Attributes and outcomes of end stage liver disease as compared with other noncancer patients admitted to a geriatric palliative care unit
Introduction
End stage liver disease (ESLD), now the 12th leading cause of mortality in North America, is increasingly more prevalent as a noncancer disease requiring management in palliative care (1). Decompensation in ESLD brings forth a myriad of medical complications and patients commonly face progressive, fulminant, and often complex symptom burdens. These characteristic attributes of ESLD impact both patient function and quality of life throughout the natural progression of disease (2-4). Although the natural trajectory of these patients is a gradual decline, patient’s clinical and personal experiences are complicated by episodic and acute and life-threatening disease exacerbations, often requiring multiple hospital admissions and stabilizations resulting in an uncertainty in prognosis (5,6). This is further complicated by the fact that some patients with ESLD are undergoing assessment for transplant or are pending assessment for transplant when a severe decompensation episode occurs.
Due to the unpredictable nature of complications and outcomes, and lack of a defined “terminal phase”, palliative care is often initiated only when death is perceived as being imminent. This is evidenced as ESLD patients rarely are referred to palliative care services (7,8). Palliative care units (PCUs) can serve as an option for continued care for those living with life-limiting illness such as ESLD. Although there is growing support that such a service should be available based on needs, not diagnosis or prognosis, PCUs are a limited resource and are not able to accommodate longer patient admissions. Out of the multiple PCU admission variables, such as complexity of symptoms, support needs and patient and family preferences, prognosis is often restricted to those patients with 3 months or less (9).
Given the relative scarcity of data regarding the illness experience of patients with ESLD admitted to a PCU (10-12), the assumption is made that they follow the same trends as other noncancer terminal conditions. There is conflicting data as to whether or not patients with noncancer diagnoses, of which ESLD is included, “out-live” their prognosis when compared to cancer patients and take up resources from an otherwise deserving patient when admitted to a PCU (6,13,14). Anecdotally, concerns have been raised that ESLD patients may be admitted late in their disease course, thus not allowing for equitable access to such a service because of concern over a perceived longer length of stay (LOS).
The aim of this study is to better characterize the illness experience of patients with ESLD on a geriatric PCU comparing ESLD patients and noncancer patients in terms of admission Palliative Performance Score (PPS), estimated prognosis and LOS.
Methods
Study design and setting
This was a single-center retrospective chart review of all noncancer patients (n=235) admitted to Baycrest Health Sciences Palliative Care Unit in Toronto, Canada from September 1st 2011 to April 10th 2015. Baycrest Health Sciences is a provincially funded, community academic non-acute hospital attached to both a long term care and retirement living facility, specializing in chronic disease management and geriatric care. The PCU is a 31-bed in-patient facility with 23 beds allocated to patients with a prognosticated mortality of 3 months or less. The remaining 8 beds are for longer-term palliative admission (prognosticated mortality greater than 3 months and less than 1 year). Referral to the PCU is standardized via a common referral form (CRF) for each patient that, in addition to demographic data, requires a calculation of PPS and an estimated prognosis (<3 vs. >3 months and <1 year). The PPS is a performance scale designed to represent functional status among patients receiving palliative care. The PPS is divided into 11 performance categories that are measured in 10% decremental stages from 100% (no evidence of disease, no limitations on any aspect of daily life) to 0 (deceased) (15). A higher PPS represents a higher functional status.
The estimated prognosis on the CRF requires that the referring physician indicate a range they feel best estimates the patient’s prognosis (<30, 31–90, 91–180, 181–365 days). These criteria are reviewed by the admitting physician along with the intake social worker on the PCU. Prognosis, complexity of symptom control issues and patient and family circumstances are used to prioritize admissions. If admission appropriateness is questioned, further discussions are held with the multidisciplinary team and referring center.
Patients
Our study considered and included all patients admitted to the PCU during the study period. The admission and exclusion criteria to the study are those that were utilized for PCU admission: prognosis less than a year, with the majority of patients having a prognosis of less than 3 months (23/31 allocated beds in the PCU), age greater than 65 years of age, the presence of a life-limiting disease, agreement to palliative care philosophy, a do not resuscitate status and prognosis. By these definitions, all patients with ESLD were those excluded from transplant. This study was approved by the Research Ethics Board at Baycrest Health Sciences.
Data collection and analysis
Information was extracted from electronic medical records for all patients who were admitted during that time period. Demographics were collected, as well as admitting diagnosis, source of admission (home, acute care hospital, and long term care), PPS score within 7 days of admission (admission PPS), estimated prognosis, LOS (from admission to death or discharge) and disposition (death or discharge location). The estimated prognosis, as described above, was categorized in four groups (days): <30, 31–90, 91–189, and 181–365 days. The patient’s admission PPS score was collected from the electronic record on the day of admission or up to and including their first week of admission. We compared demographic data, LOS, estimated prognosis, and PPS between ESLD and other noncancer patients using Welch’s t-test. Descriptive statistics were used to characterize the patient sample. We measured correlations between LOS and patient characteristics using Pearson’s test and chi square analyses. All statistical tests were performed using SPSS version 22.0.
Results
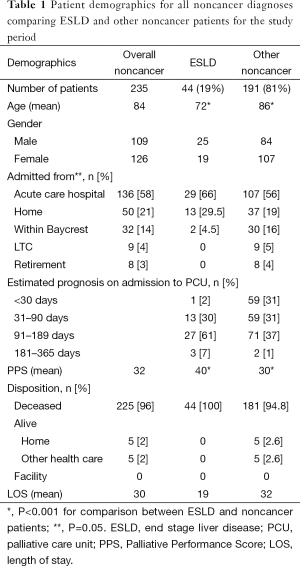
There were 235 patients with noncancer diagnoses and 756 patients with cancer diagnoses admitted to the PCU during the study period. All 235 patients with noncancer diagnoses were included with their baseline characteristic data presented in Table 1. Overall, there were 44 (19%) patients with ESLD. There were slightly more males in the ESLD group compared to the other noncancer group with a M:F ratio of 1.3 vs. 0.79. Compared with other noncancer patients, ESLD patients are both significantly younger (mean age of 72 vs. 84, P<0.001) and are admitted with a significantly higher PPS (mean PPS of 40 vs. 30, P<0.001). There were no differences in estimated prognosis between ESLD patients and other noncancer patients.
Full table
There was also no significant differences in LOS (P=0.18) between ESLD patients and other noncancer patients. However, there was a nonsignificant trend towards a shorter LOS for ESLD patients; the mean LOS for ESLD patients was 19 days and for the other noncancer patients 32 days. There was a significance in source of admission for the overall group in that both patients with ESLD and other noncancer patients were admitted from acute care more often than other locations (P=0.05). There was no significance in disposition (P=0.30); the vast majority of patients with ESLD and other noncancer diagnoses died on the PCU.
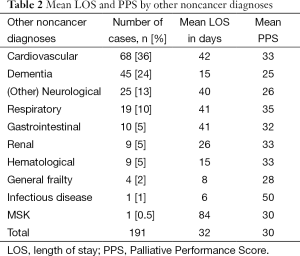
For all other noncancer patients (excluding ESLD), the majority of patients had either cardiovascular disease or end-stage dementia (Table 2). Among the other noncancer group, patients had similar PPS scores except one patient admitted with an infectious disease state as their primary diagnosis who had a higher PPS of 50 compared to the mean of 30 (Table 2). This patient along with those in the dementia, hematological and general frailty category had a shorter LOS that did not reach statistical significance.
Full table
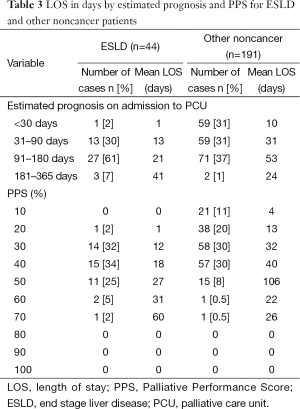
The majority of patients with ESLD were admitted with a trend towards a longer estimated prognosis of 3–6 months (n=27, 61%), compared to the patients in the other noncancer group who had about an even one-third split across 1 (n=59, 31%), 3 (n=59, 31%), and 6 (n=71, 37%) months (Table 3). Across all PPS scores between 20% and 50%, there was a nonsignificant trend towards a shorter LOS for ESLD patients compared to other patients with noncancer.
Full table
Pearson product moment correlation was computed between PPS and estimated prognosis, PPS and LOS, and estimated prognosis and LOS (Table 4). For each patient population, there was a strong positive correlation between PPS and estimated prognosis (0.89 and 0.94 for ESLD and other noncancer respectively, P<0.001 for each). Thus, in those with higher PPS scores, the clinician was more often assigning a better estimated prognosis. The correlation between PPS and LOS was less for both groups but better for ESLD patients (0.47, P<0.001) as compared with the other noncancer group (0.31, P<0.001). A similar in magnitude correlation was observed for estimated prognosis as compared with LOS in both groups, 0.39 (P<0.01) and 0.26 (P<0.001) for ESLD and other noncancer patients. However, in both instances, the linear correlation between PPS and LOS and estimated prognosis and LOS was numerically larger for ESLD patients as compared with other noncancer patients.

Full table
Discussion
Our study characterizes attributes and clinical course of ESLD patients as compared with other noncancer patients in a geriatric PCU. Overall, patients with ESLD were younger and had a higher PPS score with no significant difference in LOS or disposition when compared to other noncancer patients. There was a statistically nonsignificant trend towards a shorter LOS for ESLD patients as compared with other noncancer patients. Thus, although ESLD patients had a better functional status on admission, all of these patients did not survive and this occurred earlier in their stay as compared with other noncancer patients. In addition, physician-based estimated prognosis on admission, which takes into account an overall clinical gestalt including consideration of a patient’s PPS, favoured a better prognosis than what actually occurred in the ESLD patient group, despite a higher mean PPS value. PPS as a metric appeared to correlate slightly better with actual LOS in the ESLD patients as compared with other noncancer patients. In our study, it is not surprising that patients admitted with ESLD are younger, with a higher PPS and a trend towards a longer estimated prognosis as the epidemiology of ESLD generally afflicts a younger population of patients and many can be asymptomatic and well-functioning for decades, often completely unaware of their diagnosis and progressive nature of disease, until complications abruptly present in the decompensated phase of the illness (16).
For patients with ESLD, our study suggests that estimated prognosis and PPS, although well correlated, do not translate to longer survival and most patients die sooner as compared with other noncancer patients despite a better on-admission functional status. Also, the clinician’s estimate of prognosis for both patients with ESLD and other noncancer patients is inaccurate with a tendency to overestimate. We were not expecting to find that PPS and LOS were more strongly correlated in the ESLD patients when compared to other noncancer patients given the same estimated prognosis. Considering this, previous studies have documented the relationship between PPS and survival and in particular, the stronger association between lower PPS scores and shorter length of survival compared to higher PPS scores (14,17,18). However in our study, despite patients with ESLD having a significantly higher PPS, which would normally guide the clinician to anticipate a longer LOS, these patients with ESLD in fact did not live longer, rendering this important finding. Thus, although PPS and LOS correlated well in the ESLD patient group, the ability to reliably estimate prognosis based on clinical judgement and consideration of PPS likely results in an over-expected survival duration. As noted, LOS was shorter for ESLD patients albeit without reaching significance. Taken together, on-admission assessment, including utilization of PPS, may not sufficiently capture all the relevant parameters that may be of importance when estimating prognosis in ESLD patients.
The implications for our findings are three fold. Firstly, patients with ESLD and other noncancer diagnoses, do not demonstrate a long LOS (>3 months). In our study, patients with ESLD tend to have a very short LOS, and thus bed utilization. Referring physicians and PCU administrators should therefore not be concerned with ESLD patients possibly stabilizing and taking up a short-term bed for a longer period. Secondly, our study demonstrated that for patients with ESLD, the PPS was a better correlate of survival than the clinician’s estimated prognosis which is consistent with other studies (9). Because this correlation is stronger in ESLD patients than in other noncancer patients, PPS should receive stronger consideration over estimated prognosis as a PCU admitting criteria for patients with ESLD. Finally, despite having a higher PPS, these patients tend to have a shorter LOS and often always die in the PCU. The reason for this may be uniquely attributed to the unpredictable nature of complications related to ESLD in that the onset and severity of the complications can change prognosis rapidly, causing a faster rate of decline. Appreciating this difference in illness trajectory of patients with ESLD compared to other noncancer patients on a PCU would have implications for prognosticating and planning for end-of-life care for patients, their families and the care team.
Our study has several limitations. To begin, our study is limited by being from a single center and age of the patients included. Mortality from chronic liver disease and cirrhosis is highest between the ages of 55–64 and our study does not include patients in this age range (19). Further to this, some bias may also exist in the population of ESLD patients studied in a geriatric palliative setting as these patients may not fully represent the spectrum of clinical decline observed in various etiologies of ESLD. Also, other patient comorbidities that may affect survival were not taken into account in our analysis. A limitation of our study is a small sample size of ESLD patients as compared with noncancer, although the ratio of patients in these two groups may be reflective of admission patterns at other general PCUs. Regarding the information on the common referral form (CRF), it is not known whether the referring physician was a specialist palliative care physician or not and whether that would have influenced the estimated prognosis and accuracy of the PPS in any way. The admitting PPS was not independently verified for accuracy at the time of patient admission, however independent verification of a patient’s PPS at the time of admission to a PCU is often not the norm and therefore, this limitation may improve the generalizability of our findings. We also cannot conclude from our study whether or not our PCU is prioritizing admissions on the basis of location or if patients with ESLD and other noncancer diagnoses in settings other than acute care, are not being referred.
Conclusions
Patients with ESLD present with significant palliative care needs which can be supported in various settings throughout the continuum of their illness experience. PCUs serve as an option for continued care and patients should be admitted based on needs rather than diagnosis or prognosis. This study demonstrates that patients admitted with ESLD to a PCU likely will have a different illness experience than their other noncancer counterparts and that they should not be refused an admission because of fear of outliving their prognosis. Better characterization of this patient population and tailoring to their palliative care requirements will likely lead to a significant benefit among patients, caregivers and health providers. Moreover, additional prognostic tools may need to be developed that better prognosticate LOS for ESLD patients admitted to PCUs.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Everhart JE, editor. The burden of digestive diseases in the United States. Washington, DC: US Government Printing Office, 2008:111-4.
- Bianchi G, Marchesini G, Nicolino F, et al. Psychological status and depression in patients with liver cirrhosis. Dig Liver Dis 2005;37:593-600. [Crossref] [PubMed]
- Moscucci F, Nardelli S, Pentassuglio I, et al. Previous overt hepatic encephalopathy rather than minimal hepatic encephalopathy impairs health-related quality of life in cirrhotic patients. Liver Int 2011;31:1505-10. [Crossref] [PubMed]
- Poonja Z, Brisebois A, van Zanten SV, et al. Patients with cirrhosis and denied liver transplants rarely receive adequate palliative care or appropriate management. Clin Gastroenterol Hepatol 2014;12:692-8. [Crossref] [PubMed]
- D'Amico G, Garcia-Tsao G, Pagliaro L. Natural history and prognostic indicators of survival in cirrhosis: a systematic review of 118 studies. J Hepatol 2006;44:217-31. [Crossref] [PubMed]
- Fox E, Landrum-McNiff K, Zhong Z, et al. Evaluation of prognostic criteria for determining hospice eligibility in patients with advanced lung, heart, or liver disease. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. JAMA 1999;282:1638-45. [Crossref] [PubMed]
- Ogle KS, Mavis B, Wyatt GK. Physicians and hospice care: attitudes, knowledge, and referrals. J Palliat Med 2002;5:85-92. [Crossref] [PubMed]
- Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 2010;363:733-42. [Crossref] [PubMed]
- Downar J, Chou YC, Ouellet D, et al. Survival duration among patients with a noncancer diagnosis admitted to a palliative care unit: a retrospective study. J Palliat Med 2012;15:661-6. [Crossref] [PubMed]
- Boyd K, Kimbell B, Murray S, et al. Living and dying well with end-stage liver disease: time for palliative care? Hepatology 2012;55:1650-1. [Crossref] [PubMed]
- Iredale J. End-stage chronic liver disease: time to define a good death. Hepatology 2008;47:1799-800. [Crossref] [PubMed]
- Lamba S, Murphy P, McVicker S, et al. Changing end-of-life care practice for liver transplant service patients: structured palliative care intervention in the surgical intensive care unit. J Pain Symptom Manage 2012;44:508-19. [Crossref] [PubMed]
- Christakis NA, Lamont EB. Extent and determinants of error in doctors' prognoses in terminally ill patients: prospective cohort study. BMJ 2000;320:469-72. [Crossref] [PubMed]
- Lau F, Maida V, Downing M, et al. Use of the Palliative Performance Scale (PPS) for end-of-life prognostication in a palliative medicine consultation service. J Pain Symptom Manage 2009;37:965-72. [Crossref] [PubMed]
- Anderson F, Downing GM, Hill J, et al. Palliative performance scale (PPS): a new tool. J Palliat Care 1996;12:5-11. [PubMed]
- Scaglione S, Kliethermes S, Cao G, et al. The Epidemiology of Cirrhosis in the United States: A Population-based Study. J Clin Gastroenterol 2015;49:690-6. [Crossref] [PubMed]
- Glare P, Sinclair C, Downing M, et al. Predicting survival in patients with advanced disease. Eur J Cancer 2008;44:1146-56. [Crossref] [PubMed]
- Chow E, Harth T, Hruby G, et al. How accurate are physicians' clinical predictions of survival and the available prognostic tools in estimating survival times in terminally ill cancer patients? A systematic review. Clin Oncol (R Coll Radiol) 2001;13:209-18. [PubMed]
- Centers for Disease Control and Prevention. National Center for Health Statistics. Health Data Interactive. Available online: www.cdc.gov/nchs/hdi.htm


