Review on applications of metastatic lymph node based radiomic assessment in nasopharyngeal carcinoma
Abstract
Nasopharyngeal carcinoma (NPC) has a distinct geographical prevalence in Southern China and Southeast Asia with a high overall survival rate (> 90%) in the early stage of the disease. However, almost 85% of patients suffer from the locally advanced disease with nodal metastasis at diagnosis. The overall survival rate would drastically drop to 63%. In addition to the generic tumor, nodal, and metastasis (TNM) staging, radiomic studies focusing on primary nasopharyngeal tumors have gained attention in precision medicine with artificial intelligence. While the heterogeneous presentation of cervical lymphadenopathy in locally advanced NPC is regarded as the same clinical stage under TNM criteria, radiomic analysis provides more insights into risk stratification, treatment differentiation, and survival prediction. There appears to be a lack of a review that consolidates radiomics-related studies on lymph node metastasis in NPC. The aim of this paper is to summarize the state-of-the-art of radiomics for lymph node analysis in NPC, including its potential use in prognostic prediction, treatment response, and overall survival for this cohort of patients.
Keywords
INTRODUCTION
Nasopharyngeal carcinoma (NPC) is cancer arising from the epithelium of the nasopharynx, frequently originating at the Fossa of Rosenmüller. According to World Cancer Research Fund International, NPC is ranked the twenty-second most common cancer worldwide, with over 133,000 new cases in 2020[1]. Although NPC is uncommon in western countries, it is characterized by distinct geographical prevalence and male predominance in the orient. More than 80% of the global cases were diagnosed in endemic areas such as Southern China and Southeast Asia. For instance, in Hong Kong, it was the seventh most common cancer in men and the seventeenth most common cancer in women in 2019, with a male-to-female ratio of 2.9 to 1[2].
The staging of NPC adheres to the Tumor, Node, Metastasis (TNM) system of the Union for International Cancer Control (UICC) and the eighth edition of the American Joint Committee on Cancer (AJCC)[3]. For accurate disease staging, magnetic resonance imaging (MRI) or positron emission tomography with computed tomography (PET-CT) images are essential. The overall survival rate in early-stage (stage I or II) NPC can be as high as 93%, while it drops to 63% in the advanced stage (stage III to IVb)[4]. A meta-analysis showed that 85% of locally advanced NPC patients presented with nodal metastasis at diagnosis and bear a poor survival outcome[5].
With the recent trend of investigating the applications of artificial intelligence (AI) and deep learning (DL), the use of radiomics has drawn more attention in the precision therapy of NPC. There are numerous comprehensive reviews on the applications of AI in NPC[6,7]. These reviews focused mainly on the radiomic analysis of the gross tumor volume[8], while others evaluated the radiomics in PET-CT of NPC lymph nodes and primary tumors. A recent study by Xia et al. proposed that lymph node assessment as opposed to that of primary tumors performed better in survival prediction[9]. However, to the best of our knowledge, minimal effort has been placed to explore and summarize radiomics-related studies on lymph node metastasis in NPC[9].
This review aims to summarize the current evidence for the radiomics use for NPC with nodal metastasis and explore its clinical potential in the prognostic prediction, treatment response, and overall survival of NPC patients with lymph node metastasis.
ARTIFICIAL INTELLIGENCE AND RADIOMICS
The term “radiomics” is regarded as novel among clinicians. It is often misunderstood as synonymous and interchangeable with artificial intelligence, machine learning, and deep learning. This section provides an overview and the interrelationship of these terminologies.
Artificial intelligence (AI) is a constantly evolving technology, and with recent efforts exploring the applications of AI and medical imaging in NPC from diagnosis, imaging segmentation for radiotherapy planning to treatment monitoring and prognostication.
Ng et al. reviewed the implementation of AI in NPC, summarizing four main types of applications, namely auto-contouring, diagnosis, prognosis, and treatment planning[7]. AI, first termed by an American computer scientist John McCarthy in 1956, has been expanded to a wide spectrum of applications and abilities demonstrated by the machine[10]. For example, knowledge representation, natural language processing, automatic reasoning, machine learning, intelligent robots, and automatic programming are under the category of AI[11].
Machine learning is a branch of AI using algorithmic systems to perform tasks such as prediction and diagnosis of interest[12]. Deep learning, also called deep neural network learning, employs a neural network to allow automatic learning capability mimicking a learning process in the human brain[13].
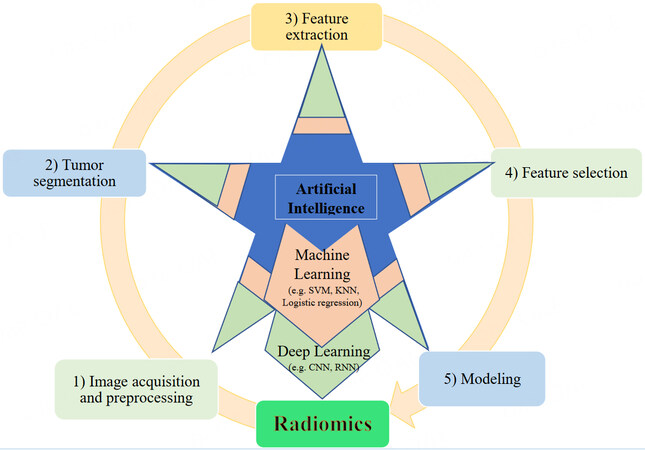
Radiomics is a quantitative approach in which models are built based on high-dimensional spatial features in medical imaging that are not visually perceptible and interpretable by human beings[14,15]. Radiomics is a high-frequency lexicon in oncological medicine. It requires of the acquisition, preprocessing, and extraction of a huge amount of data in medical images for quantitative analysis, providing additional information based on the differences in tumor characteristics such as shape and textures[16]. In radiomics, a large number of features are generated to determine the non-linear relationship between them. With AI development, computer scientists adopt deep learning algorithms and machine learning methods for tumor segmentation, feature extraction, and selection, and finally formulating a model for analysis [Figure 1].
