma and the risk of shoulder and back functional limitation, and relieve postoperative pain (Figure 7). Compared with traditional thoracotomy, thoracoscopic internal fixation of rib fracture has the following advantages: (I) the fracture localization under endoscopy is intuitive and accurate, expanding the fracture fixation range; (II) reduction and fixation of rib fracture under endoscopy can avoid the trauma of intercostal vessels, nerves, and thoracic viscera caused by traditional thoracotomy, reduce complications, and accelerate postoperative recovery; (III) it avoids scapular distraction and eliminates the touchability of the bone fracture plate to the scapula through medial cortical fixation; (IV) it can comprehensively explore and treat intrathoracic injury in the same period, especially some occult injuries; and (V) minimally invasive and aesthetic surgery is easy for patients to accept (19,20). However, there are still several drawbacks to this technique, involving a few limitations and difficulties in adequate reduction and fixation. For example, the reduction and fixation tools are not designed specifically for thoracoscopic approach, leading to difficulty in reduction and prolonged operative time. In addition, the integrity of pleura can be destroyed, resulting in thoracic adhesion and falling off of the plate screw with subsequent intrusion into the thoracic cavity, which remains difficult to remove during reoperation. At present, the preformed bone fracture plate sold in the market is designed according to the outer cortex of the fixed ribs. Theoretically, thoracoscopic SSRF technology will lead to widespread adoption due to its smaller incision, better observation of intrathoracic structure, reduced pain after operation, and faster recovery.

In conclusion, the rapid development of SSRF has been recognized by more and more thoracic surgeons and traumatologists. With the advent of this, new internal fixation materials and techniques are constantly emerging. Minimally invasive surgical techniques and absorbable internal fixation materials are opening as the major avenues of future medical innovation.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Michelitsch C, Acklin YP, Hässig G, et al. Operative Stabilization of Chest Wall Trauma: Single-Center Report of Initial Management and Long-Term Outcome. World J Surg 2018;42:3918-26. [Crossref] [PubMed]
- Ziegler DW, Agarwal NN. The morbidity and mortality of rib fractures. J Trauma 1994;37:975-9. [Crossref] [PubMed]
- Lafferty PM, Anavian J, Will RE, et al. Operative treatment of chest wall injuries: indications, technique, and outcomes. J Bone Joint Surg Am 2011;93:97-110. [Crossref] [PubMed]
- Fraser SF, Tan C, Kuppusamy MK, et al. The role of a video-assisted thoracic approach for rib fixation. Eur J Trauma Emerg Surg 2017;43:185-90. [Crossref] [PubMed]
- Solberg BD, Moon CN, Nissim AA, et al. Treatment of chest wall implosion injuries without thoracotomy: technique and clinical outcomes. J Trauma 2009;67:8-13; discussion 13. [Crossref] [PubMed]
- Tarng YW, Liu YY, Huang FD, et al. The surgical stabilization of multiple rib fractures using titanium elastic nail in blunt chest trauma with acute respiratory failure. Surg Endosc 2016;30:388-95. [Crossref] [PubMed]
- de Campos JRM, White TW. Chest wall stabilization in trauma patients: why, when, and how? J Thorac Dis 2018;10:S951-S962. [Crossref] [PubMed]
- Mohr M, Abrams E, Engel C, et al. Geometry of human ribs pertinent to orthopedic chest-wall reconstruction. J Biomech 2007;40:1310-7. [Crossref] [PubMed]
- Song J, Yan T, Wang T, et al. Internal fixation of claw-type rib bone plates on multiple fractured ribs. Int J Clin Exp Med 2017;10:6934-41.
- Bottlang M, Walleser S, Noll M, et al. Biomechanical rationale and evaluation of an implant system for rib fracture fixation. Eur J Trauma Emerg Surg 2010;36:417-26. [Crossref] [PubMed]
- Chai X, Lin Q, Ruan Z, et al. The clinical application of absorbable intramedullary nail and claw plate on treating multiple rib fractures. Minerva Chir 2013;68:415-20. [PubMed]
- Tatsumi A, Kanemitsu N, Nakamura T, et al. Bioabsorbable poly-L-lactide costal coaptation pins and their clinical application in thoracotomy. Ann Thorac Surg 1999;67:765-8. [Crossref] [PubMed]
- Ito T, Kudo M, Yozu R. Usefulness of Osteosynthesis Device Made of Hydroxyapatite-Poly-L-Lactide Composites in Port-Access Cardiac Surgery. Ann Thorac Surg 2008;86:1905-8. [Crossref] [PubMed]
- Marasco SF, Sutalo ID, Bui AV. Mode of failure of rib fixation with absorbable plates: a clinical and numerical modeling study. J Trauma 2010;68:1225-33. [Crossref] [PubMed]
- The utility of 3D printing for surgical planning and patient-specific implant design for complex spinal pathologies: case report. J Neurosurg Spine 2017;26:513-8. [Crossref] [PubMed]
- Tan ET, Ling JM, Dinesh SK. The feasibility of producing patient-specific acrylic cranioplasty implants with a low-cost 3D printer. J Neurosurg 2016;124:1531-7. [Crossref] [PubMed]
- Song L, Zhang Q, Ning SA, et al. The utility of 3D printing for implant design for rib fracture fixation. Chin J Thorac Cardiovasc Surg 2018;34:288-91.
- Xia H, Zhu P, Li J, et al. Thoracoscope combined with internal support system of chest wall in open reduction and internal fixation for multiple rib fractures. Exp Ther Med 2018;16:4650-4. [PubMed]
- Ren MM, Kong FY, Yang B, et al. Comparison of video-assisted thoracoscopic surgery and traditional thoracotomy for treatment of multiple rib fractures. Chin J Trauma 2014;30:512-5.
- Ren ZL, Ren XP, Zhang Y, et al. Clinical effect of single hole thoracoscope combined with encircling bone plate for treatment of multiple rib fractures. Chin J Thorac Surg 2018;5:180-3. (Electronic Edition).