Spinal AV Fistula Disconnection
This is a preview. Check to see if you have access to the full video. Check access
Microsurgical Management of L1 Arteriovenous Fistula
Please note the relevant information for patients suffering from dural arteriovenous fistula is presented in another chapter. Please click here for patient-related content.
Overall, spinal vascular malformations (SVMs) are relatively rare lesions that make up an estimated 10% of all central nervous system vascular malformations. These vascular lesions are classified according to their vascular angioarchitecture and nidal location. Spinal dural arteriovenous fistulas (sDAFs) represent the most common type of SVM (50-85%).
Spinal dural arteriovenous fistulas are a heterogeneous group of predominantly acquired pathologic vascular malformations that are defined by an abnormal connection between an artery and a vein.
The pathogenesis of sDAVFs is yet to be fully elucidated, conversely to their intracranial counterparts, in which dural venous thrombosis and neoangiogenesis contribute to the abnormal recanalization of the primitive direct connections between the arteries and veins around the major dural venous sinuses. For a detailed discussion about intracranial DAVFs, please refer to the Principles of Dural Arteriovenous Fistulas chapter.
| Type | Description |
| I | Spinal dural arteriovenous fistulas (sDAVFs)(previously called angioma racemosum venosum): located at the dural sleeve of a spinal root, associated with a single-coiled vessel on the dorsal pial surface of the spinal cord |
| II | Glomus AVMs (previously called angioma racemosum arteriovenosum): characterized by a true intramedullary nidus and arteriovenous shunting occurring deep into the pia |
| III | Metameric or juvenile AVMs (previously called Cobb syndrome): involves one or more metameres (and consequently portions of the neural tissue, dura, bone, muscle, and skin) |
| IV | Direct or perimedullary AVFs (PAVFs): direct arteriovenous fistulas, usually supplied by the anterior spinal artery, drainage through the pial venous network resulting in aneurysmal dilation of the draining veins |
In 2002, another modification of the above four-tiered classification system was proposed that also considers additional pathophysiologic categories, such as neoplastic vascular lesions, and provides a detailed description of the anatomic characteristics of different SVMs according to their relation to the dura mater.
| Class | Description |
| Neoplastic vascular lesions |
Hemangioblastomas Cavernomas |
| Spinal cord aneurysms | |
| Arteriovenous fistulas |
Extradural Intradural
|
| Arteriovenous malformations |
Extradural-intradural (type III) Intradural
|
In this chapter, I will discuss presentation, management, and surgical nuances for disconnection of the most common dorsal intradural spinal dAVFs, and I will briefly review the technical variations required to manage ventral spinal and extradural dAVFs.
Clinical Presentation and Pathophysiology
Type I lesions, spinal dural arteriovenous fistulas (sDAVFs), are the most commonly found SVMs. They are also referred to as Foix-Alajouanine syndrome, originally described in 1926. Pathophysiologically, sDAVFs are characterized by a low-flow abnormal connection between an anterior or posterior radiculomeningeal arterial branch and a medullary or radicular vein. The shunt is often located near the dura mater around the intervertebral foramen and adjacent to the dorsal nerve root sensory ganglion.
More than 90% of DAVFs are thoracolumbar lesions (from T4 to L3) and affect men five times more often than women. Approximately 15% of these lesions derive their vascular supply from the internal iliac arteries, and 5-15% from the intercostal arteries. Dural AVFs are subclassified based on the number of their feeding vessels. Type A lesions have a single feeding vessel, and type B lesions are nourished by more than one feeding vessel.
At diagnosis, patients are usually in the sixth decade of life (with a mean age of 50-60 years). Spinal trauma, represented by a vertebral fracture, or spinal surgery has been implicated as the cause in up to 20% of these patients.
There are four recognized pathophysiologic mechanisms for the presentation of spinal cord vascular anomalies: 1) venous hypertension, 2) vascular steal syndrome, 3) subarachnoid hemorrhage, and 4) intraparenchymal hemorrhage (hematomyelia). Focal or global venous hypertension is the most important mechanism for symptomatic presentation of dorsal spinal dAVFs. The low-flow volume fistula results in heightened intravascular pressure within the downstream venous plexus. This phenomenon reduces the pressure gradient between the arterial and venous vasculature, resulting in diminished perfusion and subsequent spinal cord hypoxia.
Symptoms usually have an insidious and progressive course of neurologic decline and functional disability over the course of months to years, but progression with interim remissions and acute exacerbations has also been observed.
Alternatively, these patients may also present with nonspecific signs or symptoms. Patients commonly suffer from various combinations of thoracolumbar pain with or without radiculopathy (20-50%), progressive parapresis (60-75%) and bladder/bowel dysfunction (40-63%). The typical patient is a middle-aged or older gentleman with progressive lower extremity complaints, which are exacerbated during standing or walking and relieved by sitting.
Postural changes, Valsalva maneuver and exertion including physical exercise can lead to exacerbation of symptoms. This phenomenon may be related to increased intra-abdominal and intrathoracic gradients that lead to increased vena caval pressures that ultimately translates into higher intraspinal venous pressures.
Acute deteriorations are uncommon in the scope of sDAVFs, but may occur as a result of subarachnoid hemorrhage or spinal cord infarction. Cervical sDAVF should be included in the differential diagnosis of angiographically negative intracranial subarachnoid hemorrhage, especially if neck pain was reported at the onset of symptoms or if the subarachnoid blood connects into the space around the craniocervical junction and spinal cord. In such cases, the vertebral arteries should be carefully investigated during vascular imaging.
Spinal cord infarction is, on the other hand, the pathological end-stage of the disease and is associated with acute/subacute deterioration in about 15% of patients.
The differential diagnosis for the above symptoms and signs is extensive, and one should consider other etiologies that present in a similar manner, including spinal cord tumors or demyelinating conditions. The lumbosacral pain is often improved with motion or changes in position, leading one to consider the misdiagnosis of spinal stenosis or herniated disk syndromes. Similar signs may be caused by an AVM, but the patient’s age at presentation is a relatively reliable distinguishing factor between these two lesions, with AVMs usually occurring in patients age 15 to 40 years old.
More often, due to its rarity and under-recognition, a dAVF is not considered in the initial differential diagnosis of spinal cord disorders, and the patient undergoes unnecessary spinal procedures or is deprived of appropriate treatment.
Figure 1: A schematic representation of the angioarchitecture of spinal dural arteriovenous fistulas (type I) is shown. Note the fistulous connections within the dural root sleeve. Multiple connections are usually present; the surgical target it the draining vein as it forms at the inner dural surface and approaches the spinal cord.
Type IV lesions are also known as perimedullary arteriovenous malformations or fistulas (PAVFs). They are characterized by an abnormal arteriovenous shunt on the pial surface of the spinal cord. A precise epidemiology is yet to be determined. PAVFs may represent up to 15% of all SVMs.
PAVFs are considerably more rare than sDAVFs, have no gender predilection, affect patients between the third and fourth decade of life, and generally occur in the conus/cauda equina region (~80% of cases). This class of malformation can affect the proximal cauda equina segments, precluding a complete nidal resection. When occurring in the cervical and thoracic spinal segments (~20% of cases), they are commonly fed by the branches of the anterior and posterior spinal arteries, resulting in giant venous dilatations or varices.
Further subclassification into types IVa, IVb, and IVc is based on single or multiple feeding arteries and giant lesions, respectively. The abnormal connection is commonly encountered on the ventral surface of the spinal cord (~45%), the filum terminale (~28%), or the surface of the ventral root (~18%). Symptoms are also insidious, as illustrated in type I lesions, but acute deterioration may be observed in up to one-quarter of the patients (subarachnoid hemorrhage).
Figure 2: Schematic representation of glomus (type II, top row) juvenile (type III, bottom row left) and perimedullary (type IV, bottom row right) dural arteriovenous fistulas. Note the large serpiginous dilated varices.
Diagnosis and Evaluation
A high index of suspicion for this class of vascular lesions and their inclusion in the differential diagnosis list are key issues for diagnosis, especially after excluding degenerative, neoplastic and demyelinating entities.
Magnetic resonance (MR) imaging is usually the first imaging study for investigation of SVMs. The extent of diffuse engorged venous congestion associated with sDAVFs on the posterior surface of the spinal cord may correlate with the intensity of the hyperintense cord signal (edema). The absence of T2 hyperintensity is rare. Spinal cord edema may be the only imaging finding, and therefore the physician must maintain a high index of suspicion in order not to overlook a sDAVF.
Contrast enhancement occurs rather infrequently, and is usually heterogeneous. Ring enhancement is considered rare, but when present, it poses a significant diagnostic challenge by raising the suspicion of a spinal cord tumor.
PAVFs present more obvious serpentine flow void patterns and some areas of spinal cord focal expansion, representing spinal cord edema or acute/subacute intramedullary hemorrhage. Globular-shaped flow voids indicate aneurysms or venous varices.
MRI findings are useful for diagnosis, but do not detect the location of the fistulous point; therefore, angiographic studies are always necessary. New MR angiography (MRA) protocols, such as fast contrast-enhanced and CT angiography, are able to precisely detect the level of the fistulous connection in approximately 80% of patients. The MRA can sensitively detect the presence of early venous filling during the first pass of the contrast agent, and thereby can confirm or estimate the presence and the spinal level of a dAVF.
Spinal angiography is required for most patients and is still considered the gold standard. Noninvasive angiography has at least a complimentary role by guiding a focused angiogram and by potentially reducing the examination time, patient exposure to radiation, contrast load, and procedural risks.
Digital subtraction spinal angiography confirms the diagnosis and evaluates the angioarchitecture of a dAVF. This modality is important for precise localization of the pathology and surgical or endovascular planning. The study must accurately identify all of the contributing arterial feeding vessels and the draining venous system. Delayed venous return following injection of the anterior spinal artery suggests venous hypertension and increases the likelihood of diagnosing a fistula.
The angiogram should evaluate the emergence of the artery of Adamkiewicz and the premature appearance of or stasis within the intraspinal venous system, followed by selective examination of the dorsal and intercostal arteries. The T2-signal changes within the cord, and the location of venous engorgement do not reliably correlate with the rostrocaudal level of the fistula. Negative examinations require bilateral catheterization of the internal iliac arteries.
Rarely, spinal dAVFs can be complex and engage feeding vessels from more than one spinal level. These lesions may also occur around the craniocervical junction and lead to brainstem edema or ischemia (vascular “steal” phenomenon).
Figure 3: A 52-year-old man presented with a brief episode of paraparesis and underwent MR imaging. The initial lumbar MR demonstrated no remarkable findings except a questionable increase in the extent of vascularity along the dorsal conus medullaris (left upper image, arrow). Thoracic imaging disclosed additional hypervascularity within the dorsal intradural space (right upper image). Catheter angiography identified an L1 dAVF with a large midline arterialized vein on the dorsal surface of the cord (second row of images; the red arrow demonstrates the fistula and the blue arrow shows the arterialized vein on the cord). Intraoperative exploration identified the fistulous vein on the dorsal surface of the L1 nerve root (third row of images; the root is at the tip of the suction device). Intraoperative disconnection was performed following temporary clip ligation and coagulation of the vein (bottom row of images). The clip was removed to allow for watertight closure of the dura.
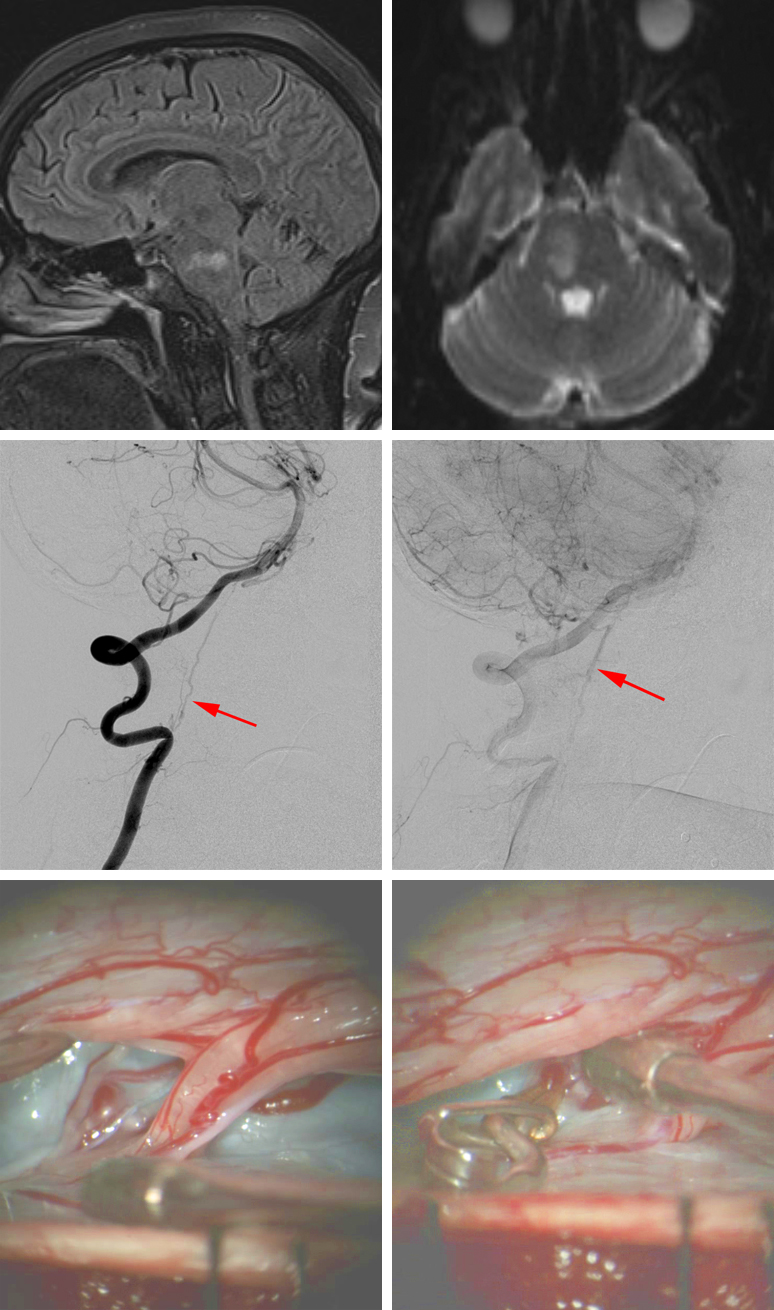
Figure 4: A 54-year-old woman presented with an acute onset of left hemiparesis and diplopia. MR imaging suggested enlarging ischemic infarction of the right inferior pons (top row of images). Cervical and cerebral angiography demonstrated a sDAVF arising from the right vertebral artery (second row of images, arrows) originating from the right C3 segmental branch of the artery with medullary venous outflow draining in a cephalad direction along the cervical spinal cord and brainstem. The patient underwent a cervical laminectomy and dAVF disconnection. Intraoperative findings noted three fistulous vessels arising anteriorly adjacent to the C2 nerve root; all of these vessels were coagulated and cut. A temporary clip was used to ensure no change in the spinal cord responses on neurophysiologic monitoring before transection of the arterialized veins (third row of images). The fistulous vessels were disconnected at the level of the dorsal nerve root. The patient experienced a progressive improvement in her hemiparesis after surgery. Follow-up 6-month MR imaging after surgery demonstrated no additional areas of ischemia.
Figure 5: Sagittal MR imaging (left) and anteroposterior angiogram (right) demonstrated a perimedullary arteriovenous malformation. Note the large varices and the widespread serpiginous perimedullary flow voids around the conus medullaris. This patient underwent curative embolization of this malformation. Resection of this malformation can be challenging because of the involvement of the cauda equina.
Treatment Paradigms
The treatment of both sDAVFs and PAVFs is multidisciplinary and involves microsurgical disconnection of the arterialized vein(s) and/or endovascular liquid embolization of the arterial feeder(s) and/or the draining vein. Microsurgery has continued to maintain its omnipresence as the method of choice for definitive fistula interruption, but recent advances in the therapeutic armamentarium of endovascular techniques have expanded their indication in the management of these fistulas.
In contrast to some of their relatively inaccessible intracranial counterparts, sDAFs remain easily reachable via microsurgery.
Microsurgery is a good option because: 1) sDAVFs and PAVFs have small and elongated low-flow vessels which impair catheter navigability and selective catheterization so that the fistulous point cannot be reliably reached; 2) the association of the fistulous-feeding arteries to the main spinal cord vascular supply (anterior spinal artery, posterior spinal artery, and the artery of Adamkiewicz) increases the risk of spinal cord ischemia by means of endovascular methods; and 3) the dorsal position of most spinal fistulas makes them readily accessible by surgery.
The goal of treatment is to arrest the progression of neurologic deficits and reverse them by endovascularly occluding the shunting zone (distal extent of the arterial feeders and proximal extent of the venous drainage) or surgically occluding the intradural arterialized vein distal to the shunting zone or ablating the fistulous nidus.
Observation is seldom indicated because of the significant morbidity associated with progression of the disease.
Early intervention prior to development of disabling symptoms is associated with good neurologic recovery. The recovery of function occurs in a specific sequence; motor function returns first, followed by sensory function, and then bowel, bladder, and sexual function. However, in patients who undergo occlusion of their vascular shunt zone, only two-thirds will experience some improvement in their motor deficits, and one-third will demonstrate a similar effect in sensory dysfunction.
Even less frequently, patients experience improvement in bowel, bladder, and sexual function. Worsening of symptoms following the initial postoperative improvement may be a sign of recanalization (following endovascular intervention) or formation of a secondary shunt.
The physician’s decision-making process for selection of the final mode of therapy requires consideration of the angioarchitecture/extent of the lesion and the surgical/endovascular expertise available at the treating facility. Microsurgical disconnection is often the most durable and effective option for patients with type I DAVFs.
Alternative Approaches
Endovascular therapy has been employed more frequently in the Onyx era and has been indicated as the treatment of choice for sDAVFs by some colleagues. These colleagues have attempted endovascular therapy as the first strategy during spinal angiogram. Surgical treatment is then reserved if embolization is not feasible or as a second-line therapy in the case of recanalization.
Endovascular embolization potentially provides several advantages over microsurgery. These include less invasiveness and subsequent reduction in the associated operative risks. The endovascular approach also allows for the immediate institution of postoperative anticoagulation, an important consideration when progressive venous thrombosis of the spinal venous plexus is identified perioperatively.
However, this mode of therapy also carries a higher risk of iatrogenic spinal cord ischemia caused by occlusion of medullary arteries or their parent vessels. This risk is especially real when embolizing in the region of the artery of Adamkiewicz because of the vital perfusion zone of this vessel’s distal vascular territory associated with minimal collateral support.
Endovascular embolization should preferably be attempted by means of liquid embolisates at the shunting zone. Endovascular management is generally contraindicated for lesions in which the arterial pedicle providing the feeding blood supply to the fistula possesses distal arterial branches to the spinal cord.
Radiosurgery has been utilized anecdotally, and since it has not been extensively studied, it is not recommended routinely in the management of spinal fistulas.
Surgical management is clearly indicated for lesions when the following conditions are met:
- catheterization of the arterial feeder is impossible,
- an extensive network of collateral arterial supply is identified preoperatively, posing a high risk of recanalization after endovascular intervention,
- recanalization occurs after endovascular management, or
- endovascular therapy for a type I intradural ventral DAVFs may place the anterior spinal artery at risk.
I prefer the microsurgical approach for most spinal fistulas (type I) because surgery is associated with minimal risk and is definitive while preserving the collateral vessels leading to the spinal cord. Other types of spinal vascular malformations are handled on an individual basis based on their location and angioarchitecture. Intramedullary spinal cord AVMs are discussed in their own dedicated chapter.
Preoperative Considerations
Timing of surgery is a matter of controversy, however, ruptured fistulas can be disconnected on an elective basis. I usually prefer to confirm some neurological improvement in patients who have complete loss of function to justify surgical intervention.
After diagnostic imaging, patients are classified according to their functional capabilities. The main scoring system for spinal fistulas is the Aminoff-Logue disability scale.
| Type | Description of Patient |
| 0 | Normal |
| 1 | Leg weakness, abnormal stance or gait, but no restriction of motor activity |
| 2 | Restricted activity |
| 3 | Requires one cane, stick, or some support for walking |
| 4 | Requires two sticks, crutches, or walker |
| 5 | Unable to stand and confined to bed or wheelchair |
MICROSURGICAL DISCONNECTION OF SPINAL DAVF (TYPE I)
For spinal fistulas, a posterior midline approach is all that is needed for safe exposure. I prefer to use a wide laminectomy, while I take care not to disturb the capsule of the facet joint. Ligamentum flavum is removed all the way to the next bony segment cranially and caudally.
It is worthwhile to extend the laminectomy one level above and below the lesion in order to provide adequate exposure and inspection of the neighboring roots because some fistulas may occasionally involve their adjacent roots. A partial medial facetectomy and pediculectomy is usually required for management of ventral thoracic PAVFs.
Laminotomy and hemilaminectomy are potential alternatives, but not my preferred strategies.
Intraoperative localization of complex thoracic fistulas can be challenging in obese patients. I usually discuss the architecture of the lesion with the angiographer to make sure I thoroughly study the lesion structure and location before surgery. Preoperative selective catheterization of the feeding vessel and a Guglielmi detachable coil deposit within the lumen of the vessel adjacent to the respective bony pedicle is a reasonable option for intraoperative localization in select cases. In addition, various radiopaque deposits can be injected in the pedicle prior to surgery that corresponds to the affected nerve root. Such deposits are easily localizable via a lateral radiograph during surgery.
Immaculate epidural hemostasis using gelfoam powder soaked in thrombin is paramount for allowing uninterrupted pristine microsurgery after the dural opening.
Spinal dural arteriovenous fistulas are usually readily identified after dural opening via an expanded bilateral laminectomies extending to the spinolaminar junction. It is important to emphasize that the fistulous nidus itself is within the dural leaves near the nerve root sleeve; the draining vein almost always leaves the dura mater together with the dorsal nerve root on its way onto the dorsal spinal cord. Therefore, the surgical target is the draining vein (before it branches intradurally), and the goal of the operation is the disconnection or clip ligation of the main draining vein as close to the dura it pierces as possible.
Intraoperative near-infrared indocyanine green (ICG) videoangiography may be useful to confirm the location of the arterialized vein, if necessary.
Figure 6: Intraoperative ICG angiography (inset photo) demonstrates an early draining vein before any other arteries in the spinal canal are visible.
Resection or coagulation of the fistula site should be pursued when preoperative angiography identifies multiple arterialized medullary veins or for lesions that demonstrate both intradural and extradural venous engorgement. The use of intraoperative spinal angiography to confirm a complete disconnection of complex fistulas is highly advised.
Intraoperative electrophysiological monitoring using motor and sensory evoked potentials is routinely performed throughout surgery. It is especially useful during microclip temporary occlusion of the presumed fistulous vein, because any deterioration in the evoked potentials results in clip removal to avoid cord injury. This maneuver is particularly important during PAVF resection.
Interruption of the fistula leads to discoloration of the arterialized venous drainage from red to purple blue. Confirmation of surgical obliteration may be done via intraoperative fluorescence angiography (ICG or fluorescein).
The fistulous corkscrew venous drainage system on the dorsal spinal cord should also appear collapsed. It is important not to remove or manipulate these veins because their dissection will lead to cord injury.
The inner dural surface near the fistula (nerve root sleeve) is carefully inspected for other small feeding vessels. I usually coagulate the small transdural arterial feeders.
Figure 7: Intraoperative fluorescein angiography confirms complete sDAVF disconnection. The corkscrew draining vein on the conus is not enhancing in the arterial phase (black arrow), and the disconnected arterialized vein (blue arrow) appears purplish blue.
If the arterialized vein is not readily apparent upon dural opening, I inspect the suspected root circumferentially. If this search is nonrevealing, a lateral radiograph is obtained to confirm exposure of the appropriate spinal segment. As mentioned above, fluorescence angiography may also be used to detect early filling of any of the regional veins.
Microsurgical Resection of PAVFs
PAVFs or malformations are not readily identified after dural opening. The denticulate ligament is cut and retraction sutures in this ligament gently rotate the spinal cord/conus, which brings into view the lateral or anterior supply of the malformation. The gentle rotation of the cord should be performed and maintained under neuroelectrophysiologic guidance.
There are associated large venous varices near the fistula that should not be injured prematurely during dissection. The proximal cauda equina is often affected by the malformation; this finding excludes the opportunity for complete resection of the lesion. In these cases, circumferential devascularization of the malformation and coagulation of the draining veins is curative (in situ occlusion technique).
In patients with a single feeding artery from the anterior or posterior spinal arteries, a temporary clip is applied to the expected feeding artery and occlusion of the fistula is checked via intraoperative fluorescence angiography. The patency of the collateral normal spinal vessels is also evaluated. In the meantime, electrophysiologic parameters are routinely monitored to confirm the spinal cord’s integrity.
After ensuring occlusion of the fistula, the proximal portion of the draining vein is coagulated and cut so that the clip can be removed and watertight dural closure achieved. Large compressive varices may need to be reduced via bipolar coagulation or resected in an epipial fashion.
Microsurgical Resection of Extradural sDAVFs
Extradural AVFs are high-flow lesions and their surgical management carries a greater risk. These lesions require a more thorough disconnection and resection than coagulation of the arterialized medullary veins, otherwise the fistula will still persist via the arterialized epidural venous plexus.
Endovascular therapy should be considered for preoperative selective occlusion to minimize intraoperative hemorrhage. The resection plans for these lesions depends on the extent and location of the nidus.
Metameric or Juvenile AVMs
Treatment for such lesions is typically considered to be palliative, with the goal of stabilizing the lesion and the symptoms. Staged endovascular partial embolization is recommended to reduce the size of the lesion, reduce venous congestion, decrease flow, or eliminate associated aneurysms. Surgical intervention is rarely if ever safe.
Glomus AVMs
These type II malformations are typically high-flow intramedullary lesions with multiple feeding vessels arising from the anterior and posterior spinal arteries draining into the medullary veins. These lesions are true intraparenchymal AVMs and are discussed in their own dedicated chapter on Spinal Cord AVM.
Closure
The dura is closed with running sutures in a watertight manner. Duraplasty is necessary to repair the resultant dural defect if the dural edges are not readily approximated.
Postoperative Considerations
The patient is observed in the intensive care unit overnight. Steroids are weaned slowly. A postoperative angiogram is performed to confirm complete obliteration of the arteriovenous shunting.
The patient should remain flat for 24 hours postoperatively with the head of the bed gradually elevated. This maneuver can potentially decrease the risk of CSF leakage.
Follow-up imaging includes repeat angiograms 1,3,5 and 10 years after the procedure. Recurrent symptoms warrant earlier imaging.
Pearls and Pitfalls
- Spinal arteriovenous fistulas comprise a heterogeneous group of entities that share similar pathologic vascular pathoanatomy, namely abnormal connection(s) between a radiculomedullary artery and vein.
- Early treatment is recommended before severe neurologic deficits occur.
- A clear understanding of the angioarchitecture of the malformation is necessary for its effective disconnection.
Contributors: Benjamin K. Hendricks, MD, and Marcus André Acioly, MD
References
Black P. Spinal vascular malformations: an historical perspective. Neurosurg Focus. 2006;21:E11.
Ducruet AF, Crowley RW, McDougall CG, Albuquerque FC. Endovascular treatment of spinal arteriovenous malformations, in Spetzler RF, Kalani YS, Nakaji P (eds): Neurovascular Surgery. 2nd ed. New York: Thieme; 2015.
Dumont AS, Oldfield EH. Spinal vascular malformations (Chapter 397), in Winn RH (ed): Youmans Neurological Surgery, Vol 3, 6th ed, Philadelphia: Elsevier Saunders, 2011, 4167-4202.
Ferrell AS, Tubbs RS, Acakpo-Satchivi L, Deveikis JP, Harrigan MR. Legacy and current understanding of the often-misunderstood Foix-Alajouanine syndrome. Historical vignette. J Neurosurg. 2009;111:902-906.
Flores BC, Klinger DR, White JA, Batjer HH. Spinal vascular malformations: treatment strategies and outcome. Neurosurg Rev. 2016 Apr 13. [Epub ahead of print].
Kalani MA, Kalani YS, Spetzler RF. Surgical management of spinal vascular malformations, in Spetzler RF, Kalani YS, Nakaji P (eds): Neurovascular Surgery, 2nd ed. New York: Thieme; 2015.
Kim LJ, Spetzler RF. Classification and surgical management of spinal arteriovenous lesions: arteriovenous fistulae and arteriovenous malformations. Neurosurgery. 2006;59(5 Suppl 3):S195-201;discussion S3-13
Krings T, Geibprasert S. Spinal dural arteriovenous fistulas. Am J Neuroradiol 2009;30:639-648.
Kuwayama N. Epidemiologic survey of dural arteriovenous fistulas in Japan: clinical frequency and present status of treatment. Acta Neurochir Suppl. 2016;123:185-188.
Niimi Y, Berenstein A, Setton A, Kupersmith MJ. Endovascular treatment of dural arteriovenous fistulas, in Lawton M, Gress D, Higashida RT (eds): Controversies in Neurological Surgery: Neurovascular Diseases. New York: Thieme, 2006
Özkan N, Kreitschmann-Andermahr I, Goerike SL, Wrede KH, Kleist B, Stein KP, Gembruch O, Sandalcioglu IE, Wanke I, Sure U. Single center experience with treatment of spinal dural arteriovenous fistulas. Neurosurg Rev. 2015;38:683-692.
Spetzler RF, Detwiler PW, Riina HA, Porter RW. Modified classification of spinal cord vascular lesions. J Neurosurg. 2002;96(2 Suppl):145-156.
Takai K, Kurita H, Hara T, Kawai K, Taniguchi M. Influence of indocyanine green angiography on microsurgical treatment of spinal perimedullary arteriovenous fistulas. Neurosurg Focus. 2016;40:E10.
Tuchek CA, Cohen-Gadol AA. Microsurgical ligation of spinal arteriovenous fistulae: techniques. Neurosurg Focus. 2014;37 Suppl 2: Video 11.
Weiss N, Bederson J, Post K. Management of spinal cord tumors and arteriovenous malformations (Chapter 188), in Quinones-Hinojosa A (ed): Schmidek & Sweet Operative Neurosurgical Techniques, Vol 2, 6th ed, Philadelphia: Elsevier Saunders, 2012, 2135-2151.
Please login to post a comment.