Intradural Clinoidectomy Free
This is a preview. Check to see if you have access to the full video. Check access
Intradural clinoidectomy for a large paraclinoid aneurysm.
GENERAL CONSIDERATIONS
Anterior clinoidectomy is an important tool for neurovascular and skull base surgery. This technique is cardinal in expanding access to the sella, proximal carotid artery, and central skull base. The goal of anterior clinoidectomy is to the reveal the more proximal ophthalmic and clinoidal segments of the internal carotid artery (ICA) while unroofing the optic canal and skeletonizing the proximal optic nerve. This maneuver expands the optico-carotid and carotid-oculomotor access windows and therefore the operative corridor to the interpeduncular cisterns. Both the carotid artery and optic nerve are partially untethered and can be more safely and gently mobilized.
Controversy surrounds the value of clinoidectomy for “appropriately selected” cases. Moreover, there is no consensus on the indications and benefits of extradural versus intradural clinoidectomy. Many reports of modified variations of clinoidectomy have complicated the technical complexity of this osteotomy and have further dampened some of my colleagues’ enthusiasm for adopting this technique. This chapter aims to clarify and simplify the appropriate indications for clinoidectomy.
The indications and advantages of extradural clinoidectomy are:
- The extradural space allows a more “aggressive” osteotomy of the medial sphenoid wing and clinoid while protecting the intradural neurovascular structures during drilling.
- This maneuver is less selective and more inclusive for various pathologies.
- It is more beneficial for resection of medial sphenoid wing meningiomas as it allows early devascularization of the tumor and decompression of optic nerve. The tumor-infiltrated clinoid can be removed. Upon early decompression of the nerve, further tumor manipulation may not place the nerve at risk of traction injury.
- This maneuver is also used as part of the extradural middle fossa approach to the lesions of the cavernous sinus.
The indications and advantages of intradural clinoidectomy are:
- The intradural space allows limited osteotomy of the clinoid while the intradural structures are potentially at risk during drilling and are exposed to bone dust.
- This maneuver is more selective and the osteotomy can be tailored to the underlying pathology.
- It is desirable for clip ligation of ophthalmic and paraclinoid artery aneurysms since bony removal can be tailored and clinoidectomy can be executed under careful monitoring of the aneurysm to prevent manipulations that could potentially place the aneurysm at risk of intraoperative rupture. Partial clinoidectomy may also be necessary for proximal posterior communicating (P-Comm) artery aneurysms.
An intradural clinoidectomy may be associated with a smaller risk of cerebrospinal fluid (CSF) rhinorrhea for two reasons. First, by performing an early intradural inspection of the pathoanatomy, a clinoidectomy may be deemed unnecessary. Second, a partial clinoidectomy tailored to the pathology at hand may obviate the need for a complete clinoidectomy. These two factors may lead to a decreased need for osteotomy and subsequent violation of the sphenoid and even the ethmoid sinuses. The risk of oculomotor nerve injury may also be slightly decreased with extradural clinoid resection. This difference may be due to medial bone removal early in surgery during an intradural versus extradural clinoidectomy.
Adherence of the aneurysm dome to the clinoidal dura is a contraindication for extradural clinoidectomy. In addition, erosion of the clinoid by the aneurysm dome and the presence of carotidoclinoid foramen demand an intradural technique.
Ultimately, surgeon’s preference and comfort level dictates “which side of the dura” is entered to execute anterior clinoidectomy. I prefer the extradural approach due to my experience level with this procedure. I also prefer to avoid drilling within the intradural space if at all possible to minimize the risk of injury to the neighboring structures.
Note that intradural clinoidectomy can be tailored and not all the steps mentioned below are mandatory. Initial intradural inspection of the lesion dictates the need for the extent of clinoid osteotomy.
PREOPERATIVE CONSIDERATIONS
The extent of clinoid aeration (pneumatized clinoid) may be evaluated on preoperative CT scan and predicts the need for more robust plugging of the bony defect after clinoidectomy to avoid a CSF fistula. Thin-slice CT also determines the ossification of the clinoidal ligaments, specially the carticoclinoid and interclinoid ligaments. For further details on the anatomical variations of the anterior clinoid process, please refer to the Extradural Clinoidectomy chapter.
