Penetrating extremity trauma is notorious for neurovascular injuries, mandating a high index of suspicion, meticulous planning and exploration in the operating room along with assistance from other surgical specialties to avoid and tackle any complications during foreign body retrieval.
Dr. George Shaji,
Department of Orthopaedics, Father Muller Medical College and Hospital, Mangalore, Karnataka, India.
E-mail: george.shaji@gmail.com
Introduction: In penetrating injuries, neurovascular structures are the main concern as they can be damaged either at the point of injury or are at risk of iatrogenic damage during exploration. Lapse in planning and a hasty attempt at retrieval in the emergency, often results in retention of a part of the foreign body. In this case report, we emphasize the need for exploration in the operating room to prevent potential complications from missed foreign body.
Case Report: A 24-year-old motorcyclist involved in a road traffic collision was received at our trauma center, with a foreign object sticking out from his lower third right arm. On clinical exam, there were no distal neurovascular deficits. A radiograph was taken and the patient was shifted to the theater. On exploration, the foreign body was removed with gentle manipulation after careful debridement, along its path of insertion. Only localized muscle injury was noted. All the surrounding neurovascular structures were intact. At 3 weeks, wound had healed with no residual symptoms.
Conclusion: Penetrating trauma is notorious for neurovascular injuries and therefore a meticulous history taking, clinical exam, and planning is vital. Exploration in the operating room is a must for complete and safe retrieval of the foreign body.
Keywords: Penetrating trauma, foreign body, surgical exploration, retrieval.
Penetrating trauma occurs when an object pierces the skin to enter into the body tissues, creating an open wound [1]. The penetrating object may remain in the tissues, come back out the way it entered, or pass through the tissues and exit from another area [1]. Lapse in planning and a hasty attempt at retrieval in the emergency, often results in retention of a part of the foreign body. Retained foreign bodies can result in varied complications such as infection, foreign body granulomas, and soft-tissue damage [2]. Neglected foreign bodies are a common cause of malpractice claims [3]. In this case report, we emphasize the need for a high index of suspicion, meticulous planning, good patient communication, and a thorough surgical exploration and debridement in the operating room, to avoid potential complications during retrieval or from missed foreign body.
A 24-year-old motorcyclist involved in a road traffic collision was received at our trauma center, with the handle of his two-wheeler’s side mirror sticking out from a wound in the antero-medial aspect of his lower third right arm (Fig. 1). He had ongoing pain with foreign body sensation and bleeding from the wound, with restricted elbow movements. A detailed history elicited, confirmed that the side mirror had detached from the handle during the incident and there were no shattered glass pieces on his body. Patient did not have any foreign body sensations elsewhere, nor were there any other wounds. On clinical exam, although the object was palpable at the other end, there was no exit wound. There were no distal neurovascular deficits either (Fig. 2).
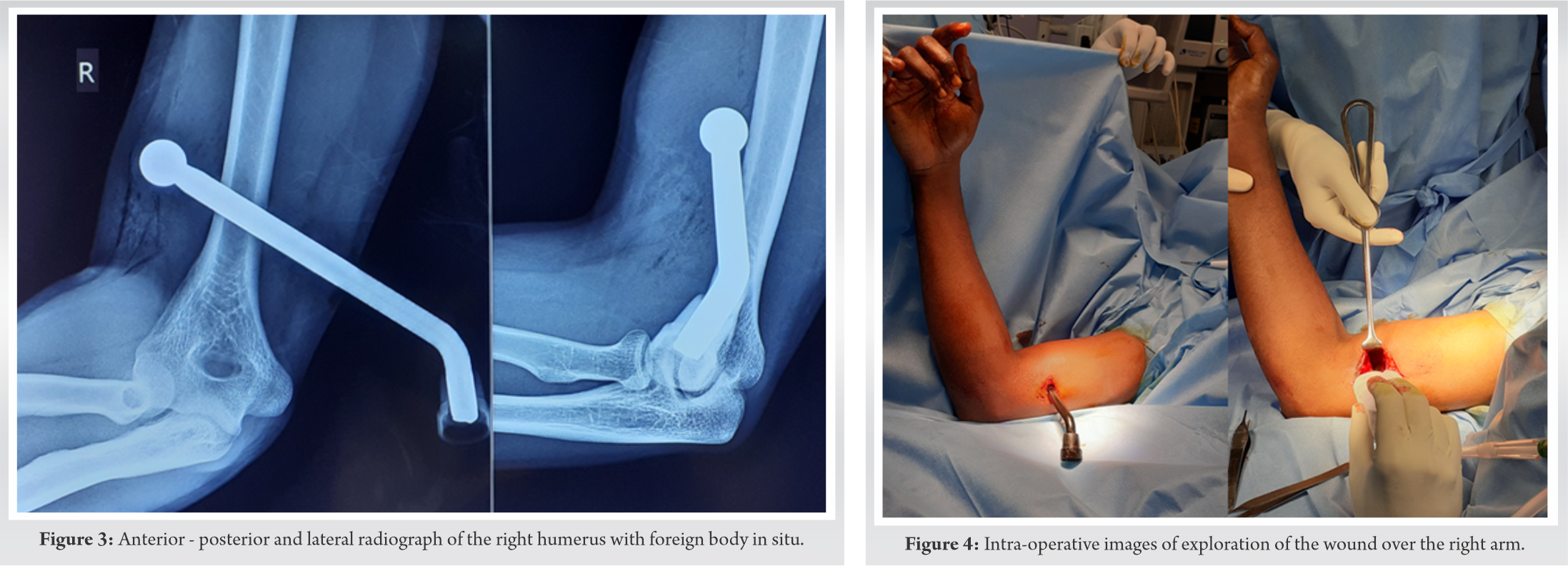
 Wrist and finger movements were normal. A radiograph was taken to look for possible foreign bodies (Fig. 3), and it showed a large metallic foreign object plunged into the anterior musculature of the lower third arm with blunt-end in situ. The patient was shifted to the operating room after getting the routine labs done. In the theater, the wound was explored under regional anesthesia (Fig. 4).
Wrist and finger movements were normal. A radiograph was taken to look for possible foreign bodies (Fig. 3), and it showed a large metallic foreign object plunged into the anterior musculature of the lower third arm with blunt-end in situ. The patient was shifted to the operating room after getting the routine labs done. In the theater, the wound was explored under regional anesthesia (Fig. 4).
 No contaminants were found. The foreign object was removed in a single-pull technique after careful dissection and debridement with copious irrigation. Twist and turn movements were avoided to prevent any iatrogenic damage to the surrounding structures (Fig. 5). Fluoroscopy was used intraoperatively to double check. Only localized muscle injury was noted. All surrounding neurovascular structures were found to be intact. The wound was closed primarily and institutional antibiotics were started. Approximately, 9-cm length of the foreign object was measured to be within the arm musculature with blunt end in situ (Fig. 6).
No contaminants were found. The foreign object was removed in a single-pull technique after careful dissection and debridement with copious irrigation. Twist and turn movements were avoided to prevent any iatrogenic damage to the surrounding structures (Fig. 5). Fluoroscopy was used intraoperatively to double check. Only localized muscle injury was noted. All surrounding neurovascular structures were found to be intact. The wound was closed primarily and institutional antibiotics were started. Approximately, 9-cm length of the foreign object was measured to be within the arm musculature with blunt end in situ (Fig. 6).
 Postoperatively, neurology was assessed and was normal (Fig. 7). A check radiograph was taken for documenting the absence of any foreign objects (Fig. 8).
Postoperatively, neurology was assessed and was normal (Fig. 7). A check radiograph was taken for documenting the absence of any foreign objects (Fig. 8).
 Further post-operative stay was uneventful. Sutures were removed by 2 weeks and at 3rd week of follow-up; the wound had healed with no residual symptom.
Further post-operative stay was uneventful. Sutures were removed by 2 weeks and at 3rd week of follow-up; the wound had healed with no residual symptom.
Riders of motorized two-wheelers form a large part of the victims of road traffic injuries [4]. Right sided injuries to the body predominate, with involvement of the upper extremity after the initial impact [5]. Head injury usually follows a secondary impact with the surroundings. The severity of injury depends on the body part involved, characteristics of the penetrating object, and the amount of energy transmitted to the tissue [1]. As often the damage is internal and not visible therefore, its assessment becomes difficult. Majority of the times the penetrating object causes a tamponade effect and its removal may cause reflux bleeding [6]. Foreign bodies could be metallic, organic, or inorganic [7]. Radiographs are a crucial first line assessment tool for metallic objects. Proper knowledge of regional anatomy is imperative before exploration. Neurovascular structures are the main concern as they can be damaged either at the point of injury or are at risk of iatrogenic damage during exploration [7]. Any potential surrounding structure being damaged may need primary repair, which may require a surgical specialist to be available and this should also be anticipated while planning [7]. Adequate anesthesia, asepsis, assistance, lighting, and time are essential prerequisites for a surgical exploration [2]. The use of tourniquet is at surgeon’s discretion, depending on the injury. The preferred path for retrieval of a foreign body is along its path of insertion [7]. The entrance of the wound containing the foreign body must be enlarged with a skin incision and a thorough debridement with lavage done under antibiotic cover, to avoid infection in the late post-operative period. Many complications have been described in literature from retained/missed foreign bodies, including migration into the joints, delayed inflammatory reactions, granuloma formation, and infection [2, 8]. Neglected foreign bodies are a common cause of malpractice claims [3]. Therefore, a good patient communication and proper documentation of pre-operative, intra-operative and post-operative findings along with corroborative clinical images and investigations are crucial for medico-legal purposes. Although in our case report we did not encounter any intra-operative or post-operative complications, it is uncommon to have just a localized injury after a penetrating trauma. We were fortunate to have such a “near miss encounter,” sparing the neurovascular structures.
A detailed history, meticulous clinical assessment and planning are paramount in the safe retrieval of a foreign body. No attempt should be made to remove a foreign body in the emergency itself. Exploration must be done in the operation theater only, as it is uncommon to have just a localized injury. Complicated retrievals may require support from other surgical specialties.
Penetrating trauma is notorious for neurovascular injuries and therefore a meticulous history taking, clinical exam, and planning is vital. Exploration in the operating room not only facilitates safe retrieval but also can avoid complications from missed foreign body. Good patient communication and proper documentation are equally important for medico-legal purposes.
References
- 1.Stewart MG, editor. Principles of ballistics and penetrating trauma. In: Head, Face and Neck Trauma: Comprehensive Management. New York: Thieme; 2005. p. 188-94. [Google Scholar]
- 2.Lammers RL. Soft tissue foreign bodies. Ann Emerg Med 1988;17:1336-44. [Google Scholar]
- 3.Vukmir RB. Medical malpractice: Managing the risk. Med Law 2004;23:495-513. [Google Scholar]
- 4.Abhilash KP, Chakraborthy N, Pandian GR, Dhanawade VS, Bhanu TK, Priya K. Profile of trauma patients in the emergency department of a tertiary care hospital in South India. J Family Med Prim Care 2016;5:558-63. [Google Scholar]
- 5.Jain A, Menezes RG, Kanchan T, Gagan S, Jain R. Two-wheeler accidents on Indian roads-a study from Mangalore, India. J Forensic Leg Med 2009;16:130-3. [Google Scholar]
- 6.Bravman JT, Ipaktchi K, Biffl WL, Stahel PF. Vascular injuries after minor blunt upper extremity trauma: Pitfalls in the recognition and diagnosis of potential “near miss” injuries. Scand J Trauma Resusc Emerg Med 2008;16:16. [Google Scholar]
- 7.Skinner EJ, Morrison CA. Wound Foreign Body Removal. In: Stat Pearls. Treasure Island, FL: Stat Pearls Publishing; 2020. [Google Scholar]
- 8.Singh A, Kaur A, Singh M. Missed foreign body in the arm-a case report. Glob J Res Anal 2017;6:337-8. [Google Scholar]







