Multiportal video-assisted thoracic surgery, uniportal video-assisted thoracic surgery and minimally invasive open chest surgery—selection criteria
Introduction
Thoracic surgery has evolved continuously into a less invasive approach. As a result of this continuous progress, various techniques have been developed, which allow performing safe and effective procedures with minimal trauma to the patient. The first steps were taken by Jacobeus over 100 years ago, performing these types of surgeries mainly for diagnostic purposes (1). For many decades, a minimally invasive approach was selected only for minor procedures and it wasn’t until the early 90s that video assisted thoracic surgery was developed and used to perform major pulmonary resections (2).
Since then, the speed of evolution for this technique has increased significantly, pushed by thoracic surgeons in search for a less invasive approach and technological advances, providing better instruments, cameras, and hemostatic devices that make this process more manageable for all involved (3).
Minimally invasive thoracic surgery (MITS) can be divided into two major groups: minimally invasive open chest surgery [mini thoracotomy, hybrid video-assisted thoracic surgery (VATS)] and pure video assisted thoracic surgery (multiportal and uniportal VATS).
Nowadays, it is not a matter about if a minimally invasive approach is better for patients but rather about which approach to choose to offer the optimal care for every patient. Each approach has its own benefits and which to select must be tailored to the surgeon, patient and disease.
VATS is no longer a novelty or a trend, it is well-established and possibly the standard of care for many thoracic diseases requiring surgery. It has been proven that it enhances recovery, reduces pain (4), minimizes postoperative complications, and shortens the length of hospital stays (5).
Currently, the thoracic surgeon should be able to train for and adopt a VATS approach and the question that is going to be faced is which VATS approach should be adopted. Should it be dealt in a step wise manner beginning with mini thoracotomy, hybrid VATS and then develop a pure VATS approach, starting with three port VATS and progressing through until finally arriving to a uniportal approach? Or should the surgeon select any of the approaches from the beginning and train to perfect it?
The purpose of this article is to evaluate the different techniques available for minimally invasive thoracic surgery and the different factors that surgeons should consider in the process of developing any of them.
Minimally invasive open chest surgery
Muscle sparring thoracotomy (MST) and hybrid VATS (combines muscle sparring thoracotomy and video assistance) can be included in this group. Both are performed with some degree of rib spreading, representing the major difference with pure VATS. Varying criteria exists regarding the length of a mini thoracotomy, but it is usually between 4 and 10 cm. Some authors even suggest that incisions larger than 6cm, without rib spreading, should be considered an open procedure or a hybrid VATS (6).
In MST, surgery is performed with direct visualization and dissection is done directly through the incision, allowing for direct palpation of the tissues. It offers the advantage of a smaller incision and, perhaps, it serves as a good transition procedure for the surgeon beginning the path to minimally invasive surgery, but his majority of cases are still being performed through a posterolateral thoracotomy.
Hybrid VATS, a term describe by Okada, combines direct and thoracoscopic visualization and allows hand maneuvering dissection (7). It serves as an option when complex cases are challenging for pure VATS or for those where surgeon is not comfortable with a VATS approach, such as large tumors, fused lymph nodes at the hilum or diffuse, thick adhesions.
One of the benefits of these techniques is that it can be used as a bridge from conventional thoracotomy to VATS surgery, allowing the surgeon to get used to working in a smaller surgical field and thoracoscopic visualization without losing direct hand dissection. The contrary also applies, as they can be used as conversion techniques for VATS procedures that result technically challenging.
The key benefit of these techniques is that the surgeon is able to directly palpate the structures, which results very useful in cases of lymph nodes fused to vascular structures, lung cancer with prior neoadjuvant therapy or tuberculosis, in which the dissection plane is difficult to find and sometimes can only be “felt” in order to find it.
Both serve as a good choice for centers with a restricted budget, as almost all the procedure is completed through manual maneuvering (dissection, ligation, suturing), hence the need of surgical staplers, and clips is usually avoided, significantly reducing costs. (8)
Both, MST and Hybrid VATS can be selected by surgeons starting their path in minimally invasive surgery and have a strong background in open surgery, allowing a friendlier transition. Bronchial and vessel suturing are technically less demanding through this approach, which could make it preferable for surgeons without extended experience in VATS suturing in high-volume centers.