METHODS
A literature search was conducted to retrieve all studies of NPC with nodal metastasis under radiomic analysis. Keywords were combined using Boolean logic to produce the resulting search phrase: (“artificial intelligence” OR “machine learning” OR “deep learning” OR “neural networks, computer” OR “algorithms”) AND (“nasopharyngeal neoplasm” OR “Nasopharyngeal carcinoma” OR “NPC”) AND ("lymph nodes” OR “lymphatic metastasis”). Using this search phrase, studies were searched on PubMed, Ovid Medline, and Embase between Jan 2002 to June 2022. The studies were screened, with duplicates removed. Inclusion and exclusion criteria were defined to allow evaluation only on those applying radiomics in NPC with nodal metastasis [Table 1]. The authors looked into the methodology and image segmentation methods of individual studies. Studies with lymph node-based radiomic analysis as regions of interest (ROI) were included. Studies that are limited to primary tumors as ROI or those without detailed descriptions of lymph node analysis were excluded. Fourteen studies were selected to highlight the current state-of-the-art lymph node-based radiomics applications in NPC.
Inclusion and exclusion criteria for study selection
| Inclusion criteria | Original studies Published in English language Published from 2002 to date Full-text paper available Details of image data and features extraction were described Image segmentation specifically mentioned on lymph node analysis as regions of interests Studies related to Nodal metastasis of NPC |
| Exclusion criteria | Conference papers and literature reviews Written in other languages Full-text not available Deep learning or radiomics were not used for modelling Only the primary site of tumour was segmented as regions of interest in features selection |
RADIOMIC STUDIES IN LYMPH NODE ANALYSIS AND RISK STRATIFICATION
There are studies exploring the full potential of radiomic analysis in both primary tumor and nodal metastasis in head and neck cancer, suggesting that the additional metastatic lymph node radiomic information could be a complementary prognostic factor in loco-regional control of the disease[17,18]. Studies extracted in Table 2 investigated the radiomic features of lymph node metastasis in NPC patients to predict high-risk patients requiring treatment adjustment and modification.
Studies of lymph node analysis for NPC in treatment planning and risk stratification using radiomics
| Authors, year | No. of cases (patients) | No. of radiomic features | Image modalities | AI methods* | Study aim | Performance metrics/results | Conclusion | Limitation |
| Li et al., 2018[19] | 306 | 1,117 | MRI | ANN, KNN, SVM models | To analyse the recurrence patterns and reasons in NPC patients with IMRT; To investigate the feasibility of radiomics for analysis of radioresistance | AUCs: 0.727-0.835 True positive rate: ANN: 0.815 KNN: 0.778 SVM: 0.741 Accuracy: ANN: 0.812, KNN: 0.775, SVM: 0.732 | The main recurrence patterns: In-field and high-dose region relapse. | Small sample cohort; Single centre; Retrospective study; Lack of independent external validation |
| Yu et al., 2019[20] | 70 Training set = 51; Testing set = 19 | 479 | MRI | SMOTE algorithm, center and scale and boxcox, Pearson correlation coefficient, and LASSO regression | To determine tumoral biomarkers using pre-treatment MR images for predicting ART eligibility in NPC patients prior to the start of treatment | Average AUCs of 3 different MRI set models: Training set: 0.895-0.984 Testing set: 0.750-0.930 | MRI-based radiomic features are capable for pre-treatment identification of ART eligibility in NPC patients | Heterogeneity of image acquisition and reconstruction protocols; Small cohort; Low rate of adaptive replanning; Retrospective study |
| Kang et al., 2021[21] | 243 | 10,400 | MRI | SMOTE algorithm, center and scale and boxcox, Pearson correlation coefficient, and LASSO regression | A combined model was established based on the MRI-radiomics of pre- and mid-treatment (Tx) to assess the risk of disease progression or death in locally advanced NPC | Training set: AUC pre-Tx: 0.8003 AUC mid-Tx: 0.9253 Accuracy: 0.725 Precision: 0.704 Sensitivity: 0.618 Specificity: 0.805 Test set: AUC pre-Tx: 0.8527 AUC mid-Tx: 0.8849 Accuracy: 0.790 Precision: 0.795 Sensitivity: 0.686 Specificity: 0.868 | The log-rank test of high- and low-risk groups had better prognostic performance in PFS, LRFS, DMFS, and OS than TNM stage. A combined model of pre- and mid-treatment MRI-radiomics successfully categorized patients into high- and low-risk groups | Retrospective study; Single agency; Non-endemic Areas of NPC; Lack of external validation; Disunity of the treatment plan affects the prediction effect of the model |
| Lam, et al., 2021[22] | 135 | 55 | CT and MRI | Ridge algorithm (for single-omics model); MKL algorithm (for multi-omics model) | To investigate the role of different multi-organ omics-based prediction models for pre-treatment prediction ART eligibility in NPC patients | Radiomic model average AUCs: Training set = 0.942; Testing set = 0.927; 64%-94% radiomic features were selected in all the studied multi-omics models | The Radiomic model was found to play a dominant role for ART eligibility in NPC patients, and Radiomic features accounted for the largest proportion of features in all the multi-omics models | Small size single cohort; Model overfitting; |
| Lam et al., 2022[23] | 182 Training set + Internal validation: 124 External validation set: 58 | 2,130 | CT | In-house developed pipeline tool based on Python v3.7.3. Radiomic (R), clinical (C), and combined (RC) models | To investigate the capability of CT based neck nodal radiomics for predicting IfTMs triggered ad hoc ART events in NPC patients | AUCs of Training + internal validation set: R model: 0.784 C model: 0.648 RC model: 0.782 External validation: R model: 0.723 C model: 0.673 RC model: 0.710 | CT-based neck nodal radiomics was capable of predicting IfTM-triggered ART events in NPC patients undergoing RT | Retrospective study; Significant difference in patients between two cohorts; Small sample size |
Five studies from 2018 to 2022 adopted various machine learning algorithms for radiomic analysis with regions of interest in nodal metastasis. All these studies achieved AUCs between 0.725-0.984 in training and testing sets. Of these, four studies employed MRI images for analysis[19-22]. Li et al. identified the NPC recurrence patterns using radiomic analysis, suggesting the feasibility of using radiomics as imaging biomarkers to identify RT-resistant cases. This may facilitate early intervention for NPC patients[19].
Currently, there is no set protocol to identify patients requiring adaptive radiation therapy (ART). During the course of intensity modulated radiotherapy (IMRT), oncologists may consider ART in some patients based on clinical factors such as significant weight loss, changes in palpable cervical lymph node volume, ill-fitting masks, or prolonged treatment breaks. NPC patients at the same clinical TNM stage may respond variably in terms of tumour size and lymph node volume after IMRT. In many cases, the decision of employing ART is dependent on the individual clinicians’ judgment and is not standardized. Lam et al. used CT-based imaging protocol for nodal radiomic analysis in predicting the use of ART, demonstrating the radiomics model outperformed the clinical staging model significantly (P < 0.0001)[23]. The choice of CT was pragmatic and logically sound for its robust, shorter scanning time and good lymph node identification quality in ill-fitting thermoplastic casts (ifTMs). CT offers quick re-assessment of cases with extensive cervical lymphadenopathy before treatment and subsequent shrinkage of the disease during radiotherapy. In addition, studies were able to stratify high-risk NPC patients using the pre-treatment MRI-based radiomic analysis for ART eligibility assessment, facilitating oncologists in streamlining resources to enhance efficiency[20,22].
RADIOMICS STUDIES IN TREATMENT OPTIONS PREDICTION
NPC with nodal metastasis at presentation and time of diagnosis is not uncommon. In fact, more than 75% of patients with NPC are diagnosed at advanced stages (i.e., Stages III and IV)[5,24]. In addition to IMRT, chemotherapy and neoadjuvant chemotherapy are used as adjuncts in the treatment of locally advanced NPC. However, with the known acute and long-term toxicities from radiation and chemotherapy, not all patients are able to tolerate or respond well to the combined treatment modalities. Studies on deep learning and radiomics analyses attempted to predict the treatment response based on an individual’s clinical and biochemical status. By developing various radiomic-based models, therapeutic response prediction could make personalized treatment possible and avoid the unnecessary adverse side effects from chemoradiation. Xu et al. and Wang et al. developed MRI-based radiomic models on NPC lymph node metastasis cohorts to predict treatment responses in chemoradiotherapy (ChemoRT) and neoadjuvant chemotherapy (NAC), as shown in Table 3[25,26]. The sensitivity and specificity of the radiomic models were higher in training cohorts than in validation cohorts. The AUCs of these models were over 0.9 for treatment response prediction for most studies.
Radiomics studies for treatment response prediction
| Authors, year | No. of cases (patients) | No. of radiomic features | Image modalities | AI methods* | Study aim | Performance metrics/results | Conclusion | Limitation |
| Xu et al., 2021[25] | 145 Training set: 102; Testing set: 43 | 2,704 | MRI | IBSI standard; LASSO | To predict the treatment response of metastatic cervical lymph node to ChemoRT in NPC | Primary cohort: AUC = 0.927 Sensitivity = 0.911 Specificity = 0.826 Accuracy = 0.872 Validation cohort: AUC = 0.772 Sensitivity = 0.792 Specificity = 0.790 Accuracy = 0.791 | MRI-based radiomic models might facilitate individualized therapy for metastatic lymph nodes before treatment | Retrospective study; Heterogeneity in MRI image; PET/CT excluded; Single institution |
| Wang et al., 2022[26] | 165 Training set: 85 Testing set: 80 | 31,920 | MRI | RECIST 1.1; Logistic regression and cross-validated by BS with a resampling number of 1,000 | To develop and evaluate a modified radiomic model for the NAC response prognosis in NPC patients | Cross-validation cohort: AUC = 0.948 Sensitivity = 0.849 Specificity = 0.840 Independent testing cohort: AUC = 0.925 Sensitivity = 0.821 Specificity = 0.792. | MRI-based radiomic model showed promising capability for the individual prediction of NAC response in NPC patients, which might provide chances for individualized treatment in NPC patients while retrenching the cost of clinical resources | NAC regimen and treatment cycles are not controlled; Single centre study |
RADIOMICS STUDIES IN SURVIVAL PREDICTION
The clinical staging of NPC is an important prognostic factor for survival. The one-year survival rates of NPC at stage I and stage IV diseases were 99.0% and 78.8% respectively. For stage I disease, the five-year survival has a small decline to 92.7%. However, the five-year survival of a stage IV NPC has a drastic drop to 47.1%[24]. Despite a distinct geographical prevalence in southern China and Southeast Asia, over three-quarters of patients still present late with a neck mass due to its asymptomatic nature at an early stage[24]. With the development in radiomics research, the prognostic performance of clinical staging is often compared with the novel development of radiomic models on survival analysis in locally advanced NPC. Studies focusing on the use of radiomics in predicting survival are listed in Table 4. Yang et al. developed a multidimensional nomogram using nodal volume-based radiomic features to predict progression-free survival, superseding the model using the clinical tumor-node-metastasis (TNM) staging[27].
Radiomics based studies for survival analysis
| Authors, year | No. of cases (patients) | No. of radiomic features | Image modalities | AI methods* | Study aim | Performance metrics/results | Conclusion | Limitation |
| Yang et al., 2019[27] | 224 Training set: 149; Test set: 75 | 260 | MRI | LASSO regression | To develop a multidimensional nomogram for predicting PFS in patients with locoregionally advanced NPC | C-index of nomogram: Training cohort: 0.843 Validation cohort:0.811 C-index of TNM staging: Training cohort: 0.592 Validation cohort: 0.613 | A novel nomogram involving DVHs, GTVnd based radiomic signature could effectively predict the PFS in patients with advanced NPC | Small sample size |
| Ming et al., 2019[28] | 303 Training: 200; Validation: 103 | 208 | MRI | LASSO cox regression | To develop prognosis signatures through a radiomics analysis for NPC patients by pre-treatment MRI | C-index of training set in DFS/OS/DMFS:Radiomics model: 0.692/0.716/0.695; Clinical model: 0.676/0.688/0.634; Combination model: 0.736/0.717/0.719 C-index of validation set in DFS/OS/DMFS:Radiomics model: 0.689/0.786/0.602; Clinical model: 0.722/0.738/0.586; Combination model: 0.751/0.845/0.643 | The DFS and OS radiomics nomograms demonstrated the excellent prognostic estimation for NPC patients with a non-invasive way of MRI. The combination of clinical and radiomics features can provide more information for precise treatment decision | Insufficient number of follow-up; Lack of LRFS analysis; No external validation; |
| Bologna et al., 2020[29] | 136 | 2,144 | MRI | Multivariate Cox regression | To develop prognostic models for overall survival in patients from non-endemic areas (Europe or United States) | The radiomics-based signature had good prognostic power. C-index of OS: 0.68 C-index of LRFS: 0.72 | Radiomic features can provide independent prognostic information in NPC patients from non-endemic areas | Absence of an independent validation cohort; Only include positive nodal disease |
| Zhang et al., 2020[30] | 220; Training set: 132; Internal testing: 44; External testing: 44 | 2,364 | MRI | Univariate analysis; MRMR; Random forest; CPH; DCNN; | To explore the prognostic value of radiomics-based and digital pathology-based imaging biomarkers from macroscopic MRI and microscopic whole-slide images for patients with NPC | C-index of DCNN: Training cohort: 0.741 Internal test: 0.779 External test: 0.689 C-index of combined CRH model: Training cohort: 0.817 Internal test: 0.828 External test: 0.834 C-index of TNM stage: Training cohort: 0.737 Internal test: 0.593 External test: 0.654 | The multi-scale nomogram may serve as a non-invasive, cost-effective, and useful tool for facilitating individualized treatment and future decision-making in NPC | Retrospective study; Relatively small sample size; Molecular profile was not included. All Chinese cohorts |
| Chen et al., 2021[31] | 1,643; Training set: 847; Internal testing: 400; External testing: 396 | - | MRI | LASSO; XGB; SHAP | To predict distant metastasis in locoregionally advanced NPC patients using MRI-based tumor burden features | C-index of Internal/External Validation cohorts: LASSO: 0.707/0.699 XGB-A: 0.683/0.589 XGB-B: 0.739/0.621 XGB-C: 0.766/0.760 | The proposed survival system provides a promising tool for risk stratification in locoregionally advanced NPC patients | - |
| Qiang et al., 2021[32] | 3,444; Training set: 1,838; Internal testing: 787; External testing: 819 | - | MRI | 3D-CNN; XGB; | To distinguish low-risk patients with locally advanced NPC for whom CCRT is sufficient | C-index for DFS: Training cohort: 0.787 Internal validation: 0.776 External validations: 0.719-0.757 The AUCs for DFS: Training cohort: 0.809 Internal validation: 0.806 External validations: 0.756-0.857 | The proposed framework can capture more complex and heterogeneous information to predict the prognosis of patients with locally advanced NPC and potentially contribute to clinical decision making | Retrospective study; Histologically only included WHO types II and III cases; |
| Zhang et al., 2021[33] | 233 Training set: 169; Internal testing: 19; External testing: 45 | - | MRI | LASSO; AIC algorithms | To develop a model to evaluate DMFS in locally advanced NPC | AUCs of Clinical/Radiomic/Combined models Training cohort: 0.698/0.789/0.796 Validation: 0.727/0.761/0.795 Testing: 0.649/0.765/0.808 | The MRI-based combined model evaluates the risk of DMFS in locally advanced NPC patients to provide a complementary tool for making treatment decisions | Retrospective study; Difference in data distribution; Poor radiomic signatures repeatability |
Similar to Yang’s study, all seven studies published from 2019 to 2021 suggested that radiomic models or combined clinical and radiomic models performed better than conventional clinical models in predicting distant metastasis and survival. There are only four studies that provided the quantity of radiomic features used, ranging from 208 to 2,364, for model development and training for reference[27-30].
Locoregional recurrence free survival (LRFS) and distant metastasis free survival (DMFS) are of particularly concern to clinicians in the management of locally advanced NPC with lymph node metastasis. The variability of treatment options, such as neoadjuvant or induction chemotherapy, combined concurrent chemoradiotherapy, IMRT, or targeted therapy, are often compared with its efficacy, survival outcomes and toxicities in locally advanced NPC. Radiomics models could provide useful information in guiding treatment options and predicting survival outcomes based on the imaging-specific “tumor-fingerprint” of each individual patient.
DISCUSSION
This article reviewed studies specifically on lymph node metastasis in NPC for radiomics analysis to evaluate several objectives: risk stratification, treatment response, and survival predictions. Notably, the application of machine learning for the clinical management of NPC commenced more than a decade ago. Aussem et al. used a Bayesian network in machine learning to classify and identify risk factors in NPC in 2012[34]. Ng et al. observed exponential growth in using AI in NPC since 2018[7]. While there is a shift of interest from gross primary tumor volume to cervical lymphadenopathy in NPC for imaging analysis, studies of radiomics targeting lymph node metastasis in NPC have drawn researchers’ attention. Despite the growing number of radiomics studies on locally advanced NPC, they are often piecemeal and fall short of knowledge-building in the area of NPC management. This paper attempted to review and classify relevant pieces of literature according to clinical use. Hence, the knowledge could be better integrated for unleashing the future potential of radiomics in the treatment of NPC with lymph node metastasis.
As a clinician, the concepts of radiomics and deep learning in NPC appear to be a “black box” compared to traditional statistical models for prediction and survival analysis. The lack of understanding and explanation of how the model was built by image feature selection and algorithms raises clinicians’ skepticism about the generated outcomes. Critically analyzing the pitfalls of these studies are difficult from a clinician’s perspective, creating a huge resistance to translating these findings into real clinical applications. To improve the interpretability of AI models, Lundberg and Lee proposed a unified framework - Shapley additive explanations framework (SHAP) to understand how the machine learning models predict based on various weighting of selected features[35]. For example, Chen et al. adopted SHAP to highlight the six features (BMI, EBVDNA, LDH, tumor volume, lymph node volume, and diameter) contributing to the complex nonlinear relationship with distant metastasis in NPC[31]. SHAP was also used in nonmetastatic NPC scenarios. Du et al. suggested tumor shape sphericity, first-order mean absolute deviation, T stage, and overall stage influenced the outcome of 3-year disease[36]. Although SHAP provides an explanation of the pattern learned by radiomic models, it does not correlate nor explain the patient’s characteristics with the imaging trained in the models. Yet, it does provide insights to clinicians in understanding the chain of thoughts of the machine learning models in predicting the outcomes in radiomics analysis.
Besides, whether the models reported could be extended from the training sample to the entire population is a key factor for promoting radiomics analysis into clinical use for the treatment of lymph node metastatic NPC. Most of the current studies involved retrospective data in a single or a few institutions. Since different imaging parameters affect the radiomic features being extracted, reproducibility of the data and feature selection become the major barrier. The major challenge in consideration of the clinical implementation of radiomics is whether the developed models are applicable across different institutions. Tumor segmentation is part of the key steps for radiomic implementation. The contouring of both primary tumor and nodal disease volume from imaging for radiomic features extraction is operator dependent and time-consuming even for an expert radiologist or oncologist. Likewise, the selection of radiomic features requires prior image processing and tumor contouring. Standardization and automation of this process may be a possible direction for this aspect. Automatic segmentation has been shown to reduce the time of radiotherapy planning by up to 30%-40%[37]. The reduction of intra- and inter-observer variability during tumor delineation has also improved the consistency of IMRT performance[37]. Different algorithms, such as single-atlas-based, multi-atlas-based, and deep-learning-based auto segmentation models were developed to delineate the head and neck lymph node metastasis in automatic tumor contouring. Atlas-based auto segmentation takes a collection of image segmentations as an atlas to map and delineate the region of interest of a new patient’s image data set[38-40]. It could help to identify head and neck lymph node lesions[39]. Although atlas-based auto segmentation could reduce the time for lymph node contouring and selection bias, there is no single best atlas to fit all individual image data[38]. Multi atlas-based auto segmentation, using several patients’ tumor segmentations or peer-reviewed manual contours, provides more reference atlases to improve the accuracy in tumor contouring, at the expense of high computational power requirement[40,41]. Deep learning based auto segmentation, most commonly with convolutional neural networks algorithm, provides robust and consistent lymph node segmentation tasks in head and neck regions[41,42]. Using the automated approach for segmentation and radiomic feature extraction, it would pave the way for better radiomics model generalizability.
Factors that affect the radiomics variabilities due to image acquisition are collectively known as the batch effect[43]. The protocol of medical imaging taken for NPC could be different among different centers. This heterogeneity predisposes the difficulty in the standardization of protocol development. In addition, the toolboxes for image pre-processing and radiomic feature definitions may lead to unwanted variations, affecting the generalizability of the model produced.
FUTURE DIRECTION
There is so far no consensus to interpret the NPC nodal metastasis within the imaging study - whether the number of lymph nodes, its size, or the radiological features of the malignant nodal lesion (e.g., the presence of extra-nodal extension) that would affect the radiomic model. The major future directions of radiomics studies are to address the issue of a batch effect in image acquisition and feature extraction standardization, and ultimately to improve radiomics reproducibility and generalizability[14].
Approaches to imaging standardization
It has been found that radiomic feature repeatability is largely variable with image acquisition, especially for textural features[44]. Much work has been done to minimize the variations in the acquisition and reconstruction of images before feature extraction. One of which is the standardization of image acquisition protocol in CT and PET/CT imaging[45,46]. The current challenge is that standardization is only emphasized on basic quantitative measurements, such as the standardized uptake values (SUVs), but not for the more complicated features of radiomics analysis. Moreover, in MRI there are no existing guidelines and the images produced are not quantitative[47]. It is hoped that a more standardized and reproducible imaging workflow will be developed shortly, thus improving generalizability. MRI fingerprinting demonstrates the capability to reproduce quantitative measurements of tissue properties by mapping the unique signal evolutions, i.e., “fingerprint”, with a dictionary through a pattern-matching process. If the issue of getting a widely recognized mapping dictionary were being solved, MRI fingerprinting would be a key step to solving the challenge of imaging standardization[48].
Approaches to feature standardization
Given that the existing imaging acquisition is not standardized, researchers seek different approaches to enhance feature reproducibility. In earlier studies, researchers addressed this by performing test-retest stability investigations[49]. By doing so, researchers selected only those features that were “robust” enough to be included in the modeling. However, this approach may not help to improve the issue of feature reproducibility, instead, uncovered its variability. The majority of CT-based radiomic features were not reproducible even when the images were acquired under the same imaging protocol[50]. One of the widely used methods to improve feature reproducibility is called Combine Batches (ComBat), a method to remove the batch effect using a statistical approach. It has been shown to be useful in reducing the radiomic features that are significantly affected by the batch effect[51]. The use of ComBat is still under development as researchers recognized its limitations. These include the incompatability of datasets from unknown imaging parameters[52]. Also, ComBat is only capable of handling one batch effect at a time, which may not be able to address the multifaceted and complicated batch effect due to variations in imaging parameters. To address this, a workflow combining ComBat and a test-retest approach has been suggested, and applying ComBat in reproducible features in test-retest[53]. By doing so, the radiomics robustness could be further improved.
The future directions of radiomics study lie in optimizing the reproducibility and repeatability of feature extraction. In addition, with the development of a globally recognized protocol for quantitative scans and the statistical methods to facilitate robustness, radiomics could become an efficient tool for clinical use and improved management of advanced stage NPC patients with nodal metastasis.
CONCLUSION
This review presented a summary of the vast applications of artificial intelligence in using radiomics and deep learning analysis on lymph node metastasis for advanced NPC. With the emerging technologies in the radiomic features applications, deep learning models have been readily developed and validated with good accuracy in auto-segmentation for tumor staging and treatment planning; risk-stratification for providing more personalized treatment options, and predicting the overall survival and disease-free survival.
DECLARATIONS
AcknowledgmentsWe thank Dr. Rizwan Ullah for polishing the language.
Authors’ contributionsCollected the data, contributed data and analysis tools, performed the analysis and interpretation, wrote the paper: Chan PL
Collected the data, contributed data and analysis tools, performed the analysis, wrote the paper: Leung WS
Contributed data and analysis tools, performed the analysis and interpretation, wrote the paper: Vardhanabhuti V
Contributed data and analysis tools, performed the analysis and interpretation, provide administrative and technical support, editing and language support: Lee SWY
Conception and design of the study, provide administrative, technical , material support, editing and language support: Chan JYK
Availability of data and materialsNot applicable.
Financial support and sponsorshipNone.
Conflicts of interestAll authors declared that there are no conflicts of interest.
Ethical approval and consent to participateNot applicable.
Consent for publicationNot applicable.
Copyright© The Author(s) 2023.
REFERENCES
1. Nasopharyngeal cancer statistics. Available from: https://www.wcrf.org/cancer-trends/nasopharyngeal-cancer-statistics [Last accessed on 17 Mar 2023].
2. Centre for Health Protection. department of health - nasopharyngeal cancer. 2022. Available from: https://www.chp.gov.hk/en/healthtopics/content/25/54.html [Last accessed on 20 Mar 2023].
3. Pan JJ, Ng WT, Zong JF, et al. Proposal for the 8th edition of the AJCC/UICC staging system for nasopharyngeal cancer in the era of intensity-modulated radiotherapy. Cancer 2016;122:546-58.
4. Lee AW, Sze WM, Au JS, et al. Treatment results for nasopharyngeal carcinoma in the modern era: the Hong Kong experience. Int J Radiat Oncol Biol Phys 2005;61:1107-16.
5. Ho FC, Tham IW, Earnest A, Lee KM, Lu JJ. Patterns of regional lymph node metastasis of nasopharyngeal carcinoma: a meta-analysis of clinical evidence. BMC Cancer 2012;12:98.
6. Li S, Deng YQ, Zhu ZL, Hua HL, Tao ZZ. A comprehensive review on radiomics and deep learning for nasopharyngeal carcinoma imaging. Diagnostics 2021;11:1523.
7. Ng WT, But B, Choi HCW, et al. Application of artificial intelligence for nasopharyngeal carcinoma management - a systematic review. Cancer Manag Res 2022;14:339-66.
8. Zhong LZ, Fang XL, Dong D, et al. A deep learning MR-based radiomic nomogram may predict survival for nasopharyngeal carcinoma patients with stage T3N1M0. Radiother Oncol 2020;151:1-9.
9. Xia C, Chen Y, Vardhanabhuti V. Primary tumour and lymph node radiomics assessment in PET-CT in non-metastatic nasopharyngeal carcinoma patients. In European Congress of Radiology (ECR). Germany: European Society of Radiology/SpringerOpen; 2020. Available from: http://www.springer.com/medicine/radiology/journal/13244 [Last accessed on 20 Mar 2023].
10. Mccarthy J, Hayes P. Some philosophical problems from the standpoint of artificial intelligence. In: Webber BL, Nilsson NJ, editors. Readings in artificial intelligence. Burlington, USA: Morgan Kaufmann; 1981, pp. 431-50.
11. Luger GF. Artificial intelligence: structures and strategies for complex problem solving, 6th ed. Pearson Addison-Wesley; 2009. Available from: http://www.uoitc.edu.iq/images/documents/informatics-institute/exam_materials/artificial%20intelligence%20structures%20and%20strategies%20for%20%20complex%20problem%20solving.pdf [Last accessed on 17 Mar 2023].
12. Erickson BJ, Korfiatis P, Akkus Z, Kline TL. Machine learning for medical imaging. Radiographics 2017;37:505-15.
13. Anwar SM, Majid M, Qayyum A, Awais M, Alnowami M, Khan MK. Medical image analysis using convolutional neural networks: a review. J Med Syst 2018;42:226.
14. Park JE, Park SY, Kim HJ, Kim HS. Reproducibility and generalizability in radiomics modeling: possible strategies in radiologic and statistical perspectives. Korean J Radiol 2019;20:1124-37.
15. Wagner MW, Namdar K, Biswas A, Monah S, Khalvati F, Ertl-Wagner BB. Radiomics, machine learning, and artificial intelligence-what the neuroradiologist needs to know. Neuroradiology 2021;63:1957-67.
16. Lambin P, Rios-Velazquez E, Leijenaar R, et al. Radiomics: extracting more information from medical images using advanced feature analysis. Eur J Cancer 2012;48:441-6.
17. Bogowicz M, Tanadini-Lang S, Guckenberger M, Riesterer O. Combined CT radiomics of primary tumor and metastatic lymph nodes improves prediction of loco-regional control in head and neck cancer. Sci Rep 2019;9:15198.
18. Lee CK, Jeong SH, Jang C, et al. Tumor metastasis to lymph nodes requires YAP-dependent metabolic adaptation. Science 2019;363:644-9.
19. Li S, Wang K, Hou Z, et al. Use of radiomics combined with machine learning method in the recurrence patterns after intensity-modulated radiotherapy for nasopharyngeal carcinoma: a preliminary study. Front Oncol 2018;8:648.
20. Yu TT, Lam SK, To LH, et al. Pretreatment prediction of adaptive radiation therapy eligibility using MRI-based radiomics for advanced nasopharyngeal carcinoma patients. Front Oncol 2019;9:1050.
21. Kang L, Niu Y, Huang R, et al. Predictive value of a combined model based on pre-treatment and mid-treatment mri-radiomics for disease progression or death in locally advanced nasopharyngeal carcinoma. Front Oncol 2021;11:774455.
22. Lam SK, Zhang Y, Zhang J, et al. Multi-organ omics-based prediction for adaptive radiation therapy eligibility in nasopharyngeal carcinoma patients undergoing concurrent chemoradiotherapy. Front Oncol 2021;11:792024.
23. Lam SK, Zhang J, Zhang YP, et al. A multi-center study of CT-based neck nodal radiomics for predicting an adaptive radiotherapy trigger of ill-fitted thermoplastic masks in patients with nasopharyngeal carcinoma. Life 2022;12:241.
24. Registry, HKC. Report of Stage-specific surival of nasopharyngeal cancer in Hong Kong 2019. Available from: https://www3.ha.org.hk/cancereg/pdf/survival/Stage-specific%20Survival%20of%20NPC%20in%20HK.pdf [Last accessed on 17 Mar 2023].
25. Xu H, Liu J, Huang Y, Zhou P, Ren J. MRI-based radiomics as response predictor to radiochemotherapy for metastatic cervical lymph node in nasopharyngeal carcinoma. Br J Radiol 2021;94:20201212.
26. Wang Y, Li C, Yin G, et al. Extraction parameter optimized radiomics for neoadjuvant chemotherapy response prognosis in advanced nasopharyngeal carcinoma. Clin Transl Radiat Oncol 2022;33:37-44.
27. Yang K, Tian J, Zhang B, et al. A multidimensional nomogram combining overall stage, dose volume histogram parameters and radiomics to predict progression-free survival in patients with locoregionally advanced nasopharyngeal carcinoma. Oral Oncol 2019;98:85-91.
28. Ming X, Oei RW, Zhai R, et al. MRI-based radiomics signature is a quantitative prognostic biomarker for nasopharyngeal carcinoma. Sci Rep 2019;9:10412.
29. Bologna M, Corino V, Calareso G, et al. Baseline MRI-radiomics can predict overall survival in non-endemic ebv-related nasopharyngeal carcinoma patients. Cancers 2020;12:2958.
30. Zhang F, Zhong LZ, Zhao X, et al. A deep-learning-based prognostic nomogram integrating microscopic digital pathology and macroscopic magnetic resonance images in nasopharyngeal carcinoma: a multi-cohort study. Ther Adv Med Oncol 2020;12:1758835920971416.
31. Chen X, Li Y, Li X, et al. An interpretable machine learning prognostic system for locoregionally advanced nasopharyngeal carcinoma based on tumor burden features. Oral Oncol 2021;118:105335.
32. Qiang M, Li C, Sun Y, et al. A prognostic predictive system based on deep learning for locoregionally advanced nasopharyngeal carcinoma. J Natl Cancer Inst 2021;113:606-15.
33. Zhang L, Wu X, Liu J, et al. MRI-based deep-learning model for distant metastasis-free survival in locoregionally advanced nasopharyngeal carcinoma. J Magn Reson Imaging 2021;53:167-78.
34. Aussem A, de Morais SR, Corbex M. Analysis of nasopharyngeal carcinoma risk factors with Bayesian networks. Artif Intell Med 2012;54:53-62.
35. Lundberg SM, Lee SI. A unified approach to interpreting model predictions. In Proceedings of the 31st International Conference on Neural Information Processing Systems. Long Beach, California, USA. 2022. Available from: https://dl.acm.org/doi/10.5555/3295222.3295230#sec-cit [Last accessed on 17 Mar 2023].
36. Du R, Lee VH, Yuan H, et al. Radiomics model to predict early progression of nonmetastatic nasopharyngeal carcinoma after intensity modulation radiation therapy: a multicenter study. Radiol Artif Intell 2019;1:e180075.
37. Chao KS, Bhide S, Chen H, et al. Reduce in variation and improve efficiency of target volume delineation by a computer-assisted system using a deformable image registration approach. Int J Radiat Oncol Biol Phys 2007;68:1512-21.
38. Stapleford LJ, Lawson JD, Perkins C, et al. Evaluation of automatic atlas-based lymph node segmentation for head-and-neck cancer. Int J Radiat Oncol Biol Phys 2010;77:959-66.
39. Zhou JY, Fang W, Chan KL, Chong VF, Khoo JB. Extraction of metastatic lymph nodes from MR images using two deformable model-based approaches. J Digit Imaging 2007;20:336-46.
40. Yang J, Beadle BM, Garden AS, et al. Auto-segmentation of low-risk clinical target volume for head and neck radiation therapy. Pract Radiat Oncol 2014;4:e31-7.
41. Cardenas CE, Beadle BM, Garden AS, et al. Generating high-quality lymph node clinical target volumes for head and neck cancer radiation therapy using a fully automated deep learning-based approach. Int J Radiat Oncol Biol Phys 2021;109:801-12.
42. Men K, Chen X, Zhang Y, et al. Deep deconvolutional neural network for target segmentation of nasopharyngeal cancer in planning computed tomography images. Front Oncol 2017;7:315.
43. Johnson WE, Li C, Rabinovic A. Adjusting batch effects in microarray expression data using empirical Bayes methods. Biostatistics 2007;8:118-27.
44. Da-Ano R, Visvikis D, Hatt M. Harmonization strategies for multicenter radiomics investigations. Phys Med Biol 2020;65:24TR02.
45. Boellaard R, Delgado-Bolton R, Oyen WJ, et al. FDG PET/CT: EANM procedure guidelines for tumour imaging: version 2.0. Eur J Nucl Med Mol Imaging 2015;42:328-54.
46. Kaalep A, Sera T, Rijnsdorp S, et al. Feasibility of state of the art PET/CT systems performance harmonisation. Eur J Nucl Med Mol Imaging 2018;45:1344-61.
47. Schick U, Lucia F, Dissaux G, et al. MRI-derived radiomics: methodology and clinical applications in the field of pelvic oncology. Br J Radiol 2019;92:20190105.
48. Fujita S, Hagiwara A, Yasaka K, et al. Radiomics with 3-dimensional magnetic resonance fingerprinting: influence of dictionary design on repeatability and reproducibility of radiomic features. Eur Radiol 2022;32:4791-800.
49. Aerts HJ, Velazquez ER, Leijenaar RT, et al. Decoding tumour phenotype by noninvasive imaging using a quantitative radiomics approach. Nat Commun 2014;5:4006.
50. Berenguer R, Pastor-Juan MDR, Canales-Vázquez J, et al. Radiomics of CT features may be nonreproducible and redundant: influence of CT acquisition parameters. Radiology 2018;288:407-15.
51. Mahon RN, Ghita M, Hugo GD, Weiss E. ComBat harmonization for radiomic features in independent phantom and lung cancer patient computed tomography datasets. Phys Med Biol 2020;65:015010.
52. Horng H, Singh A, Yousefi B, et al. Generalized ComBat harmonization methods for radiomic features with multi-modal distributions and multiple batch effects. Sci Rep 2022;12:4493.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Chan PL, Leung WS, Vardhanabhuti V, Lee SWY, Chan JYK. Review on applications of metastatic lymph node based radiomic assessment in nasopharyngeal carcinoma. J Cancer Metastasis Treat 2023;9:6. http://dx.doi.org/10.20517/2394-4722.2022.100
AMA Style
Chan PL, Leung WS, Vardhanabhuti V, Lee SWY, Chan JYK. Review on applications of metastatic lymph node based radiomic assessment in nasopharyngeal carcinoma. Journal of Cancer Metastasis and Treatment. 2023; 9: 6. http://dx.doi.org/10.20517/2394-4722.2022.100
Chicago/Turabian Style
Chan, Po Ling, Wan Shun Leung, Varut Vardhanabhuti, Shara W. Y. Lee, Jason Y. K. Chan. 2023. "Review on applications of metastatic lymph node based radiomic assessment in nasopharyngeal carcinoma" Journal of Cancer Metastasis and Treatment. 9: 6. http://dx.doi.org/10.20517/2394-4722.2022.100
ACS Style
Chan, PL.; Leung WS.; Vardhanabhuti V.; Lee SWY.; Chan JYK. Review on applications of metastatic lymph node based radiomic assessment in nasopharyngeal carcinoma. J. Cancer. Metastasis. Treat. 2023, 9, 6. http://dx.doi.org/10.20517/2394-4722.2022.100
About This Article
Copyright
Data & Comments
Data

 Cite This Article 8 clicks
Cite This Article 8 clicks










Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.