
Brain abscess caused by Listeria monocytogenes: a case report and literature review
Introduction
Listeria monocytogenes is a unique Listeria species that is frequently pathogenic to humans. Listeria is a facultatively anaerobic, gram-positive rod bacterium (1). L. monocytogenes is an opportunistic food-borne pathogen that is widely distributed in nature and is responsible for listeriosis. The incidence confirmed by laboratory testing was 0.29 cases/100,000 population in the U.S. from 2009 to 2011 (2). Brain infection (meningitis and meningoencephalitis) and bacteremia are common clinical manifestations of listeriosis in pregnant women and fetuses as well as in elderly and immunocompromised individuals, but it manifests as self-limiting gastroenteritis in normal hosts. Risk factors affecting the survival and function of macrophages may increase susceptibility to L. monocytogenes in hosts (3). However, brain abscesses occur rarely, in only approximately 10% of patients with Listeria infection of the brain (4). Brain abscess is a further progression of meningoencephalitis. L. monocytogenes may reach the brain parenchyma via capillary endothelial cells, which comprise a single layer of microvascular endothelial cells characterized by tight junctions. On the other hand, infectious macrophages may pass through the endothelium of the middle cerebral artery, resulting in cerebritis or brain abscess formation (5,6). Herein, we report a case of a cerebral abscess caused by L. monocytogenes, review the relevant literature and discuss the pathogenesis, diagnosis and treatment of infection with this bacterium. We present the following case in accordance with the CARE reporting checklist (available at https://apm.amegroups.com/article/view/10.21037/apm-22-383/rc).
Case presentation
Our patient was a 59-year-old male. He experienced numbness in the right fingers radiating to the wrist 13 days prior. After 3 days, he progressed to aphasia and weakness of the right upper limbs. The patient visited a local hospital, and a brain CT scan revealed low density in the left frontoparietal lobe, which was considered ‘acute cerebral infarction’ (Figure 1A). After two days of anticoagulation therapy, the area of numbness enlarged, combined with speech disorder and weakness of the right upper limb. The patient’s symptoms did not improve after standard stroke treatment. The patient had a history of type II diabetes and a 20-day course of oral prednisolone (40 to 25 mg/day) due to iridocyclitis a month and a half ago. He had a tooth extraction 1 month prior and denied a history of otitis. Neurological examination showed the following: slightly dysfluent speech, with the tongue deviating to the right; bilaterally equal response to painful stimuli in the face; and decreased sensation to pinpricking and touch in the right arm. His strength was graded as follows: right arm, 0/5; right leg, 2/5; left extremities, 4/5. Deep-tendon reflexes were symmetric, and the Babinski sign was negative. No rigid neck or Kernig’s sign was present.
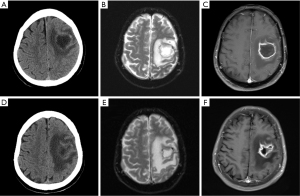
After admission, blood analysis revealed mild leukocytosis of 10.9×109/L with an elevated neutrophil count of 7.4×109 but normal hematocrit and platelet counts. Lumbar Puncture was performed. Cerebrospinal fluid (CSF) results were as follows: cell count, 1/mm3; total protein, 1.04 g/L; and culture, negative. Brain MRI showed that the frontoparietal lesion was a cystic-solid mass measuring 3.0 cm with low T1 and equal mixed T2 signals. Diffusion-weighted imaging (DWI) indicated a high signal in the region of the lesion, with ring enhancement around the lesion (Figure 1B,1C). These results suggested an intracranial mass lesion possibly caused by infection.
The patient underwent needle biopsy of a left-side frontoparietal mass under general anesthesia, and 10 mL of yellowish-gray pus was drained and submitted for bacteriological testing. The bacterial culture results revealed the presence of Listeria monocytogenes, which was sensitive to penicillin G, ampicillin, trimethoprim and meropenem. The final diagnosis was cerebral abscess due to L. monocytogenes. It took about 10 days to wait for bacterial culture results and drug susceptibility results, and we first empirically used the broad-spectrum antibiotic meropenem for 12 days (2 g Q8 h) until culture results were available. After getting the susceptibility results, we switched the antibiotic to oral trimethoprim/sulfamethoxazole 160/800 mg/12 h for an additional 2 weeks. Supportive treatment, including hypoglycemic therapy and rehabilitation training, was administered simultaneously. The symptoms of slurred speech, numbness and impaired muscle strength of the right leg improved, though muscle strength of the right upper limb did not recover. CT and MRI examinations performed 2 weeks after the biopsy revealed a smaller abscess and reduced perifocal edema (Figure 1D-1F).
The patient was transferred to a local hospital for rehabilitation and continued trimethoprim/sulfamethoxazole for 8 weeks. The remaining right arm dysfunction recovered. At six months, the patient had returned to normal daily activities and only exhibited weakness of the right fingers. The patient is very satisfied with the treatment, he believes that he received prompt and effective therapy.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
The significance of this case is that the patient's initial symptoms were numbness and weakness of the right upper limb, accompanied by aphasia, with no fever. The patient was once diagnosed with acute cerebral infarction. This can be a warning to clinical work. For those patients with hemiplegia or aphasia who have high risk factors for infection, we should consider the possibility of central nervous system infection.
L. monocytogenes, an intracellular bacterium, is well adapted for survival as a saprophyte in soil and decaying vegetation. L. monocytogenes was recently shown to penetrate the intestinal mucosa and enter the blood circulation following oral ingestion, leading to systemic disease in adults (7). Immune clearance of Listeria depends on macrophages activated by T cells. Production of tumor necrosis factor (TNF) and nitric oxide (NO) by macrophages via stimulation of IL-18 (interleukin) also participates in this process (8). Therefore, factors affecting the survival and function of macrophages may increase susceptibility to L. monocytogenes in hosts. Risk factors include pregnancy, immunodeficiency, cancer, HIV infection, cirrhosis, diabetes mellitus, alcohol intoxication and immunosuppressive therapy (3,9). L. monocytogenes can invade the bloodstream via intestinal infection, cross the blood-brain barrier and invade the central nervous system. The epithelium of the choroid plexus allows this bacterium to gain access to the central nervous system (CNS) to induce meningitis, which is the most common CNS symptom of listeriosis. However, the mechanism of listerial encephalitis is different, and the formation of brain abscesses is a rare occurrence.
Eighty-seven cases of brain abscess caused by Listeria from 1968 to 2021 have been reported (10-15). Fifty-five (63.2%) patients were male, and the average age was 54.3 years old. A total of 68/87 patients (78.2%) had one or more risk factors for developing listeriosis in the CNS, and 18/87 (20.7%) had no risk factors; 1/87 (1.1%) had an undetermined status. The mortality rate was 23.0%. Blood culture results were available for 67 cases, and 54/67 (80.6%) were positive. L. monocytogenes was isolated from the cerebrospinal fluid or brain abscess of 34/67 (50.7%) patients. A total of 27/81 (33.3%) patients received monotherapy, and 54/81 (66.7%) received combination therapy. Ampicillin was the most commonly used antibiotic (in 63 cases; Table 1).
Table 1
| High-risk patients | Mortality rate | Blood cultivation rate | CSF or brain abscess cultivation rate | Monotherapy rate | Combination therapy rate |
|---|---|---|---|---|---|
| 68/87 (78.2%) | 23.0% | 54/67 (80.6%) | 34/67 (50.7%) | 27/81 (33.3%) | 54/81 (66.7%) |
CSF, cerebrospinal fluid.
The patient in this study had a history of oral glucocorticoids for iridocyclitis, which may be a risk factor for Listeria infection. Symptoms of sensory and movement dysfunction with patchy low density on CT were easily misdiagnosed as acute infarction. However, his relatively stable condition and discrepancy between the lesion and artery distribution were important for diagnosis. His history of diabetes, dental treatment and glucocorticoid treatment not only increased the risk of infection but also resulted in atypical symptoms by inhibiting the immune response. Imaging and examination findings were consistent with brain abscess. No marked abnormalities were found by CSF examination, which may be associated with the formation of an abscess capsule. In this case, needle biopsy and bacterial culture helped in determining the diagnosis of L. monocytogenes infection, though initial symptoms of the infection were nonspecific, manifesting as dysfunction of the corresponding brain region. Symptoms of fever may be absent if a local capsule forms or if there is a history of oral glucocorticoid use. Imaging findings are similar to those of other brain abscesses: equal- or low-density mass with low-density perifocal edema by CT scan; MRI showing a center lesion with T1 low signal and T2 high signal, capsule with T1 equal and T2 low signal, and surrounding edema zone (16). Treatment of brain abscess caused by Listeria is consistent with treatment of abscesses caused by other pathogens, including surgery to remove the lesion and the use of appropriate antibiotics based on drug susceptibility testing. According to previous research, patients who accepted surgical treatment had better survival than those who did not (74% to 63%) (17). Ampicillin is the first choice of antibiotic due to its ability to penetrate the blood-brain barrier and the rare drug resistance. Combination with trimethoprim/sulfamethoxazole, meropenem and imipenem is feasible, but Listeria is resistant to cephalosporin antibiotics.
Conclusions
Brain abscess caused by L. monocytogenes is rare, but it should be considered in patients who have risk factors for listeriosis. Pathogen infection, including with Listeria monocytogenes, should be taken into account when patients with impaired immune function exhibit hemiplegia and aphasia. However, Listeria infection should also be considered in immunocompetent patients because risk factors are absent in 21% of cases. Performing needle biopsy or lesion resection and starting antibiotic therapy according to drug susceptibility testing in the early stage is key to treating this kind of disease.
Acknowledgments
We thank all the medical staff involved in treating the patients.
Funding: This work was supported by the National Natural Science Foundation of China (No. 81541119).
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://apm.amegroups.com/article/view/10.21037/apm-22-383/rc
Peer Review File: Available at https://apm.amegroups.com/article/view/10.21037/apm-22-383/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://apm.amegroups.com/article/view/10.21037/apm-22-383/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bille J. Manual of Clinical Microbiology. 9th ed. Washington, DC: ASM Press 2007.
- Centers for Disease Control and Prevention (CDC). Vital signs: Listeria illnesses, deaths, and outbreaks--United States, 2009-2011. MMWR Morb Mortal Wkly Rep 2013;62:448-52. [PubMed]
- Charlier C, Perrodeau É, Leclercq A, et al. Clinical features and prognostic factors of listeriosis: the MONALISA national prospective cohort study. Lancet Infect Dis 2017;17:510-9. [Crossref] [PubMed]
- Listeriosis Lorber B. Clin Infect Dis 1997;24:1-9; quiz 10-1. [Crossref] [PubMed]
- Disson O, Lecuit M. Targeting of the central nervous system by Listeria monocytogenes. Virulence 2012;3:213-21. [Crossref] [PubMed]
- Drevets DA, Bronze MS. Listeria monocytogenes: epidemiology, human disease, and mechanisms of brain invasion. FEMS Immunol Med Microbiol 2008;53:151-65. [Crossref] [PubMed]
- Radoshevich L, Cossart P. Listeria monocytogenes: towards a complete picture of its physiology and pathogenesis. Nat Rev Microbiol 2018;16:32-46. [Crossref] [PubMed]
- Neighbors M, Xu X, Barrat FJ, et al. A critical role for interleukin 18 in primary and memory effector responses to Listeria monocytogenes that extends beyond its effects on Interferon gamma production. J Exp Med 2001;194:343-54. [Crossref] [PubMed]
- de Noordhout CM, Devleesschauwer B, Angulo FJ, et al. The global burden of listeriosis: a systematic review and meta-analysis. Lancet Infect Dis 2014;14:1073-82. [Crossref] [PubMed]
- Tiri B, Priante G, Saraca LM, et al. Listeria monocytogenes Brain Abscess: Controversial Issues for the Treatment-Two Cases and Literature Review. Case Rep Infect Dis 2018;2018:6549496. [Crossref] [PubMed]
- Trachuk P, Marin Saquicela T, Levi M, et al. Listeria brain abscess in a patient with autoimmune hepatitis. IDCases 2019;17:e00569. [Crossref] [PubMed]
- Flores-Perez RO, Villarreal-Villarreal CD, Garza JAC, et al. Supratentorial Listeria monocytogenes Brain Abscess in a Patient with Liver Cirrhosis. Ann Indian Acad Neurol 2020;23:107-9. [PubMed]
- Lan ZW, Xiao MJ, Guan YL, et al. Detection of Listeria monocytogenes in a patient with meningoencephalitis using next-generation sequencing: a case report. BMC Infect Dis 2020;20:721. [Crossref] [PubMed]
- Zhang J, Huang S, Xu L, et al. Brain abscess due to listeria monocytogenes: A case report and literature review. Medicine (Baltimore) 2021;100:e26839. [Crossref] [PubMed]
- Chung J, McCarthy KL, Redmond A, et al. Listeria monocytogenes brain abscess as a late complication of allogeneic haemopoietic stem cell transplantation. Intern Med J 2021;51:1005-6. [Crossref] [PubMed]
- Slezák O, Žižka J, Kvasnička T, et al. Worm-like appearance of Listeria monocytogenes brain abscess: presentation of three cases. Neuroradiology 2020;62:1189-93. [Crossref] [PubMed]
- Limmahakhun S, Chayakulkeeree M. Listeria monocytogenes brain abscess: two cases and review of the literature. Southeast Asian J Trop Med Public Health 2013;44:468-78. [PubMed]