Video assisted thoracic surgery
Procedures in this group are performed through one (single port VATS) or multiple incisions (multiport VATS), but all of them are completed without rib spreading and visualization is done only with the thoracoscope. Different VATS techniques can be used for surgery of similar conditions and it is up to the surgeon to choose the best suited approach. Additionally, there are other factors that can influence the decision and choice of technique is up to the surgeon’s discretion.
Surgeon-related factors
At the present time, many active thoracic surgeons have a strong background in open surgery procedures prior to starting with VATS approaches. Nonetheless, as time passes by and VATS becomes the standard approach for most thoracic conditions, many of the thoracic surgeons will have a stronger background with VATS than with open surgery. This same trend has already occurred in general surgery (9) and it is probably the most likely path in the surgical field, as more advances in technology become more widely available. The familiarity of a surgeon with a certain VATS approaches depends on many factors, but a key factor is the technique used in the center where they complete their residency. The technique surgeons are taught will be the one they will prefer to use in their first solo cases or when facing with complex surgical situations.
Since multiportal VATS has been around for more than 20 years (2,10), it is logical that most thoracic surgeons began their experience with this approach and are more acquainted with this technique. Even the most experienced uniportal surgeons began their journey in minimally invasive surgery with the three and two port technique before progressing to major pulmonary resections with a single port approach (5,11). This is usually the recommended path for surgeons that start a VATS program and it is advisable to gain experience with minor and major procedures with multiport VATS before progressing to uniport techniques.
The increase in experience gained using uniportal VATS around the world has resulted in many surgeons making a direct transition from open surgery to uniportal VATS, showing that prior experience in multiport VATS is not an absolute requirement for surgeons. Some surgeons have experienced an easier transition by progressing directly from open surgery to uniportal VATS, as the approach mimics the hand-eye disposition of open surgery and avoids diamond-based dispositions (12,13).
The learning curve for VATS procedures can differ according to various factors, such as individual skills and the volume of cases handled by the center in which the surgeon is training, but it is suggested that surgeons should perform 100 minor procedures with VATS before attempting major pulmonary resections. For VATS lobectomies, the recommended learning curve is 50 cases (14). To date, no study has been performed to determine the learning curve for uniportal VATS lobectomies, but it is likely to be very similar to the one proposed for conventional VATS. It is very important for any VATS surgeon to participate in courses, wet labs, and train in high volume centers to gain experience and perform VATS surgeries safely and successfully (3,14).
Consequently, the approach selected for each given case will depend entirely on the individual preference of each surgeon and the familiarity, experience, and confidence in performing the procedure that each surgeon has with multiport or uniportal VATS. It is of uppermost importance that the surgeon feels comfortable and confident while performing any VATS, to avoid unnecessary complications or accidents during the procedure.
Uniportal VATS is gaining a lot of popularity among thoracic surgeons around the globe in part due to that the teaching of this technique has been particularly enhanced by the fact that one of the pioneers, Dr. González Rivas, has been willing to travel around the world in an effort to make it available for almost any thoracic surgeon interested in learning the technique.
Disease-related factors
As with every new development in surgery, all techniques must go through a series of steps before becoming a consolidated practice. The first thoracoscopic procedures were only reserve for diagnostic purposes and minor therapeutic surgeries (1,15,16), but as the approach was adopted by different centers and surgical teams around the world, the complexity of cases in which VATS is being use continues to grow and expand, covering the vast majority of thoracic surgical conditions. In present times, multiportal and uniportal VATS has been successfully used to treat benign and malignant conditions, with similar results (17).
Benign conditions
The wide range of benign conditions that can be treated with a VATS approach includes relatively simple procedures, such as pleural biopsies and wedge resection to major anatomic resections.
There are few published studies comparing the results between both techniques, but a best evidence topic by Akter et al. concluded that uniport may offer improved pain scores when compared to multiport approaches, with no difference in length of stay, drainage, or complications (17).
A meta-analysis comparing the approaches only for primary pneumothorax showed shorter length of stay, lower postoperative pain score, less drainage, and lower incidence of postoperative paresthesia in the uniportal group, although conceding the need for large scale and high quality studies for validation of their conclusions (18). In a prospective study Mier et al., also showed a lower pain score when comparing uniportal vs. multiport VATS for minor procedures, although they used SILS device for the uniport approaches (19).
Regarding major lung resections for benign conditions, such as bronchiectasis, aspergilloma, lung sequestration, even fewer reports addressing the result of VATS have been published. A couple of studies published in 2016 showed the VATS lobectomy was feasible and safe for benign conditions, albeit more challenging given the particularities more frequently associated with benign or inflammatory conditions, such as adhesions and hilar and interlobar lymphadenopathy. In both studies, a multiportal approach was used (20,21).
Although benign lymphadenopathy represents a challenging condition, experienced surgeons can perform anatomic dissection of lymph nodes and bronchial and vascular structures safely through a uniport approach (22).
Given the complexity of lobectomy cases that have been published in oncologic conditions having been successfully performed with uniportal VATS, a significant difference in results will not be expected. However, the lacks of studies comparing both approaches limit any conclusion.
For minor procedures, uniportal VATS might be a preferable option, yet for major lung resections for benign conditions, it would depend on the experience of the surgeon with each technique, although VATS is preferable.
Malignant conditions
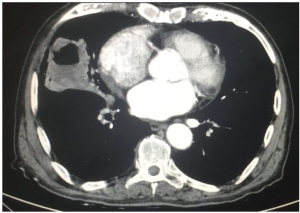
For malignant conditions, avoiding pleural, lung biopsies, and palliative procedures, such as VATS pleurodesis for malignant pleural effusion, the therapeutic procedures are usually complex and involve anatomic lung resections for lung cancer with lymph node dissection (Figure 1).
In the present time, VATS lobectomy is the recommended procedure for early stage lung cancer (23), given the evidence showing better recovery without compromising oncological results (24-26). It took more than a decade for this evidence to be well established for VATS lobectomy, in relation to the gold standard, which was lobectomy by open surgery. Multiportal VATS lobectomy has been successfully performed in early stage lung cancer and in more complex cases involving sleeve lobectomies and carinal reconstruction (27).
Since uniportal VATS is a more recent approach for major pulmonary resections and has only been around for about 5 years, there is still a lot of road to cover in terms of evidence for the approach to prove it is a better option than conventional VATS (28). However, at this time, it has proven to be safe and feasible, and in the hands of expert VATS surgeons can be used reliably for procedures involving complex cases, including bronchial, vascular and carinal reconstruction (29-32). Challenging cases with diffuse pleural adhesions can be completed with excellent visualization and good control during dissection (Figure 2). In terms of safety and feasibility both techniques are well established.
A meta-analysis recently published comparing uniportal vs. multiportal, the first one to meta-analyze clinical outcomes, shows that uniportal VATS was associated with a statistically significant reduction in chest tube drainage, in hospital stay, and overall morbidity (34). These results need to be reproduced by other meta-analysis that include more prospective studies and evaluate the results once the learning curve of uniportal VATS is surpassed in multiple centers around the world.
Thus, regarding the matter of which technique to choose for lung cancer and anatomical resections both have proven to be comparable in their results, and the evidence available is insufficient to declare one option as superior (28).
Stating this, there could be some reasons why a uniportal approach might be preferred. The approach to the target lesion is similar to open surgery, only one intercostal space is involved during the surgery, given at least a cosmetically advantage and reduces the possibility of pain in other intercostal spaces and it seems that the advances in technology are facilitating the performance of the surgeon in this technique (articulated staplers, energy devices for hemostasis and dissection (35) (Figure 3).

Key points:
- Minimally invasive open chest surgery:
- MST and hybrid VATS could help to provide a friendly transition from open surgery to VATS for thoracic surgeons;
- Both techniques represent a good choice for complex cases and center with limited resources.
- ϖ Multiportal and uniportal VATS:
- Available evidence suggests both approaches are acceptable and have similar outcomes;
- Each surgeon should choose the approach that fit them best and always keep in mind that neither is mandatory always, since numerous factors make every operation different.
Future and perspectives
The VATS road is far from ending and continues to improve every day, as the search for a less invasive approaches is always in the horizon. In this sense, the thoracic surgeon needs to be aware of the different techniques available, and after thoughtful consideration choose with path to take. Current evidence suggest that VATS procedures have better results than open surgery in term of patient recovery, postoperative pain and in hospital stay, with similar oncological outcomes. In this scenario, pure VATS approaches tend to have a lead, since future developing in technology will focused on making these techniques more feasible and easier for the thoracic surgeon. Therefore, at least for now, the future seems to be focused on improving minimal invasive surgery and the search for the ideal procedure is far from ending (Figure 4).

Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Jacobaeus H. Über die Möglichkeit die Zystoskopie bei Untersuchung seröser Höhlungen anzuwenden. Munch Med Wochenschr 1910;57:2.
- Roviaro G, Rebuffat C, Varoli F, et al. Videoendoscopic pulmonary lobectomy for cancer. Surg Laparosc Endosc 1992;2:244-7. [PubMed]
- Gonzalez-Rivas D. Uniporthal thoracoscopic surgery: from medical thoracoscopy to non-intubated uniportal video-assisted major pulmonary resections. Ann Cardiothorac Surg 2016;5:85-91. [Crossref] [PubMed]
- Tamura M, Shimizu Y, Hashizume Y. Pain following thoracoscopic surgery: retrospective analysis between single-incision and three-port video-assisted thoracoscopic surgery. J Cardiothorac Surg 2013;8:153. [Crossref] [PubMed]
- Sihoe AD. The evolution of minimally invasive thoracic surgery: implications for the practice of uniportal thoracoscopic surgery. J Thorac Dis 2014;6:S604-17. [PubMed]
- Migliore M. VATS surgery for anatomical lung resection: a different approach for every surgeon. Videoassist Thorac Surg 2016;1:31. [Crossref]
- Okada M, Sakamoto T, Yuki T, et al. Hybrid surgical approach of video-assisted minithoracotomy for lung cancer: significance of direct visualization on quality of surgery. Chest 2005;128:2696-701. [Crossref] [PubMed]
- Zhu Q, Xiao H, Xu E, et al. From open to single port video-assisted thoracoscopic lobectomy: a stepwise and return progression of the experience from Department of Thoracic Surgery, General Hospital of Guangzhou Military Command of P.L.A. J Thorac Dis 2015;7:1252-63. [PubMed]
- Eckert M, Cudrado D, Steele S, et al. The changing face of the general surgeon: national and local trends in resident operative experience. Am J Surg 2010;199:652-6. [Crossref] [PubMed]
- McKenna RJ Jr, Houck W, Fuller CB. Video-assisted thoracic surgery lobectomy: experience with 1,100 cases. Ann Thorac Surg 2006;81:421-5; discussion 425-6. [Crossref] [PubMed]
- Gonzalez-Rivas D. VATS lobectomy: surgical evolution from conventional VATS to uniportal approach. ScientificWorldJournal 2012;2012:780842.
- Ng CS. Uniportal VATS in Asia. J Thorac Dis 2013;5:S221-S225. [PubMed]
- Anile M, Diso D, Mantovani S, et al. Uniportal video assisted thoracoscopic lobectomy: going directly from open surgery to a single port approach. J Thorac Dis 2014;6:S641-3. [PubMed]
- Petersen RH, Hansen HJ. Learning curve associated with VATS lobectomy. Ann Cardiothorac Surg 2012;1:47-50. [PubMed]
- Gonzalez-Rivas D. Evolving thoracic surgery: from open surgery to single port thoracoscopic surgery and future robotic. Chin J Cancer Res 2013;25:4-6. [PubMed]
- Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. [Crossref] [PubMed]
- Akter F, Routledge T, Toufektzian L, et al. In minor and major thoracic procedures is uniport superior to multiport video-assisted thoracoscopic surgery? Interact Cardiovasc Thorac Surg 2015;20:550-5. [Crossref] [PubMed]
- Xu W, Wang Y, Song J, et al. One-port video-assisted thoracic surgery versus three-port video-assisted thoracic surgery for primary spontaneous pneumothorax: a meta-analysis. Surg Endosc 2017;31:17-24. [Crossref] [PubMed]
- Mier JM, Chavarin A, Izquierdo-vidal C, et al. A prospective study comparing three-port video-assisted thoracoscopy with the single- incision laparoscopic surgery (SILS) port and instruments for the video thoracoscopic approach: a pilot study. Surg Endosc 2013;27:2557-60. [Crossref] [PubMed]
- Reichert M, Kerber S, Pösentrup B, et al. Anatomic lung resections for benign pulmonary diseases by video-assisted thoracoscopic surgery (VATS). Langenbecks Arch Surg 2016;401:867-75. [Crossref] [PubMed]
- Mazzella A, Olland A, Garelli E, et al. Video-assisted thoracoscopic surgery is a safe option for benign lung diseases requiring lobectomy. Surg Endosc 2017;31:1250-6. [Crossref] [PubMed]
- Guido Guerrero W, Gonzalez-Rivas D, Hernandez Arenas LA, et al. Techniques and difficulties dealing with hilar and interlobar benign lymphadenopathy in uniportal VATS. J Vis Surg 2016;2:23.
- Howington JA, Blum MG, Chang AC, et al. Treatment of Stage I and II Non-small Cell Lung Cancer: Diagnosis and Management of Lung Cancer, 3rd ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2013;143:e278S-e313S.
- Alam N, Flores RM. Video-assisted thoracic surgery (VATS) lobectomy: the evidence base. JSLS 2007;11:368-74. [PubMed]
- Rueth NM, Andrade RS. Is VATS lobectomy better: perioperatively, biologically and oncologically? Ann Thorac Surg 2010;89:S2107-11. [Crossref] [PubMed]
- Whitson BA, Groth SS, Duval SJ, et al. Surgery for early-stage non-small cell lung cancer: a systematic review of the video-assisted thoracoscopic surgery versus thoracotomy approaches to lobectomy. Ann Thorac Surg 2008;86:2008-16; discussion 2016-8.
- Li J, Wang W, Jiang L, et al. Video-Assisted Thoracic Surgery Resection and Reconstruction of Carina and Trachea for Malignant or Benign Disease in 12 Patients: Three Centers' Experience in China. Ann Thorac Surg 2016;102:295-303. [Crossref] [PubMed]
- Sihoe AD. Reasons not to perform uniportal VATS lobectomy. J Thorac Dis 2016;8:S333-S343. [PubMed]
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Uniportal video-assisted thoracoscopic sleeve lobectomy and other complex resections. J Thorac Dis 2014;6:S674-81. [PubMed]
- Gonzalez-Rivas D, Yang Y, Stupnik T, et al. Uniportal video-assisted thoracoscopic bronchovascular, tracheal and carinal sleeve resections†. Eur J Cardiothorac Surg 2016;49 Suppl 1:i6-16. [PubMed]
- Gonzalez-Rivas D, Delgado M, Fieira E, et al. Doublesleeve uniportal video-assisted thoracoscopic lobectomy 4 for non-small cell lung cancer. Ann Cardiothorac Surg 2014;3:E2. [PubMed]
- Gonzalez-Rivas D, Xie B, Yang Y, Jiang G. Uniportal video-assisted thoracoscopic lobectomy with en bloc chest wall resection. J Vis Surg 2015;1:7.
- Guido Guerrero W, González-Rivas D. Uniportal right upper lobectomy and 6 segmentectomy. Asvide 2017;4:155. Available online: http://www.asvide.com/articles/1460
- Harris CG, James RS, Tian DH, et al. Systematic review and meta-analysis of uniportal versus multiportal video-assisted thoracoscopic lobectomy for lung cancer. Ann Cardiothorac Surg 2016;5:76-84. [Crossref] [PubMed]
- Bertolaccini L, Viti A, Terzi A, Rocco G. Geometric and ergonomic characteristics of the uniportal video-assisted thoracoscopic surgery (VATS) approach. Ann Cardiothorac Surg 2016;5:118-22. [Crossref] [PubMed]
Cite this article as: Guerrero WG, González-Rivas D. Multiportal video-assisted thoracic surgery, uniportal video-assisted thoracic surgery and minimally invasive open chest surgery—selection criteria. J Vis Surg 2017;3:56.


