Published online Apr 26, 2020. doi: 10.12998/wjcc.v8.i8.1525
Peer-review started: December 29, 2019
First decision: January 19, 2020
Revised: March 27, 2020
Accepted: April 10, 2020
Article in press: April 10, 2020
Published online: April 26, 2020
Gastric bronchogenic cysts (BCs) are extremely rare cystic masses caused by abnormal development of the respiratory system during the embryonic period. Gastric bronchial cysts are rare lesions first reported in 1956; as of 2019, only 37 cases are available in the MEDLINE/PubMed online databases. BCs usually have no clinical symptoms in the early stage, and their imaging findings also lack specificity. Therefore, they are difficult to diagnose before histopathological examination.
A 55-year-old woman presented at our hospital with intermittent epigastric pain. She had a slightly high level of serum carbohydrate antigen 72-4 (CA 72-4). Endoscopic ultrasound found that a cystic mass originated from the submucosa of the posterior gastric wall near the cardia, indicating a diagnosis of cystic hygroma of the stomach. Furthermore, a computed tomography scan demonstrated a quasi-circular cystic mass closely related to the lesser curvature of the gastric fundus with a low density. Because the imaging examinations did not suggest a malignancy and the patient required complete resection, she underwent laparoscopic surgery. As an intraoperative finding, this cystic lesion was located in the posterior wall of the fundus and contained some yellow viscous liquid. Finally, the pathologists verified that the cyst in the fundus was a gastric BC. The patient recovered well with normal CA 72-4 levels, and her course was uneventful at 10 mo.
This is a valuable report as it describes an extremely rare case of gastric BC. Moreover, this is the first case of BC to present with elevated CA 72-4 levels.
Core tip: Gastric bronchogenic cysts (BCs) are extremely rare and present as non-characteristic cysts on preoperative examinations. We report a rare case of gastric BC with elevated carbohydrate antigen 72-4 which is symptomatic and even not be considered for a correct diagnosis before surgery. The diagnosis of gastric BC was confirmed by the final pathological results after laparoscopic resection. We emphasize that BCs should be included in the differential diagnosis of cysts occurring in the stomach detected by imaging. And we recommend trying to acquire indication whether the mass invades the stomach wall through enhanced computed tomography to give doctors confidence in diagnosis. Endoscopic ultrasound-guided fine needle aspiration may provide the definite diagnosis of gastric BCs and even allows for conservative treatment, but much research will be still needed to confirm that.
- Citation: He WT, Deng JY, Liang H, Xiao JY, Cao FL. Bronchogenic cyst of the stomach: A case report. World J Clin Cases 2020; 8(8): 1525-1531
- URL: https://www.wjgnet.com/2307-8960/full/v8/i8/1525.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i8.1525
Gastric bronchogenic cysts (BCs) are an extremely rare congenital disease. They present as a cystic mass formed due to the abnormal development of the respiratory system during the embryonic period[1]. According to the location of the lesion, they can be divided into a mediastinal type, an intrapulmonary type, and an ectopic type[2]. Compared with rare extrathoracic and subdiaphragmatic BCs, gastric BCs are even more hard to be seen[3]. It has been put forwarded that BCs may have very rare chances to lose contact with the tracheobronchial tree and migrate to other parts[4]. Gastric bronchial cysts was first reported in 1956, and as of 2019, only a few cases have been described in reports available in the MEDLINE/PubMed online databases. The age at diagnosis of BCs covers a large range, from 25 to 81 years, its incidence is approximately twice as high in females as in males, and it generally occurs in the posterior wall of the gastric body and the lesser curve of the stomach[5]. Usually, there are no obvious clinical symptoms in the early stage of the disease, but upper abdominal pain, nausea, and vomiting are the most common symptoms at present. These may be related to the enlargement of the cyst causing swelling and exerting pressure on surrounding tissues and organs or secondary infection and perforation[6]. Its imaging findings also lack specificity. In view of the above situation, diagnosing this condition before surgery is difficult, and the rate of misdiagnosis is high; however, fortunately, its prognosis is good[7]. To lay a foundation for future clinical work, we report a 55-year-old patient with gastric BC and performed a review of the literature.