In the case of proximal paraclinoid aneurysms, control over the ICA must be established via neck dissection and the neck area is prepared, especially in the case of ruptured aneurysms.
Extension of the aneurysm neck proximal to the distal dural ring should be assessed on a preoperative CT angiogram. Although following clinoidectomy, opening of the outer dural ring provides access to additional few millimeters of aneurysm neck, significant extension of certain paraclinoid aneurysm necks into the cavernous sinus precludes the use of an open microsurgical route for clip ligation.
Figure 1: The neck of this aneurysm was partially concealed by the clinoid process. An intradural clinoidectomy was subsequently performed to disclose the neck of the aneurysm for clip application. Please refer to the images below.
OPERATIVE ANATOMY
The frontotemporal dura defines the superior and lateral borders to the clinoid while the periorbita and optic strut limit the anterior and inferior borders. The clinoid segment of the internal carotid artery (ICA) provides the posterior limit inferomedially. Inferolaterally, the neurovascular structures of the cavernous sinus lie under a layer of periosteal dura emerging anteriorly into the superior orbital fissure.
Click here to view the interactive module and related content for this image.
Figure 2: The view gained by a clinoidectomy. Note the extended view of the clinoidal segment of the ICA (left image). The proximity of the optic nerve to the clinoid places it at risk during drilling. The superior and lateral borders of the clinoid space are provided by the frontotemporal dura. The periorbita, optic strut, and sphenoid bone are the anterior and inferior limits. The relationships of other relevant vital structures (note the cranial nerves within the lateral wall of the cavernous sinus) are presented after other overlying dura and bone are removed (right image). These vital structures are at risk during mobilization of the process (Image courtesy of AL Rhoton, Jr).
Given the large number of neurovascular structures in this region, the importance of any additional created space or mobility of any nerves or key vessels is immediately apparent clinically. A major impediment to learning this technique is a lack of three-dimensional understanding of the clinoid and the surrounding vital structures. I will attempt to simplify the germane operative anatomy.
The following images emphasize three osteotomies required for disconnection of the clinoid
- Osteotomy along the medial lesser sphenoid wing to disconnect the lateral connection
- Osteotomy along the orbital roof to disconnect the anterior connection
- Drilling within the clinoid to create an “egg shell” and disconnect the anteroinferior connection to the optic strut
After the completion of the above three steps, the shell of clinoid can be mobilized and dissected away from the clinoidal ligaments.
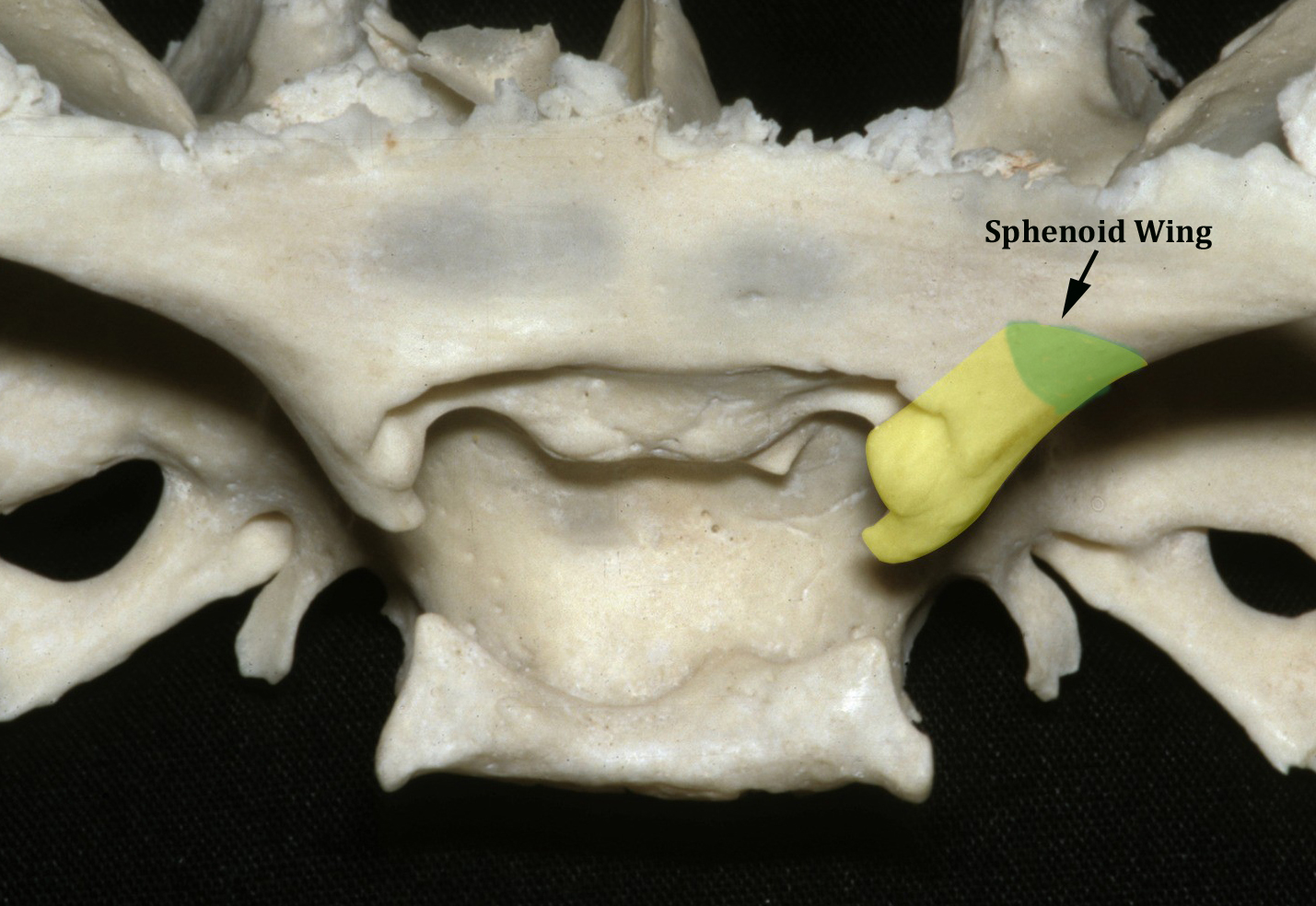
Figure 3: For an intradural clinoidectomy, the lesser sphenoid wing is removed and the superior orbital fissure may be skeletonized through the extradural approach as part of the extended pterional craniotomy (green). Therefore, the first step in intradural clinoidectomy, involving osteotomy along the sphenoid ridge to disconnect the lateral connection of the clinoid, is actually performed extradurally (Image courtesy of AL Rhoton, Jr).
Figure 4: The second step involves osteotomy along the roof of the optic nerve and frontal bone medially (pink) to disconnect the anterior and medial connections of the clinoid. This decompression of the nerve protects the nerve from any traction injury during mobilization of the clinoid. The last osteotomy comprises of drilling within the clinoid to create an “egg shell” and disconnect the anteroinferior connection to the optic strut (green). These last two steps are conducted intradurally (Image courtesy of AL Rhoton, Jr).
INTRADURAL ANTERIOR CLINOIDECTOMY
Most aneurysms and tumors arising from this region can be accessed via a standard pterional or orbitozygomatic craniotomy tailored to their specific configuration. The lesser sphenoid wing is removed and the superior orbital fissure may be skeletonized through the extradural approach as part of the standard or extended pterional craniotomy.
Figure 5: In large paraclinoid aneurysms, the Sylvian fissure is split and the optic nerve and ICA bifurcation identified. In this right-sided approach, the proximal neck of the aneurysm is often partly concealed by the anterior clinoid process. The clinoid dura is incised in a cruciate fashion; this incision may be extended more laterally or medially if necessary as dictated by the underlying pathology (inset).
