
General patient satisfaction after elective and acute thoracic surgery is associated with postoperative complications
Introduction
In medicine and particularly in surgery, there is great emphasis on clinical outcomes as markers of the quality of healthcare services. Risk-adjusted morbidity and mortality rates are often used as key indicators of service providers’ performance. These measures are easily monitored and can be used by both individual surgeons as well as collective units to evaluate specific clinical outcomes. However, over the past 30 years, there has been a significant move towards using patient satisfaction and other patient-reported outcomes measures (PROMs) to evaluate and determine both inpatient and outpatient quality of care (1).
Whilst evaluating surgical outcomes will always be necessary, they are not the only factors influencing patients’ appraisal of the quality of care they receive as inpatients. The “National Health Service (NHS) Management Inquiry’s” call for the ‘collation of user opinion’ (2) was the first initiative for patient satisfaction to be used as a metric of quality of healthcare in Britain. However, it is suggested that the origins of this concept are found in consumer healthcare, whereby high satisfaction is necessary in order to retain the patient base and expand it (3).
Patient satisfaction can be defined as an “individual’s cognitive evaluation of, and emotional reaction to, his or her healthcare experience” (4). Steering away from paternalism in medicine, the importance of patients’ views in evaluating quality of care has gained great emphasis given the move towards a more holistic, patient-centred way of viewing health and illness. However, patient satisfaction is not a discrete measure like morbidity or post-operative complications. It is by definition more closely linked to patients’ emotional appraisal of the care received, and given the number of factors that may influence it, it has been historically more difficult to evaluate and interpret (2). Patients’ subjective perception on the quality of their care can shape adherence to post-operative advice, treatments, and has been implicated in better patient-doctor communications for symptom identification and management (5,6). Additionally, as it is a non-clinical indicator, it does not necessarily correlate with the clinical outcome measures that surgeons typically use (7,8) and has not been associated to patient-reported quality of life (9) in other surgical settings.
Therefore, it is a complementary method for reviewing care services, with implications on patients’ continuous engagement with their care, quality of patient-clinician interactions, and patient-reported outcomes. However, in many countries, organisations are using satisfaction data as a means to assign budgets. The ‘Hospital Consumer Assessment of Healthcare Providers and Systems Survey’ is used in USA to allocate financial incentives (10).
Acknowledging the increasing role of this metric in evaluating the performance of our medical and healthcare activities, we aimed to evaluate the satisfaction with care of patients following admission for elective and acute thoracic surgical procedures at a large UK University Hospital, through the use of the validated European Organization for Research and Treatment of Cancer (EORTC) IN-PATSAT32 questionnaire. Specifically, the study aimed to identify potential factors that may influence patients’ appraisal of their healthcare following surgery, expanding a previous evaluation limited to lung cancer patients (11).
Methods
Study design
This cross-sectional pilot study explores the factors that may influence inpatient satisfaction with care, regardless of their disease, following referral for thoracic surgery in our surgical unit. Over two months (July and August 2016) we consecutively recruited all patients who were admitted for surgical intervention in our Thoracic Surgery Department.
Patients’ satisfaction assessment
The EORTC IN-PATSAT32 module was used to assess self-reported satisfaction with inpatient care. It is cross-culturally validated (12) and was delivered to patients on their date of discharge by their nursing team. This patient satisfaction module contains 32 items rated on a 5-point Likert scale, rating the quality of care as ‘poor’, ‘fair’, ‘good’, ‘very good’, ‘excellent’. Ratings are numerically coded as scores between 0 and 100 within 14 different scales (Table 1). Each scale evaluates a certain aspect of inpatient satisfaction (e.g., clinician information provision, nurse technological skill, etc.). We explored each of these aspects but for the purpose of this pilot we particularly focused on the differences in the general satisfaction scale based on demographic (i.e., age, sex, living area) and clinical factors (i.e., presence of complications, type of surgery, length of stay, presence of malignancy).
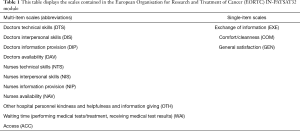
Full table
Ethical decisions and rationale
All participants in this study provided written informed consent. The Leeds Teaching Hospitals Trust Research & Innovation department approved this as service evaluation project and hence approval from the local research ethics committee was not required. However, the study was undertaken in line with the DPA (Data Protection Act) (13) and GCP guidelines (14).
Participant selection
The Department of Thoracic Surgery at the University Hospital is a tertiary referral centre, performing elective operations and acute cases. The questionnaire was administered to all consecutive patients admitted to the thoracic ward within 2 months of their discharge. Following informed consent, relevant clinical information (age, gender, cancer diagnosis, type of admission-acute or electives, length of stay, urban or rural residency) was extracted from the patients’ medical records by members of their clinical team. All clinical and self-reported data was anonymised and investigators were blinded to the identity of the patients.
Patients were included in the study if they had undergone a surgical operation within the Department. At discharge, informed written consent was gained from patients and they then subsequently completed the questionnaire before leaving the hospital. A dedicated nurse was available on the ward for clarification of any study-related information.
Data governance
In order to protect patient confidentiality, any information that contained patient identifiable data was secured in a locked cabinet with restricted access. The key was stored in a code-locked safe and any digital information was protected by password and end-to-end encryption. Direct patient identifiable information was removed after consent and the NHS numbers of patients were used to gather further clinical information. Once this was complete, NHS numbers were also removed from our data.
Data analysis
Data analysis was pursued using STATA 15.0 software (Stata Corp. College Station, TX). Patient demographic, clinical characteristics, surgical outcomes, and satisfaction with care were first summarised descriptively. Patient satisfaction was explored for each group of demographic [age, sex (male/female), living area (urban/rural)] and clinical variables [type of disease (malignant/benign), type of surgery (elective/acute), complications (absent/present) and length of inpatient stay in days]. For the purpose of this study, the following cardiopulmonary complications were taken into account and defined according to the definition provided by the ESTS database: pneumonia, atelectasis requiring bronchoscopy, adult respiratory distress syndrome, mechanical ventilation longer than 24 h, pulmonary oedema, pulmonary embolism, myocardial ischaemia, cardiac failure, arrhythmia, stroke and acute renal insufficiency (15).
As the outcome variable was not normally distributed, between group differences were explored using non-parametric Mann Whitney U tests. To determine the potential contribution of each of these variables to the variation in inpatient satisfaction, as a continuous outcome, we performed multivariable regressions with a backward elimination procedure (P<0.10).
Results
Demographic data
Seventy-five patients were asked to participate to the study, and 52 (69.3%) consented and returned the questionnaire. Missing items were treated according to the EORTC Scoring Manual (16). We present the demographic and clinical characteristics for the 52 patients included in this study (Table 2). Patients had a mean age of 58 (sd =16.7), 27 were males (52%), and 38 reported living in urban areas (73%). Patients’ post-operative length of stay (LOS) was on average 4.9 days (sd =3.8). Thirty-five (67%) patients had surgery for a malignant disease, 41 procedures (79%) were performed electively, and thirteen (25%) patients experienced any post-operative complications.
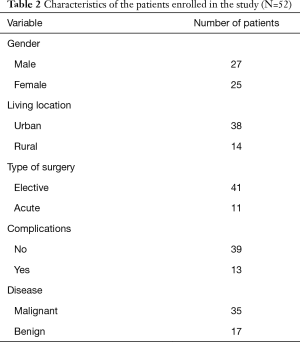
Full table
The average patient satisfaction score was 73.08 (sd =23.05) (see Table 3). Patients rated most areas of satisfaction highly (>80 satisfaction), including doctors’ and nurses’ technical skills, but offered lower scores for environment comfort and cleanliness (mean =68.85, sd =24.57).

Full table
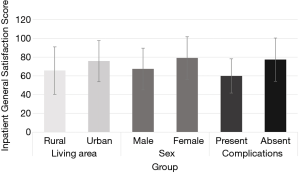
We focused our analyses on the general satisfaction with care scale to explore differences according to demographic and clinical factors (Figure 1). General satisfaction with care differed between sexes (U=231, P=0.04) and depending on the presence of post-operative complications (U=128.5, P=0.006). Satisfaction with care was lower in males (mean =67.4; sd =22.3) compared to females (mean =22.7, sd =22.7) and in patients with complications (mean =60, sd =18.26) versus those without (mean =77.4, sd =23.03). Patients’ satisfaction did not differ depending on patients’ age, type of surgical procedure, diagnosis, or LOS.
Finally, we explored which factors may explain the largest amount of variance in general satisfaction (Table 4). Our regression model revealed that 22% of the variance in general inpatient satisfaction (P=0.006) was explained by the presence of complications (Coef =−19.02, P=0.007), and marginally by sex (Coef =−10.75, P=0.071) and living area (Coef =12.10, P=0.074). Patients with and without complications differed in most of the other scales of the EORTC IN-PASAT32 (see Table 5).

Full table
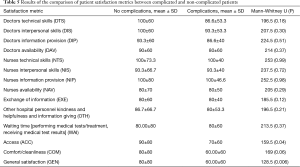
Full table
Discussion
The main finding of our study was the association between the occurrence of post-operative complications and a worse patient satisfaction with care. It can then be considered that these results reflect the importance of health status for the patient. For the individual patient, an indication of whether the intervention has cured the initial problem has the greatest bearing on how satisfied they are with their care. This was particularly the case for male patients and patients from rural backgrounds, as evidenced by our regression model whereby complications, sex, and living area best explained the variation in satisfaction with care.
Pompili et al. alternatively found no correlation between complications and satisfaction (11), particularly in patients with lengthy hospital stays. They suggested that these results could be attributed to the fact that patients who experience adverse events post-surgery consequently will often receive more attention and intense care, over longer periods of time, from both medical and nursing staff. This in turn could make the patient feel more valued, more reassured, additional information shaping recovery expectations may be offered, which may result in a higher level of satisfaction. One explanation can be that complications in acute patients, who did not expect and were not prepared for lengthier hospital admissions, may have contributed to lower levels of inpatient satisfaction. The main difference between these two papers in fact, not only the time of assessment but also the population, including also trauma/acute patients.
The findings presented here are similar to those of Di Cristofaro et al., who assessed patient satisfaction after surgery for colorectal cancer (17). The authors suggested that greater emphasis needs to be placed on communicating the potential risk of surgery, so that the doctor-patient relationships are not impaired when complications occur. Barlesi et al., who similarly studied satisfaction in a thoracic surgery department, found the same significant association with post-operative complications (18). Whilst patients may perceive that post-operative complications correlate with poor surgical technique or perioperative care, this may not be the case when traditional physician driven-endpoints are assessed. This has important implications as quality of care as perceived by patients may differ from the one judged by clinicians and appropriate communication of surgical expectations, recovery, and duration or severity of complications is warranted. Importantly, in this study, the presence of complications did not correlate with a perception of a poorer standard of care from clinicians or nurses.
As we know, surgical complications are highly variable and their presence can greatly impact the recovery of a patient (19). A meta-analysis of 50 studies found that two-thirds described a negative association between complications and psycho-social wellbeing in the post-operative period. Interestingly, they also suggested that the severity of complications does not always indicate how seriously patients will be affected by them. Whilst not all patients who suffer post-operative complications will report lower care satisfaction, it is clear that the latter are at higher risk of having poorer outcomes.
An interesting line of argument that could be drawn from this study is whether patient satisfaction is associated with quality of surgical care. A study of 180 US hospitals found that patients in the highest quartile of patient satisfaction had significantly lower risk-adjusted odds ratio of death, failure to rescue (death after complication) and minor complications (20). However, opposing these findings, Barlesi et al. found no significant correlation between quality of care and satisfaction (18). Literature therefore seems to be divided on whether there is an association between patient satisfaction with care and the quality and efficiency of healthcare received. However, these differences may also due to how quality and efficiency of care are measured between studies. Here we focused on a crucial element of patient safety, namely post-operative complications as an objective indicator of surgical care. Following from previous authors’ suggestions that patient satisfaction should be ‘integrated-into rather than substituted-for quality of health care assessment’ (21), we evidenced that post-operative complications are associated with satisfaction with care in a heterogeneous group of thoracic patients.
Limitations
This study was designed as a 2-month service evaluation, hence it was limited in its sample size and potentially not representative of the general population operated in a thoracic surgical department.
The questionnaire was limited in its scope as a cancer-specific questionnaire, which may not be representative of patients who have undergone thoracic surgery for other pathology and acutely referred patients. Nonetheless, the individual questionnaire items refer to patients’ perception of the skills of the medical staff, satisfaction with information provided as well as environment of their inpatient stay, which are common across diagnoses.
This was a pilot study using a validated inpatient satisfaction questionnaire in a cohort of thoracic surgical patients. The questionnaire does not include open ended questions for patients to provide additional insight into their quality of care. This may have reduced the amount of information to which we had access, failing to provide a more comprehensive picture as to why patients may have felt dissatisfied. However, within this study we did not set out to explore additional factors which may have influenced patients’ satisfaction over and above demographic and clinical variables routinely collected. Our findings motivate future purposively sampled qualitative explorations of potential sources of dissatisfaction with inpatient care in particular demographic and clinical groups.
Our service evaluation focused on the patients’ short-term rather than long-term surgical follow-up. A comparative evaluation at six-months to one-year post-operatively may offer insight into changes in satisfaction and complications over time, having the additional benefit of a lower social desirability bias, a confounding variable which the participants of this study could have experienced during their admission.
Nonetheless, this is a pilot study in an area warranting additional investigation at a local and national levels—surgical inpatient satisfaction. For this to be feasible, the use of the EORTC standardised patient satisfaction measurement ensures the reliability of our study and can enable its replication in larger, longitudinal cohorts for the development of large-scale recommendations and service developments. Exploring the variation in surgical inpatient services, level of information provided pre-and-post surgery to various groups and the different patient groups’ need for information may offer insight as to the usefulness of patient satisfaction measures and factors influencing this metric.
Conclusions
In this heterogeneous group of thoracic patients, the absence of post-operative complications was significantly associated with increased general patient satisfaction. Patient satisfaction will not always align with quality of surgical care but does relate to poor outcomes. Patient satisfaction can be influenced by a huge number of factors, some of which may be more difficult to identify and measure. However, if we can understand patients’ sources of dissatisfaction with their care, we can more easily stratify improvement initiatives to patient groups and services where they are most needed. Therefore healthcare professionals should be aware that satisfaction with care is closely related to patients’ complications in the short term; whilst all patients deserve a high level of care, particular focus should be given to supporting patients and managing expectations along the post-operative period.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd-19-3345b). GV reports personal fees from Roche, personal fees from Eisai, personal fees from Novartis, grants from Pfizer, grants from Breast Cancer NOW, grants from Yorkshire Cancer Research, grants from EORTC, outside the submitted work. AB serves as an unpaid editorial board member of from Dec 2019 to Nov 2021. CP serves as an unpaid editorial board member of from Sep 2018 to Aug 2020. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The Leeds Teaching Hospitals Trust Research & Innovation department approved this as service evaluation project and hence approval from the local research ethics committee was not required. All participants in this study provided written informed consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Velikova G, Coens C, Efficace F, et al. Health-Related Quality of Life in EORTC clinical trials — 30 years of progress from methodological developments to making a real impact on oncology practice. EJC Suppl 2012;10:141-9. [Crossref]
- Williams B, Coyle J, Healy D. The meaning of patient satisfaction: an explanation of high reported levels. Soc Sci Med 1998;47:1351-9. [Crossref] [PubMed]
- Sitzia J, Wood N. Patient satisfaction: a review of issues and concepts. Soc Sci Med 1997;45:1829-43. [Crossref] [PubMed]
- Shirley ED, Sanders JO. Patient satisfaction: Implications and predictors of success. J Bone Joint Surg Am 2013;95:e69. [Crossref] [PubMed]
- Martin LR, Williams SL, Haskard KB, et al. The challenge of patient adherence. Ther Clin Risk Manag 2005;1:189-99. [PubMed]
- Finefrock D, Patel S, Zodda D, et al. Patient-Centered Communication Behaviors That Correlate With Higher Patient Satisfaction Scores. J Patient Exp 2018;5:231-5. [Crossref] [PubMed]
- Brunelli A, Rocco G. Clinical and nonclinical indicators of performance in thoracic surgery. Thorac Surg Clin 2007;17:369-77. [Crossref] [PubMed]
- Rocco G, Brunelli A. Patients' satisfaction: customer relationship management as a new opportunity for quality improvement in thoracic surgery. Thorac Surg Clin 2012;22:551-5. [Crossref] [PubMed]
- Avery KN, Metcalfe C, Nicklin J, et al. Satisfaction with care: an independent outcome measure in surgical oncology. Ann Surg Oncol 2006;13:817-22. [Crossref] [PubMed]
- Tsai TC, Orav EJ, Jha AK. Patient satisfaction and quality of surgical care in US hospitals. Ann Surg 2015;261:2-8. [Crossref] [PubMed]
- Pompili C, Tiberi M, Salati M, et al. Patient satisfaction with health-care professionals and structure is not affected by longer hospital stay and complications after lung resection: a case-matched analysis. Interact Cardiovasc Thorac Surg 2015;20:236-41. [Crossref] [PubMed]
- Bredart A, Bottomley A, Blazeby JM, et al. An international prospective study of the EORTC cancer in-patient satisfaction with care measure (EORTC IN-PATSAT32). Eur J Cancer 2005;41:2120-31. [Crossref] [PubMed]
- Boyd P. The requirements of the Data Protection Act 1998 for the processing of medical data. J Med Ethics 2003;29:34-5. [Crossref] [PubMed]
- Switula DJS, Ethics E. Principles of good clinical practice (GCP) in clinical research. Sci Eng Ethics 2000;6:71-7. [Crossref] [PubMed]
- Fernandez FG, Falcoz PE, Kozower BD, et al. The Society of Thoracic Surgeons and the European Society of Thoracic Surgeons general thoracic surgery databases: joint standardization of variable definitions and terminology. Ann Thorac Surg 2015;99:368-76. [Crossref] [PubMed]
- Fayers PM, Aaronson NK, Bjordal K, et al. The EORTC QLQ-C30 Scoring Manual (3rd Edition). 2001.
- Di Cristofaro L, Ruffolo C, Pinto E, et al. Complications after surgery for colorectal cancer affect quality of life and surgeon-patient relationship. Colorectal Dis 2014;16:O407-19. [Crossref] [PubMed]
- Barlesi F, Boyer L, Doddoli C, et al. The place of patient satisfaction in quality assessment of lung cancer thoracic surgery. Chest 2005;128:3475-81. [Crossref] [PubMed]
- Pinto A, Faiz O, Davis R, et al. Surgical complications and their impact on patients' psychosocial well-being: a systematic review and meta-analysis. BMJ Open 2016;6:e007224. [Crossref] [PubMed]
- Sacks GD, Lawson EH, Dawes AJ, et al. Relationship Between Hospital Performance on a Patient Satisfaction Survey and Surgical Quality. JAMA Surg 2015;150:858-64. [Crossref] [PubMed]
- Chow A, Mayer EK, Darzi AW, et al. Patient-reported outcome measures: The importance of patient satisfaction in surgery. Surgery 2009;146:435-43. [Crossref] [PubMed]