Intermittent epigastric pain.
A 55-year-old Chinese female patient visited our hospital presenting with intermittent epigastric pain for 3 mo with no nausea, vomiting, sour regurgitation, belch, dysphagia, melena, or weight loss. In addition, she recovered spontaneously.
She had a history of contrast medium-related hypersensitivity reactions.
She had a caesarean section 27 years ago.
Her abdomen was smooth and soft and free of tenderness or an overt mass. The bowel sounds were normal.
On admission, among the tumor markers, only carbohydrate antigen 72-4 (CA 72-4) level was slightly high at 8.30 U/mL (normal range, 0-6.9 U/mL). Other results, including blood biochemistry, complete blood count and so on, were within normal limits.
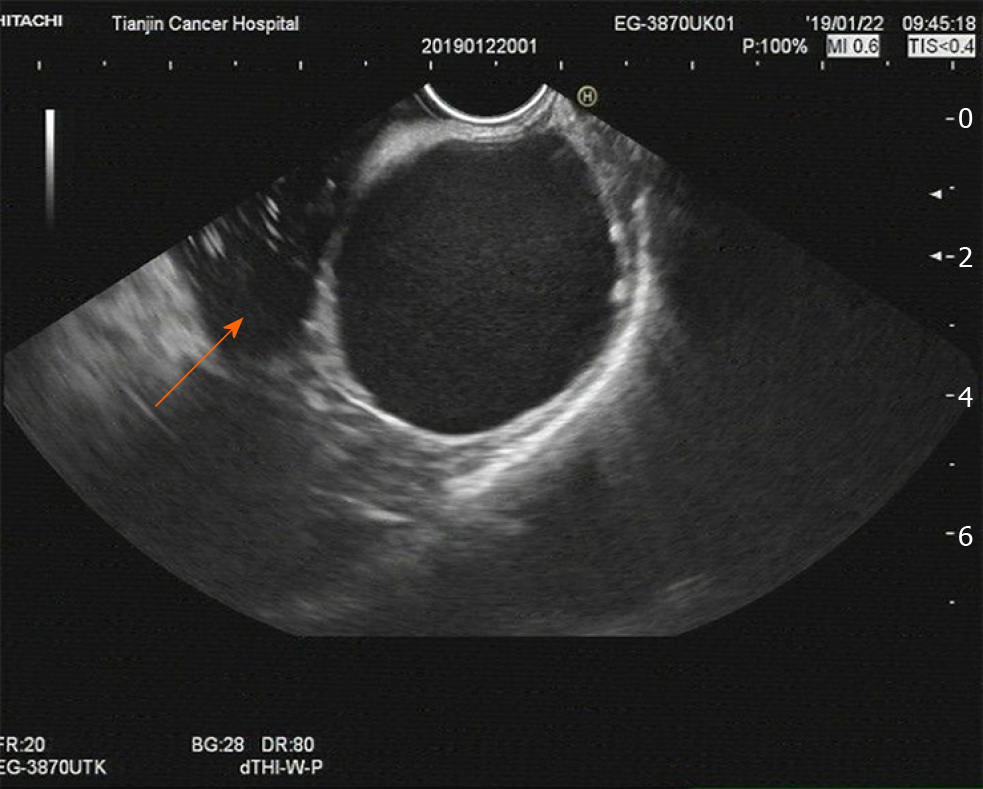
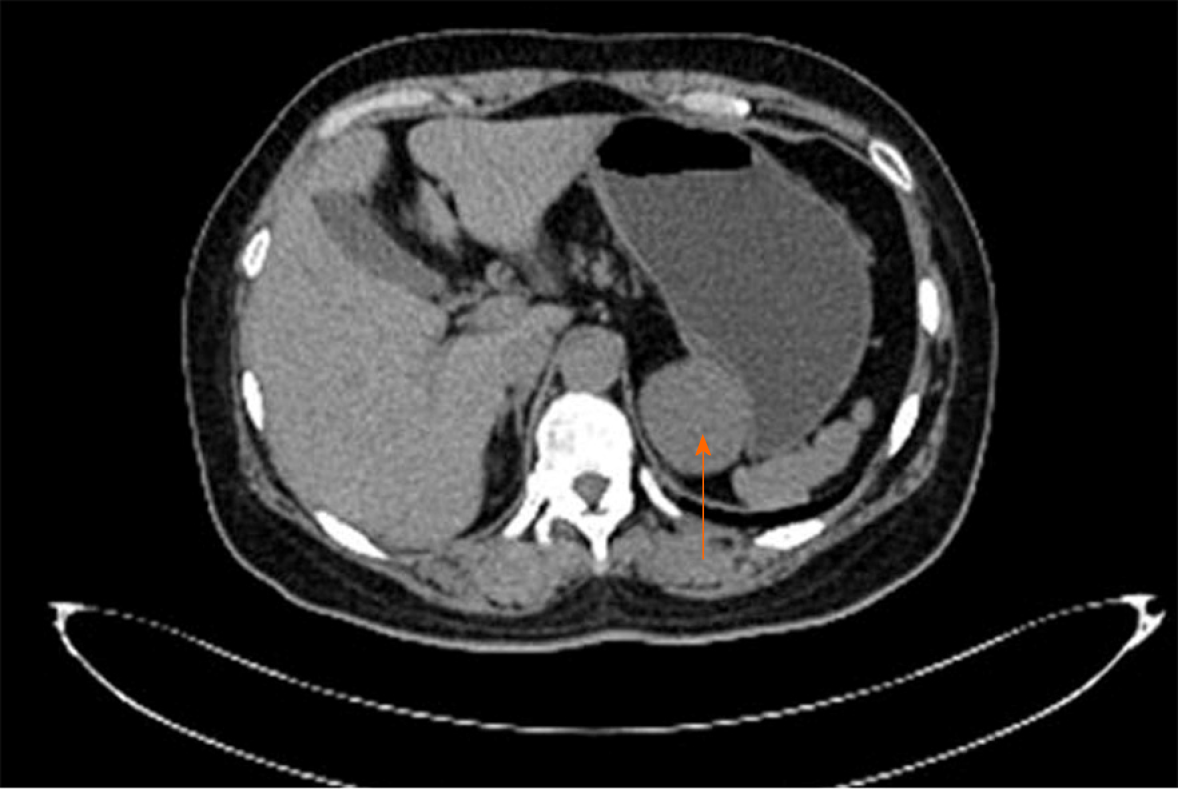
An endoscopic ultrasound (EUS) examination showed a 45 mm × 49 mm single cyst originating from the gastric submucosa. It also revealed that the cyst, without any echoes or colour flow signals, was located in the posterior wall of the fundus close to the cardia. These results indicated the possibility of cystic hygroma of the stomach (Figure 1). Furthermore, a plain computed tomography (CT) scan demonstrated a 52 mm × 43 mm quasi-circular mass. It appeared to have a low density of 29 HU and was closely related to the stomach wall of the lesser curvature of the gastric fundus, which also showed an extraluminal growth pattern with an obvious border (Figure 2). In addition, no obvious enlarged lymph nodes were found around the stomach or retroperitoneal area. Based on the above findings, a possibility for benign cyst of the gastric submucosa was considered preoperatively.
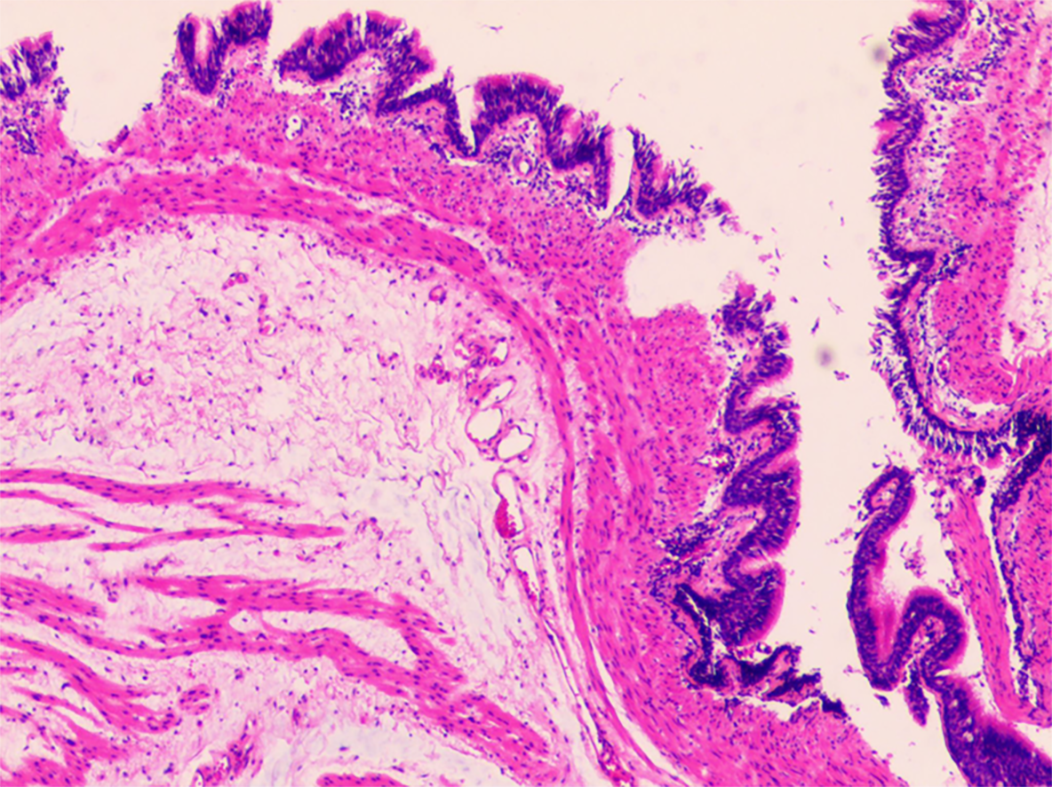
Based on the obtained specimen, this mass was accompanied by a complete capsule with a rough inner wall and measured approximately 70 mm × 60 mm × 20 mm in size. It was found to contain viscous yellow liquid. Microscopically, pseudostratified ciliated columnar epithelial cells could be observed in the cyst lining, and the structure of these cells was the same as that of the bronchus (Figure 3). Combined with immunohistochemical staining for CK7 (+), CK20 (-), TTF1 (-), and S-100 (-), the pathologists ultimately verified that this cystic mass of the fundus was a gastric BC.
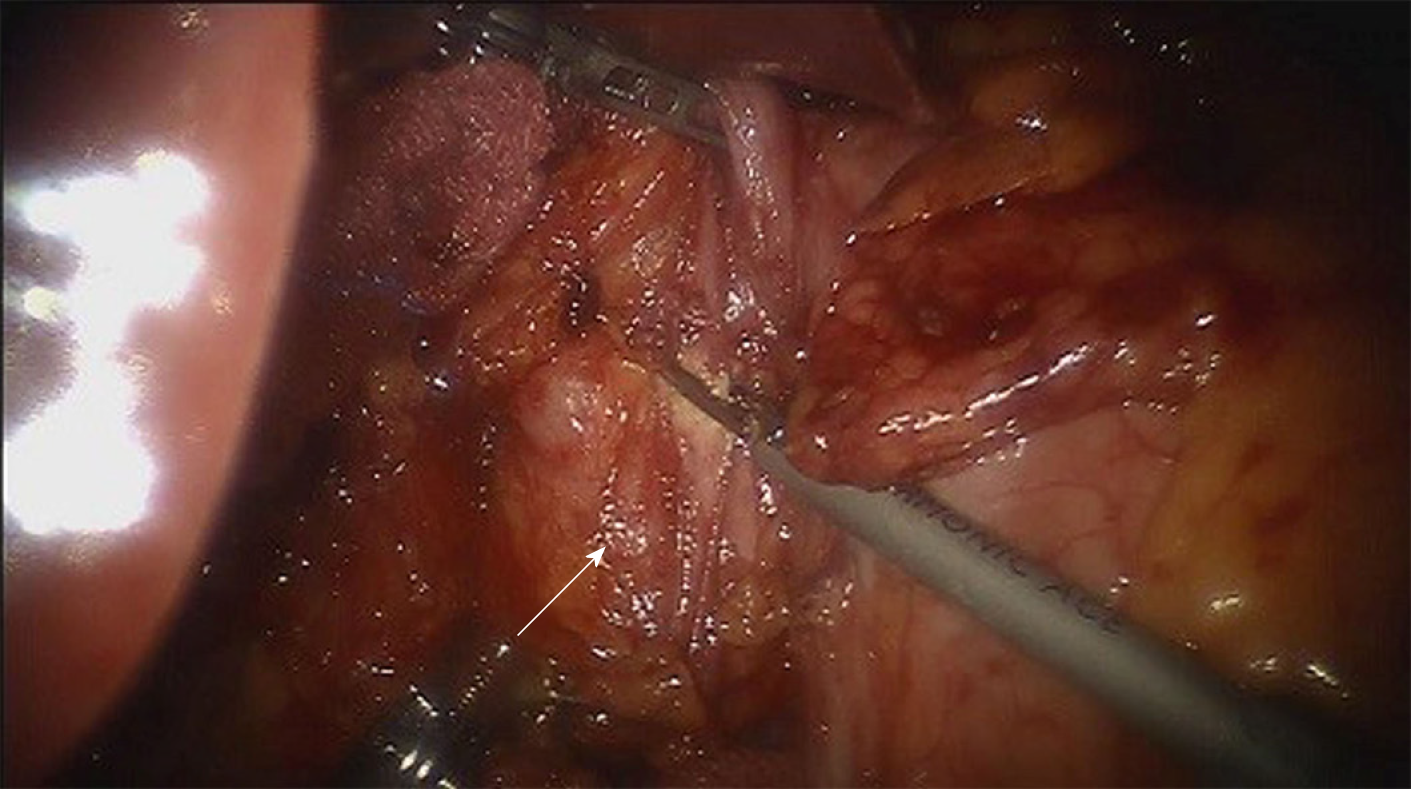
As the above imaging examinations did not clearly indicate the benign or malignant nature of the cyst and the patient wished to have the lesion completely removed, we performed a da Vinci robotic-assisted laparoscopic partial gastrectomy. Intraoperative findings of this cystic mass showed it was a smooth single-port cyst originating from the submucosa of the posterior gastric wall close to the cardia. Through surgical exploration, the gastric cavity was confirmed to be intact and smooth, and no discrete nodules were noted. Then, the cystic mass was curatively resected from the stomach, and the surgeons paid attention to avoiding cyst rupture simultaneously (Figure 4).
The patient recovered well, and her symptoms disappeared completely with a repeat CA 72-4 level normalized to 24 U/mL (0-37 U/mL) after surgery. There was no recurrence in the following 10 mo.
On imaging, a rounded cystic lesion with a well-defined boundary and no intracystic septa was noted. EUS is usually used to determine which layer of the gastric wall the lesion originates from and its general location. EUS can also reveal liquid within the cyst depending on the smooth wall and almost no echo in the lumen[8]. CT shows the location of the cyst and its relationship with surrounding tissues. On a plain CT scan, a hypodense lesion was observed, while on contrast-enhanced scan, there was no enhancement[8]. Approximately half of the cysts showed a water density value of less than 20 HU on CT[8,9]. It should be noted that if the fluid component within the cyst is thick due to a high protein content, haemorrhage, infection or calcification, a deep lesion, or poorly displayed flow signal, ultrasonography will show hypoechoic signals, and the CT value will increase[4,9-11]. These cause the cysts to be easily mistaken for solid tumors[2,12,13].
Above CT and EUS features are still not characteristic to distinguish gastric BCs from other lesions found in the submucosa of the stomach.
The final diagnosis usually depends on a pathological examination of postoperative specimens. Pathological examination will show that the capsule contains viscous or jelly-like fluid and that the wall of the capsule is lined with pseudostratified ciliated columnar epithelium accompanied by glands, smooth muscle, and cartilage tissue in partial lesions[2,14]. Some scholars believe that the discovery of ciliated respiratory epithelium and mucin on the stomach wall by EUS-guided fine needle aspiration (EUS-FNA) is sufficient for a presumptive diagnosis of cyst type, although cyst wall cartilage is considered to be the most classic basis for diagnosing BCs, a feature that cannot be unrecognized by EUS-FNA[15]. However, there is only one case with no recurrence after being diagnosed and treated as gastric BC by EUS-FNA currently[15].
Despite the questionable indications for surgical intervention, the most common choice is to remove the cyst completely via a surgical operation. We suggest that asymptomatic gastric BCs should be followed, while open surgery or laparoscopic surgery should be selected for large and symptomatic lesions, especially those with symptoms of infection and even malignant lesions[16,17]. For smaller lesions, conservative or minimally invasive treatments are also being explored. It has been reported that EUS-FNA and endoscopic mucosal resection successfully cure gastric BCs[15,18].
This is an interesting case with symptoms, elevated CA 72-4, and even unclear preoperative diagnosis. The patient’s epigastric pain was caused by the enlargement of the cyst and compression of the stomach.
One of the most unusual characteristics in this case was the correlative elevated CA 72-4 level, as in all other reported cases CA 19-9 was selected when tumor markers were raised, including those with oesophageal origins[9], gastric origins[18], and mediastinal origins[19,20]. Therefore, this is the first case of gastric BCs to manifest as described above. Consistent with this, these elevated tumor markers returned to normal after surgery[7,9,19-21], prompting us to suggest that there seems to be a direct relationship between the benign BCs and elevated tumor marker levels. However, no specific indicators have been found, and the importance of different elevated tumor markers for gastric BCs needs to be further studied.
The most regrettable thing in this case is that the preoperative diagnosis is not clear. First, it is easy to be ignored on account of the rarity of BCs. The possibility of gastric BCs should be considered when imaging suggests fluid-containing cysts in the gastric submucosa. Second, its non-specific imaging results cannot give a clear hint. Third, because the patient was allergic to the contrast agent, he failed to perform an enhanced CT which will further suggest whether the cystic lesions invaded the gastric wall. At last, after EUS revealed liquid within the cyst, no attempt was made to obtain further cytological diagnosis by EUS-FNA which maybe allow for the possibility of a confirmed diagnosis. We emphasize that BCs should be reserved in the differential diagnosis of cysts occurring in the stomach detected by imaging. And we recommend trying to acquire indication whether the mass invades the stomach wall through enhanced CT to give doctors confidence in diagnosis. EUS-FNA may provide the definite diagnosis of gastric BC and even allows for conservative treatment, but much research is still needed to confirm it.
This report is significant because it describes a very rare case of gastric BC. In addition, this is the first report to describe an increase in CA 72-4 levels in BC. This finding could be conducive to achieving better preoperative diagnoses and better choice of treatment and improving our understanding of the disease.
Manuscript source: Invited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Andrejic-Visnjic B, Fatemi R, Lambrecht NW S-Editor: Dou Y L-Editor: Wang TQ E-Editor: Li X
| 1. | Ubukata H, Satani T, Motohashi G, Konishi S, Goto Y, Watanabe Y, Nakada I, Tabuchi T. Intra-abdominal bronchogenic cyst with gastric attachment: report of a case. Surg Today. 2011;41:1095-1100. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | McAdams HP, Kirejczyk WM, Rosado-de-Christenson ML, Matsumoto S. Bronchogenic cyst: imaging features with clinical and histopathologic correlation. Radiology. 2000;217:441-446. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 262] [Cited by in F6Publishing: 214] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
| 3. | Takeda S, Miyoshi S, Minami M, Ohta M, Masaoka A, Matsuda H. Clinical spectrum of mediastinal cysts. Chest. 2003;124:125-132. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 183] [Cited by in F6Publishing: 193] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 4. | Sumiyoshi K, Shimizu S, Enjoji M, Iwashita A, Kawakami K. Bronchogenic cyst in the abdomen. Virchows Arch A Pathol Anat Histopathol. 1985;408:93-98. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 73] [Cited by in F6Publishing: 76] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 5. | Yang X, Guo K. Bronchogenic cyst of stomach: two cases report and review of the English literature. Wien Klin Wochenschr. 2013;125:283-287. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Monin MI, Pudovikov SS, Topalov KP. [Surgical treatment of mediastinal tumors and cysts]. Vestn Khir Im I I Grek. 1987;138:12-15. [PubMed] [Cited in This Article: ] |
| 7. | Tan KK, Nandini CL, Ho CK. A case of gastric bronchogenic cyst in Singapore with multiple intrigues. ANZ J Surg. 2010;80:286-287. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Murakami R, Machida M, Kobayashi Y, Ogura J, Ichikawa T, Kumazaki T. Retroperitoneal bronchogenic cyst: CT and MR imaging. Abdom Imaging. 2000;25:444-447. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 35] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Cheng Y, Chen D, Shi L, Yang W, Sang Y, Duan S, Chen Y. Surgical treatment of an esophageal bronchogenic cyst with massive upper digestive tract hematoma without esophagectomy: a case report and the review of the literature. Ther Clin Risk Manag. 2018;14:699-707. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Sirivella S, Ford WB, Zikria EA, Miller WH, Samadani SR, Sullivan ME. Foregut cysts of the mediastinum. Results in 20 consecutive surgically treated cases. J Thorac Cardiovasc Surg. 1985;90:776-782. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 79] [Cited by in F6Publishing: 47] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 11. | Wiech T, Walch A, Werner M. Histopathological classification of nonneoplastic and neoplastic gastrointestinal submucosal lesions. Endoscopy. 2005;37:630-634. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 79] [Cited by in F6Publishing: 88] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 12. | Melo N, Pitman MB, Rattner DW. Bronchogenic cyst of the gastric fundus presenting as a gastrointestinal stromal tumor. J Laparoendosc Adv Surg Tech A. 2005;15:163-165. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Fazel A, Moezardalan K, Varadarajulu S, Draganov P, Eloubeidi MA. The utility and the safety of EUS-guided FNA in the evaluation of duplication cysts. Gastrointest Endosc. 2005;62:575-580. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 54] [Cited by in F6Publishing: 57] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 14. | Cuypers P, De Leyn P, Cappelle L, Verougstraete L, Demedts M, Deneffe G. Bronchogenic cysts: a review of 20 cases. Eur J Cardiothorac Surg. 1996;10:393-396. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 50] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 15. | Sato M, Irisawa A, Bhutani MS, Schnadig V, Takagi T, Shibukawa G, Wakatsuki T, Imamura H, Takahashi Y, Sato A, Hikichi T, Obara K, Hashimoto Y, Watanabe K, Ohira H. Gastric bronchogenic cyst diagnosed by endosonographically guided fine needle aspiration biopsy. J Clin Ultrasound. 2008;36:237-239. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 24] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 16. | Shibahara H, Arai T, Yokoi S, Hayakawa S. Bronchogenic cyst of the stomach involved with gastric adenocarcinoma. Clin J Gastroenterol. 2009;2:80-84. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 17. | Sun L, Lu L, Fu W, Li W, Liu T. Gastric bronchogenic cyst presenting as a gastrointestinal stromal tumor. Int J Clin Exp Pathol. 2015;8:13606-13612. [PubMed] [Cited in This Article: ] |
| 18. | Lee SH, Park DH, Park JH, Kim HS, Park SH, Kim SJ, Oh MH. Endoscopic mucosal resection of a gastric bronchogenic cyst that was mimicking a solid tumor. Endoscopy. 2006;38 Suppl 2:E12-E13. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | Okubo A, Sone S, Ogushi F, Ogura T, Uyama T, Monden Y, Ii K. A case of bronchogenic cyst with high production of antigen CA 19-9. Cancer. 1989;63:1994-1997. [PubMed] [Cited in This Article: ] |
| 20. | Okabayashi K, Motohiro A, Ueda H, Ondo K, Kawahara K, Shirakusa T. Subcarinal bronchogenic cyst with high carbohydrate antigen 19-9 production. Jpn J Thorac Cardiovasc Surg. 2002;50:46-48. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 21. | Chen J, Liu Q, Ling Y, Yang H, Wen J, Luo K, Hu Y, Tan Z, Fu J. Extraordinarily elevated serum CA19-9 in a patient with posterior mediastinum cyst: a case report. Clin Chem Lab Med. 2017;55:e279-e281. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |