Abstract
Introduction:
Foot ulcer, with a prevalence of 15% in general population, is one of the main complications in patients with diabetes. So far, different therapeutic methods have been provided for the treatment of foot ulcers. When no response to the standard treatment methods is observed, other methods would be applied.Case Presentation:
In this report, we introduce two men with type 2 diabetes mellitus and recalcitrant diabetic foot ulcer who were treated with topical 50% trichloroacetic acid solvent and autologous fibroblasts. The treatment resulted in complete healing of foot ulcers in both patients.Conclusions:
Trichloroacetic acid and autologous fibroblast can be considered as therapeutic choice for recalcitrant diabetic foot ulcer.Keywords
1. Instruction
Foot ulcer is one of the main complications of patients with diabetes mellitus (DM) with a prevalence of 15% in general population (1). Diabetic foot ulcer (DFU) is one of the health problems of patients with DM. These ulcers are resulted from impaired blood circulation in the patients and are followed by other disorders that impose high costs to the patients. Different therapeutic modalities have been provided to treat DFUs. Treatment of infections, debridement, controlling blood sugar, vascular restoration, using high-pressure oxygen, correction of foot deformities, reduction of plantar pressure, and vacuum therapy are amongst standard treatments (2). When there is no response to the standard treatments, other methods such as electric shock, application of trichloroacetic acid (TCA), and modern methods such as treatment with stem cells would be employed (3, 4). In the current report, the effect of combined therapy with TCA and autologous fibroblasts in healing DFUs of two patients were presented in details.
2. Case Presentation
2.1. Case One
The first patient was a 64-year-old man with type 2 DM and recalcitrant DFU for one year. The patient was examined regularly. To control the vascular responses, ankle-brachial index (ABI) in posterior and anterior tibialis arteries were measured, which yielded normal findings. The patient received standard treatments for DFU including administration of suitable antibiotics to control the infection, debridement, controlling blood sugar, reduction of pressure on ulcer area, and training programs to control the ulcers. Vacuum therapy was also employed. Nevertheless, the ulcers did not show any sign of healing. Therefore, he was referred to the Skin Diseases and Leishmaniasis Research Center in Isfahan, Iran. To participate in the current study, patient signed a written informed consent and his data were recorded. The patient was photographed weekly by digital camera (Canon DS126151,400D, Made in Japan) under the same conditions, and the area of his ulcers were measured by PictZar 5.05.2 software (BioVisual Technologies, New Jersey, USA) before and after the treatment. The ulcers were scored according to Table 1 (5). The scores of infected ulcers are shown in Table 2 (6). The level of healing of the ulcers was measured based on the differences in the percentage change of involved ulcer area before and after the treatment.
University of Texas Wound Classification System
| Level | Class 0 | Class 1 | Class 2 | Class 3 |
|---|---|---|---|---|
| A | lesion before or after wound without tearing the skin | superficial wound | deep wound to tendon or capsule | wound with penetration to the bone or joint |
| B | infection + | infection + | infection + | infection + |
| C | ischemia + | ischemia + | ischemia + | ischemia + |
| D | infection and ischemia | infection and ischemia | infection and ischemia | infection and ischemia |
| Parameter | 0 | 1 | 2 | 3 |
|---|---|---|---|---|
| Suppuration | no | - | - | yes |
| Nonpurulent discharge (bloody serous) | no | slight: pink, barely perceptible | mild: pale red with certain edges | severe |
| Erythema | no | slight | mild | sever: red to dark red |
| Induration | no | slight | mild | severe |
| Tenderness (sign) | no | slight | mild | severe |
| Pain (symptoms) | no | slight | mild | severe |
| Local Heat (in comparison with uninfected side of foot) | same | slightly increased | mildly increased | severely increased |
After disinfecting the ulcer, 50% TCA and 35% TCA solutions were applied around and onto the ulcer area by cotton applicator, respectively. Then the area was washed by normal saline solvent and covered by sterile gauze. The gauze was changed once a day for a week. All routine treatments and evaluations were applied and the procedure repeated for five weeks. To provide analogous fibroblasts, 4-mm2 punch biopsy was performed from the skin behind the ear to obtain skin and blood samples and transferred to the cell culture laboratory of Skin Diseases and Leishmaniasis Research Center of Isfahan, Iran, to culture the fibroblasts. At the cell culture laboratory, the fibroblasts were cultured after preparation and culturing steps. After two passages in 45 days, 6.5 million cells were injected into ulcers. To prepare the wound for cell transplantation and to remove hypertonic tissues around the ulcer, the ulcer was debrided by scalpel (No. 15) until reaching the bleeding spot. A tiny layer of fibroblast solvent was spread on the ulcer by syringe one week after TCA application and then the ulcer was covered by Mepitel dressing (Molnlycke health care AB, Finland), a nonadhesive silicon wound dressing, and Tegaderm 3M (3M Health care, D-41453, Neuss, Germany), which is a tiny layer of polyurethane with a layer of adhesive acrylic. To prevent infection, 500 mg of ciprofloxacin (twice a day) and 300 mg of clindamycin (three times a day) were administrated for 14 days. The bandage was removed on the fifth day of treatment. The diameter of ulcer was 11.44 cm with the surface area of 55.652 cm2 (class D, level 2) (Figure 1). After five weeks of TCA application, the ulcer diameter and the area decreased to 11.04 cm and 41.776 cm2, respectively (class B, level 2) (Figure 2). After applying fibroblasts, the patient was examined weekly and after two weeks, re-epithelialization and decreasing the diameter and surface area of ulcer were observed. Four weeks after applying fibroblasts, the infection score was one, the diameter of ulcer was 7.30 cm, and its surface area was 13.349 cm2 (class B, level 1). Then 50% TCA was applied around the ulcer for four weeks. Finally, the infection score changed to zero and the ulcer diameter and surface area decreased to 2.57 cm and 0.901 cm2, respectively (class A, level 1) (Figure 3). The efficiency of treatment in this patient was 98.5% and the ulcer was completely re-epithelialized (Table 4).
Patient 1 Before Treatment With Trichloroacetic Acid
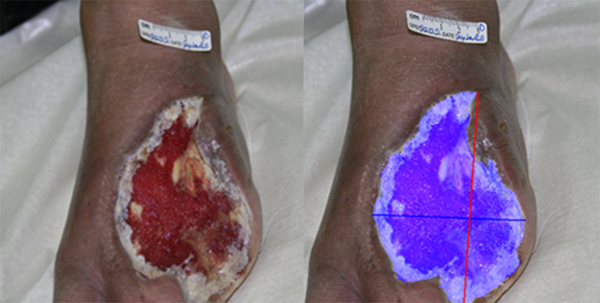
Patient 1, Five Weeks After Treatment With Trichloroacetic Acid

Patient 1, 10 Weeks After Treatment With Autologous Fibroblast

2.2. Case Two
The other patient was a 71-year-old man with type 2 DM and recalcitrant DFU for ten years. The patient was regularly examined. To control vascular responses, ABI in posterior and anterior tibialis arteries were measured and the results were within normal limits. The patient received standard treatments for DFUs including administration of suitable antibiotics to control the infection, debridement, controlling blood sugar, reduction of pressure at the ulcer area, training programs to control the ulcer, and vacuum therapy. Nonetheless, the ulcer did not show any sign of healing and therefore, he was referred to the Isfahan Skin Diseases and Leishmaniasis Research Center, Isfahan, Iran. The patient's data were recorded and a written informed consent was obtained. Every week, the patient was photographed by digital camera (Canon DS126151, 400D, Japan) under the same condition and the surface area of his ulcer was measured using PictZar 5.05.2 software before and after the treatment. The assessment of ulcer, treatment, protocol of fibroblast therapy, and evaluating healing were the same as those previously described for the case one with some small differences. In this case, the number of injecting cells was around 6.75 million after two passages during 35 days. The diameter and the surface area of the ulcer were 6.58 cm and 19.937 cm2, respectively (class D, level 2) (Figure 4). After five weeks of treatment with 50% and 35% TCA, the diameter and the surface area of the ulcer reduced to 6.21 cm and 16.307 cm2, respectively (class D, level 2) (Figure 5). After applying fibroblasts, re-epithelialization and reduction in the size of the ulcer were observed. Four weeks after fibroblasts application, the score of infection was one and the diameter of the ulcer and its surface area were respectively 5.71 cm and 9.259 cm2 (class B, level 1). Then 50% TCA was applied around the ulcer for four weeks. The final results for this patient were as follows: infection score of zero; diameter of 1.61 cm; and the surface area of 1.046 cm2 (class A, level 1) (Figure 6). The level of healing in this patient was 95% and the ulcer was re-epithelialized completely (Table 4).
| Patients | Number 1 | Number 2 |
|---|---|---|
| Age, y | 64 | 71 |
| Sex | male | male |
| Duration of diabetes, y | 1 | 5 |
| Duration of ulcer, mo | 5 | 1 |
| Class of ulcer | superficial, left foot | superficial, left foot |
| ABI | 0.90 | 0.86 |
| Location of ulcer | D | D |
| Level of ulcer | 2 | 2 |
Features of Diabetic Foot Ulcers Before and After Treatment
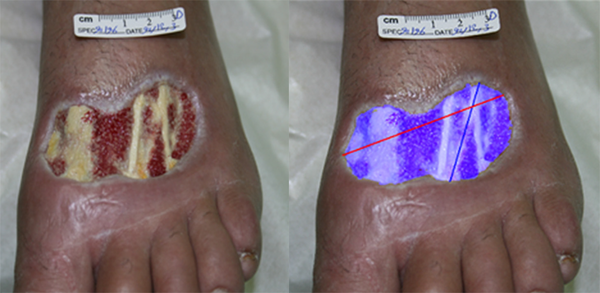
Patient 2, Before Treatment With Trichloroacetic Acid

Patient 2, Five Weeks after Treatment with Trichloroacetic Acid
Patient 2, 10 Weeks After Treatment With Fibroblast

3. Discussion
The prevalence of foot ulcers among patients with DM ranges from 4% to 10% and the lifetime incidence might be as high as 25% (7). unfortunately, the available treatment modalities for DFUs are often inadequate (8). Two patients with DM and recalcitrant to the conventional treatments ulcers were recruited to evaluate the recommended therapeutic method, ie, 50% TCA and autologous fibroblasts. Both methods were effective for the treatment of DFUs; the ulcer of one patient, which had reached the tendon, healed after ten weeks of fibroblasts application. TCA is one of the most important chemical peeling agents. Using TCA to treat recalcitrant DFUs is a new application of this chemical compound. In this regard, it has been reported that applying TCA might accelerate the process of cell regeneration after two weeks (9, 10). Stem cells, endothelial cells, and fibroblasts, either on scaffolds or as suspension, have been used to treat the ischemic DFUs. New vessels were formed due to the stimulation of growth factors and paracrine secretin receptors, which lead to the healing of the ulcer (11). A systematic review evaluated the efficiency of different therapeutic methods for DFU and reported that using cultured cutaneous fibroblast could improve nonischemic plantar ulcers during a 12-week period (3). Another randomized clinical trial reported that the level of improvement in the study group with fibroblasts application was significantly higher in comparison with the control group (12). Studies concerning the efficiency of fibroblasts on DFUs showed that the morphology of ulcers had changed during the process of healing and their proliferative capacity was reduced. Different clinical trials on the efficiency of dermagraft, a bioengineered human dermal equivalent, in chronic DFUs have reported that its significantly higher efficiency than other common methods. Using fibroblasts to treat chronic and acute ulcers relieves the pain, accelerates the healing process with fewer scars, and from another viewpoint, improves cosmetic results (13). After application of cutaneous equivalents on surgical acute ulcers, their effect on the stimulating granular tissues was confirmed and the transplanted tissue was not rejected (14). The results of the current study recommended the application of fibroblasts as an effective therapeutic modality to treat recalcitrant DFUs.
References
-
1.
Dalla Paola L, Faglia E. Treatment of diabetic foot ulcer: an overview strategies for clinical approach. Curr Diabetes Rev. 2006;2(4):431-47. [PubMed ID: 18220646].
-
2.
Aalami HB, Aalami HA, Siavashi B. Diabetic Foot Ulcer Management Review of Literature. Iran J Surgery. 2009;16(4):1-7.
-
3.
Hinchliffe RJ, Valk GD, Apelqvist J, Armstrong DG, Bakker K, Game FL, et al. A systematic review of the effectiveness of interventions to enhance the healing of chronic ulcers of the foot in diabetes. Diabetes Metab Res Rev. 2008;24 Suppl 1:S119-44. [PubMed ID: 18442185]. https://doi.org/10.1002/dmrr.825.
-
4.
Nilforoushzadeh MA, Jaffary F, Ansari N, Siadat AH, Heidari A, Adibi N. Treatment of recalcitrant diabetic ulcers using trichloroacetic acid: A case series of 6 patients. J Res Med Sci. 2012;17(5):S287-91.
-
5.
Lavery LA, Armstrong DG, Harkless LB. Classification of diabetic foot wounds. The Journal of Foot and Ankle Surgery. 1996;35(6):528-31. https://doi.org/10.1016/s1067-2516(96)80125-6.
-
6.
Knighton DR, Ciresi KF, Fiegel VD, Austin LL, Butler EL. Classification and treatment of chronic nonhealing wounds. Successful treatment with autologous platelet-derived wound healing factors (PDWHF). Ann Surg. 1986;204(3):322-30. [PubMed ID: 3753059].
-
7.
Singh N, Armstrong DG, Lipsky BA. Preventing foot ulcers in patients with diabetes. JAMA. 2005;293(2):217-28. [PubMed ID: 15644549]. https://doi.org/10.1001/jama.293.2.217.
-
8.
Margolis DJ, Allen-Taylor L, Hoffstad O, Berlin JA. Healing diabetic neuropathic foot ulcers: are we getting better? Diabet Med. 2005;22(2):172-6. [PubMed ID: 15660734]. https://doi.org/10.1111/j.1464-5491.2004.01375.x.
-
9.
Nguyen TH, Rooney JA. Trichloroacetic acid peels. Dermatol Ther. 2000;13(2):173-82. https://doi.org/10.1046/j.1529-8019.2000.00020.x.
-
10.
Nifroushzadeh MA, Jaffary F, Reiszadeh MR. Comparative Effect of Topical Trichloroacetic Acid and Intralesional Meglumine Antimoniate in the Treatment of Acute Cutaneous Leishmaniasis. Int J Pharmacol. 2006;2(6):633-6. https://doi.org/10.3923/ijp.2006.633.636.
-
11.
Ulicna M, Danisovic L, Vojtassak J. Does cell therapy and tissue engineering represent a promising treatment of diabetic foot ulcers. Bratisl Lek Listy. 2010;111(3):138-43.
-
12.
Marston WA, Hanft J, Norwood P, Pollak R, Dermagraft Diabetic Foot Ulcer Study G. The efficacy and safety of Dermagraft in improving the healing of chronic diabetic foot ulcers: results of a prospective randomized trial. Diabetes Care. 2003;26(6):1701-5. [PubMed ID: 12766097].
-
13.
Wong T, McGrath JA, Navsaria H. The role of fibroblasts in tissue engineering and regeneration. Br J Dermatol. 2007;156(6):1149-55. [PubMed ID: 17535219]. https://doi.org/10.1111/j.1365-2133.2007.07914.x.
-
14.
Gibbs S, van den Hoogenband HM, Kirtschig G, Richters CD, Spiekstra SW, Breetveld M, et al. Autologous full-thickness skin substitute for healing chronic wounds. Br J Dermatol. 2006;155(2):267-74. [PubMed ID: 16882162]. https://doi.org/10.1111/j.1365-2133.2006.07266.x.