Figure 6: I usually incise the dura along the lesser sphenoid wing to the edge of the prior extradural ridge resection (top image, hashed blue line). A second perpendicular dural incision may involve the falciform ligament. Retraction of the dural leaflets exposes the medial clinoid (bottom image).
Figure 7: As an alternative, dural opening can be performed over the bone on the lateral aspect of the anterior clinoid and the medial aspect of the optic canal through the falciform ligament in a rectangular or H-shaped fashion (hashed black line). The dural flap is then reflected over the neurovascular structures in order to protect them. After clinoidectomy, the dural flap is reflected back and sealed to decrease the the risk of a CSF leak (Image courtesy of AL Rhoton, Jr).
Figure 8: Using a diamond burr and constant irrigation, the clinoid process is cored out. Alternatively, an ultrasonic bone curette may be used. At this juncture, the extent of bony removal can be exactly tailored to expose the residual concealed proximal neck of the aneurysm. A thin shell of bone is left in order to maintain a safe border around the ICA and aneurysm. The medial leaflet of the dura further protects the vital structures. In this sketch, a limited medial clinoidectomy will be adequate to expose the aneurysm neck; a complete clinoidectomy is not necessary.
In the case of patients whose aneurysm is eroding through and adherent to the clinoid, a thin layer of bone is left on the aneurysm dome and the focus of attention is turned to exposing the aneurysm neck.
Figure 9: The clinoid is thoroughly cored out; this maneuver leads to disconnection of the clinoid from the optic canal and strut. The residual thin shell of bone is bluntly separated from the clinoidal ligaments and delivered. Venous bleeding from the cavernous sinus is easily controlled with a small piece of thrombin soaked gelfoam powder and gentle pressure by the cottonoid patty. The final result of this medial clinoidectomy is access to the more proximal neck of the aneurysm that is now available for clip application (top image, inset). Proximal control over the ICA was obtained at the neck.
If necessary, dissection may be continued along the walls of the ICA, the distal dural ring exposed and sectioned to access the clinoidal segment of the ICA.
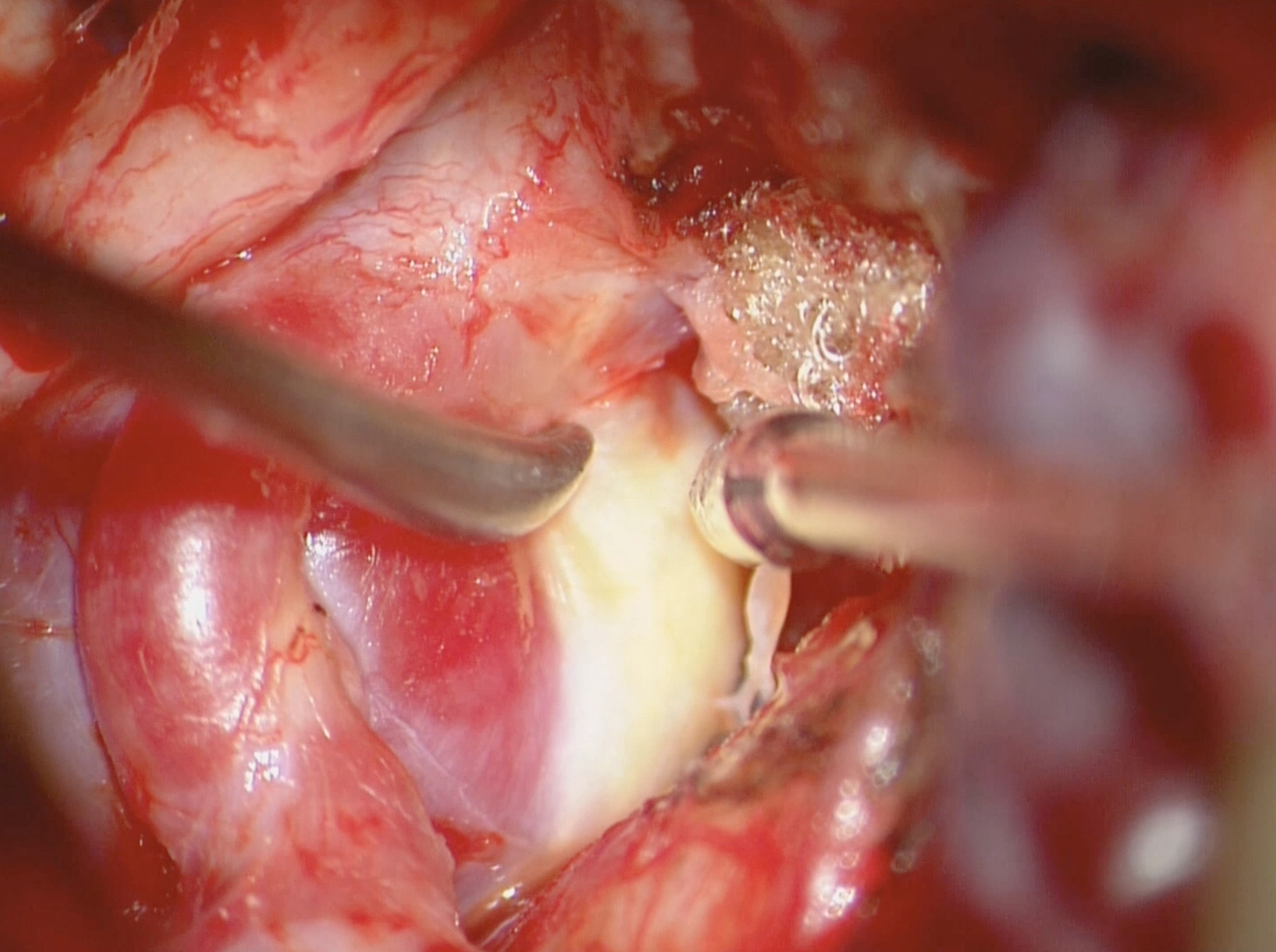
Figure 10: An intraoperative photo demonstrates access to the proximal neck of the large right-sided posterior communicating artery aneurysm.
Intradural clinoidectomy for an optic foramen meningioma.
CLOSURE
If there is concern about a pneumatized clinoid, a small piece of temporalis muscle may be placed within the defect and reinforced with a small amount of fibrin glue. The rest of the dura is closed in a standard fashion.
POSTOPERATIVE CONSIDERATIONS
The patient is monitored for CSF rhinorrhea, changes in visual acuity, and diplopia. Postoperative rhinorrhea is first managed through temporary lumbar drainage. This maneuver is often effective for cessation of the leak if the fistula is suspected at the level of clinoid resection. If not effective, the patient will be returned to the operating room for repacking of the clinoidectomy defect.
PEARLS AND PITFALLS
-
Extradural clinoidectomy is my preferred method. For paraclinoid aneurysms adherent to the dura, tumors associated with highly hyperostotic bone, or patients with ossification of clinoid ligaments, an intradural clinoidectomy or combined approach is more reasonable.
- "Egg-shelling” the medial clinoid is a safe method of performing a tailored clinoidectomy.
- Regardless of the technique used for clinoidectomy (drilling or ultrasonic bone curettes), copious irrigation is paramount to avoid thermal injury to the optic nerve.
- Once the medial clinoidectomy is performed, bony removal can be extended to the optic strut, lesser sphenoid wing and roof of the optic nerve. These maneuvers can be carried out based on the location and features of the pathology at hand.
Contributor: Marcus A. Acioly, MD, PhD
References
Rhoton AL, Jr. Aneurysms. Neurosurgery 2002;51:S121–S158.
Kulwin C, Tubbs RS, Cohen-Gadol AA. Anterior clinoidectomy: description of an alternative hybrid method and a review of the current techniques with an emphasis on complication avoidance. Surg Neurol Int 2011;2:140.
Please login to post a comment.























Comments: