Published online Jul 26, 2022. doi: 10.12998/wjcc.v10.i21.7348
Peer-review started: January 15, 2022
First decision: April 8, 2022
Revised: April 15, 2022
Accepted: May 27, 2022
Article in press: May 27, 2022
Published online: July 26, 2022
Sagittal alignment of the spine, pelvis, and lower extremities is essential for maintaining a stable and efficient posture and ambulation. Imbalance in any element can result in compensatory changes in the other elements. Knee flexion is a compensatory mechanism for spinopelvic sagittal alignment and is markedly affected in severe knee osteoarthritis (OA). The correction of knee flexion deformity (KFD) by total knee arthroplasty (TKA) can lead to complementary changes in the sagittal spinopelvic parameters (SSPs).
To determine the SSP changes in patients with knee OA, with or without KFD undergoing TKA.
The study was conducted in 32 patients who underwent TKA. A neutral standing whole-spine lateral radiograph was performed before surgery and 3 mo after surgery in these patients. Subjects were divided into two groups (Group 1 obtained > 10° corrections in KFD; group B obtained < 10° correction). The pelvic tilt (PT), pelvic incidence (PI), sacral slope (SS), lumbar lordosis (LL), and sagittal vertical axis (SVA) were measured.
The median of change in PT, PI, SS, LL, and SVA was 0.20 mm, 1.00 mm, 2.20 mm, −0.40 mm, and 6.8 mm, respectively. The difference in the change in SSPs between the two groups was statistically non-significant.
SSPs, such as PI, PT, SS, LL, and SVA, do not change significantly following TKA in end-stage knee OA despite a significant correction (> 10°) in KFD.
Core Tip: The sagittal alignment of the spine, pelvis, and lower extremities is essential for maintaining a stable and efficient posture and ambulation. Any imbalance in one element can result in compensatory changes in the other. Low back pain arising from hip pathology was termed “hip spine syndrome.” As the sagittal spinopelvic parameters (SSPs) were described, the researchers became inquisitive about documenting these changes in hip pathology and post-surgical correction. After two decades, the “knee spine syndrome” was described in a similar logical sequence. The SSPs have become an area of interest with several user-friendly tools to measure. The current papers evaluate these parameters in patients with osteoarthritis knee and undergoing total knee replacement.
- Citation: Puthiyapura LK, Jain M, Tripathy SK, Puliappadamb HM. Effect of osteoarthritic knee flexion deformity correction by total knee arthroplasty on sagittal spinopelvic alignment in Indian population. World J Clin Cases 2022; 10(21): 7348-7355
- URL: https://www.wjgnet.com/2307-8960/full/v10/i21/7348.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i21.7348
Osteoarthritis (OA) is a disease characterized by degeneration of cartilage and underlying bone within a joint. Patients with knee OA exhibit fixed flexion deformity and varus or valgus coronal deformity in the late stages. Total knee arthroplasty (TKA) is a safe and effective procedure for these patients. It reduces pain, corrects deformities, restores function, and improves the patient’s quality of life[1].
Spinopelvic sagittal alignment (SSA) of the body is vital for maintaining a stable and efficient posture and ambulation[2,3]. Any imbalance in the SSA can lead to compensatory changes in the pelvis, hip, and knee to ensure a static horizontal gaze with minimum energy expenditure[4]. Offierski and MacNab[2] first described the "hip spine syndrome," wherein hip diseases were associated with lower back pain (LBP)[2]. Additionally, Schwab et al[4] observed that altered SSA was mainly responsible for the LBP[4]. Parvizi et al[3] noticed a change in the sagittal spinopelvic parameters (SSPs) in patients with hip OA undergoing total hip arthroplasty (THA)[3]. Recently, Murata et al[5] described the "knee spine syndrome” for lumbar spine symptoms caused by degenerative changes in the knee[5]. Lee et al[6] observed that a change in SSPs compensates knee flexion[6]. Hence, correcting knee flexion deformity (KFD) by TKA could lead to complementary changes in the SSPs. While most patients have improved spinal problems following TKA, few have worsening of spinal problems or recurrence of KFD. Therefore, these multiple joints interact and affect each other. However, studies in this regard are scarce[7,8].
Indian people are predisposed to early knee OA due to their habit of squatting and sitting cross-legged[9]. The present study attempted to evaluate and validate changes in SSPs following the correction of KFD by TKA in the Indian population.
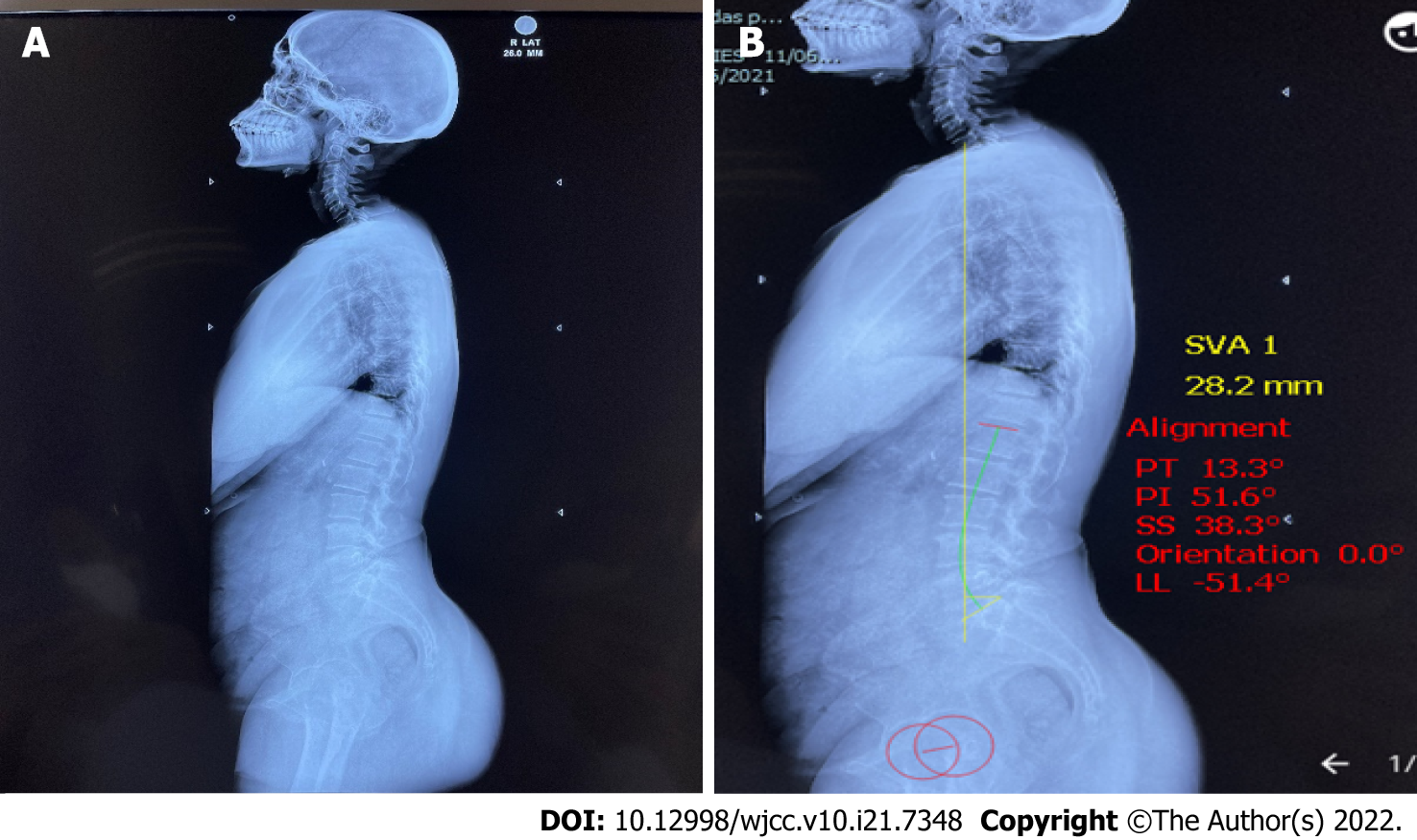
The present prospective observational study was conducted using 32 patients with knee OA admitted for TKA to the Department of Orthopedics at our institute from March 2020 to August 2021 after institutional ethics clearance. Patients with previous spine, hip, or knee surgery; previous spinal fractures, infections, coronal deformity > 10°; spondylolisthesis; or sagittal foot deformities were excluded from the study. Based on a previous study by Lee et al[7], with a mean difference of 4 and standard deviation (SD) of 8, assuming alpha = 0.05 and power (1-beta) = 80%, using the formula n = 2 [Z (1-α/2) + Z (1-β)]2 × SD2/d2, (d: Effect size), the sample size was calculated to be 32. Informed consent was obtained from all patients. Clinical and radiological examinations of the spine and knee were performed in all patients. A standing neutral whole spine static lateral radiograph (scannogram) was performed preoperatively and after 3 mo of TKA. Radiological SSP was measured on a 36” cassette orthoscannogram of the whole spine until mid-thigh. The lateral view was obtained using the software Surgimap (Surgimap, New York, NY, United States)[10]. Several studies have validated the accuracy of Surgimap[11,12]. The following SSPs were measured: (1) Pelvic incidence (PI): Angle between the line joining the center of the bicoxofemoral axis with the mid-point of the S1 endplate and another perpendicular to the S1 at its mid-point (normal = 45 ± 15); (2) Pelvic tilt (PT): Angle between the vertical reference line and line joining the hip axis to the center of the superior S1 endplate (normal = 12.6 ± 4.6); (3) Sacral slope (SS): Angle between the superior end of S1 and horizontal (normal = 37.7 ± 9.7); (4) Lumbar lordosis (LL): Angle between the superior endplate of L1 and S1 (normal = 54.6 ± 10); and (5) Sagittal vertical axis (SVA): Distance of a line connecting the centroid of the C7 vertebra and posterior superior sacral endplate from the sacral reference (normal < 5 cm) (Figure 1). Patients were divided into two groups, namely group A comprising patients with KFD correction > 10°, and group B comprising patients with KFD correction < 10°.
The knee flexion angle (KFA) is the angle between the long axis of the femur and tibia, with lateral femur epicondyle as the center, and is measured using a goniometer. The average of the two flexion deformity angles was considered for analysis in bilateral cases.
Patients were divided into two groups, Group A with correction of KFD > 10° and Group B with correction of KFD < 10°.
Descriptive statistics were used to analyze the demographic profile. Changes in parameters following TKA were analyzed using the Wilcoxon signed-rank test for non-parametric data. The Mann-Whitney U test was used to determine the difference between the two groups. Correlation between KFD angle and SSPs was determined using the Spearman's rank test.
The demographic details and baseline clinical and radiological parameters were assessed. No patient was lost to follow-up. Of the 32 patients, 9 were men, and 23 were women. Bilateral TKA was performed in 22 patients, whereas unliteral TKA was performed in 10 patients. The mean age of the patients was 61.5 ± 7.64 years. The preoperative and postoperative SSPs are presented in Table 1. The preoperative KFD was 10.0 (IQR: 5–18.75, range: 0-30) and post-operative KFD was 0.0 (IQR: 0-5, range: 0-15) with a correction of 5.0 (IQR: 1.25-15, range: 0-20), P < 0.001. Hence, based on a change in KFD, 15 patients qualified in group A and 17 patients in group B. There was no significant difference between the two groups in terms of SSPs (Table 2). Similarly, a sub-group analysis of unilateral and bilateral TKA also yielded no significant difference (Table 3). No significant difference was evident in SSP’s between males and females (Table 4).
| No. | Variable | Pre-op, median (IQR) | Post-op, median (IQR) | P value |
| 1 | PT | 14.4 (10.1-18.4) | 14.1 (10.6-18.6) | 0.455 |
| 2 | PI | 49.3 (44-54.9) | 50.9 (44.5-57.5) | 0.148 |
| 3 | SS | 36.4 (29.2-40.3) | 36.7 (28.5-41.1) | 0.551 |
| 4 | LL | -46.8 (-53.6 to -42) | -48.0 (-53.6 to -40.3) | 0.390 |
| 5 | SVA | 44.1 (3.0-78.5) | 46.8 (21.7-77.0) | 0.153 |
| No. | Variable | Group A, n = 15 | Group B, n = 17 | ||||
| Pre-op, median (IQR) | Post-op, median (IQR) | P value | Pre-op, median (IQR) | Post-op, median (IQR) | P value | ||
| 1 | PT | 14.9 (11.1-20.8) | 14 (7.2-20.4) | 0.35 | 14.0 (9.4-18.2) | 14.4 (12.2-17) | 0.540 |
| 2 | PI | 45.3 (43.6-54.6) | 51.6 (44-6-61.6) | 0.124 | 48.6 (44.2-56.3) | 48.3 (42-55.7) | 0.603 |
| 3 | SS | 35.2 (29.5-39.5) | 37.7 (30.6-42.3) | 0.413 | 36.9 (26.7-41.8) | 35.1 (26.5-40.6) | 0.890 |
| 4 | LL | -46.4 (-49.7 to -43.8) | -48.5 (-55.6 to -42.5) | 0.639 | -47.8 (-56 to -40.6) | -47.5 (-52.5 to -38.5) | 0.579 |
| 5 | SVA | 42.9 (-36.6-78.7) | 63.7 (28.2-78.1) | 0.107 | 50.1 (17.4-79.0) | 28.2 (18.9-78.0) | 0.747 |
| No. | Variable | Unilateral, n = 10 | Bilateral, n = 22 | ||||
| Pre-op, median (IQR) | Post-op, median (IQR) | P value | Pre-op, median (IQR) | Post-op, median (IQR) | P value | ||
| 1 | PT | 14 (10.1-23.4) | 13.8 (9.4-21.4) | 0.625 | 14.5 (9.8-18.3) | 14.1 (11.2-17.2) | 0.406 |
| 2 | PI | 51.1 (44.4-54.3) | 52 (41.6-63.0) | 0.193 | 48.5 (43.7-56.1) | 49.5 (44.5-54.9) | 0.384 |
| 3 | SS | 36.7 (28.6-38.5) | 37.2 (27.9-43.9) | 0.322 | 35.7 (28.9-41.7) | 36.4 (28.4-39.8) | 0.943 |
| 4 | LL | -44.5 (-55.4 to -38.2) | -48 (-57.8 to -36) | 0.959 | -47.5 (-54 to -43.2) | -48 (-53.6 to -40.9) | 0.867 |
| 5 | SVA | 47.7 (20.6-83.2) | 52.0 (26.1-83.6) | 0.375 | 42.5 (-2.9-79.1) | 33.4 (19.9-77.2) | 0.443 |
| No. | Variable | Males, n = 9 | Females, n = 23 | ||||
| Pre-op | Post-op | P value | Pre-op | Post-op | P value | ||
| 1 | PT | 13.7 | 13.2 | 0.571 | 15.7 | 17.1 | 0.660 |
| 2 | PI | 48.6 | 48.8 | 0.335 | 50.1 | 52.1 | 0.771 |
| 3 | SS | 34.9 | 35.5 | 0.967 | 34.4 | 34.9 | 0.934 |
| 4 | LL | -49.6 | -45.7 | 0.201 | -46.2 | -47.0 | 0.837 |
| 5 | SVA | 50.1 | 69.6 | 0.837 | 32.6 | 44.5 | 0.409 |
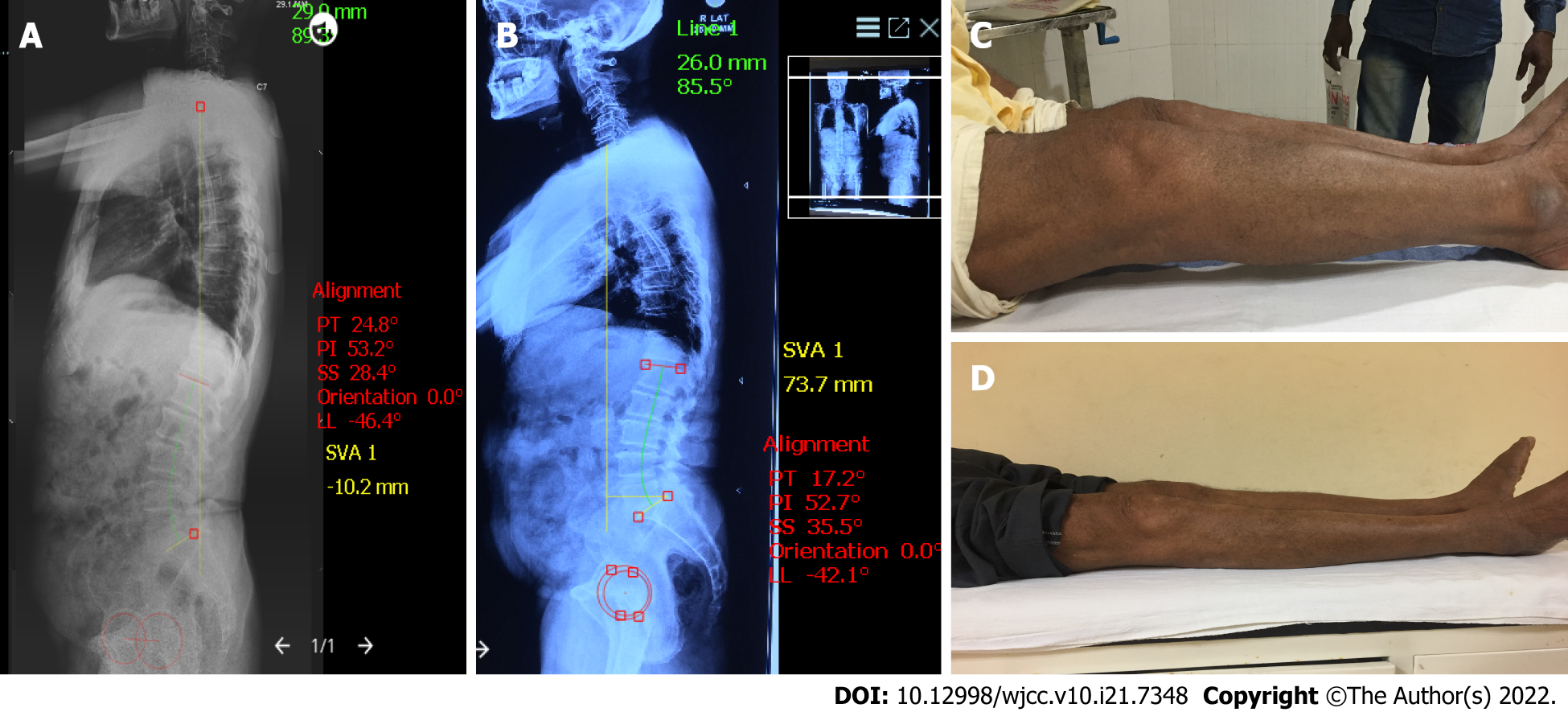
SVA > 50 mm was labeled as a global sagittal imbalance. Of the 32 patients, 16 exhibited preoperative sagittal imbalance. Of these 16 patients, the sagittal balance was restored only in 7 patients following TKA. No significant correlation was observed between change in KFD and change in SSPs (P > 0.05). A case example is illustrated in Figure 2.
In our study of groups, with correction of KFD > 10° and correction of KFD < 10°, we did not find any statistical difference in the change in SSA.
SSA is crucial for maintaining a stable and efficient upright posture and ambulation[11]. The body requires more energy consumption to maintain equilibrium when the SSA is abnormal. Pathology in the spine, pelvis, or lower extremity can disrupt the postural equilibrium. The close interrelation between these segments ensures compensatory changes in other segments. Offierski and MacNab[2] (1983) coined the term "hip spine syndrome" for LBP secondary to a hip pathology. Schwab et al[4] exhibited that alteration in the SSPs was mainly responsible for LBP in this syndrome[4]. Thus, several studies have evaluated SSPs in patients with hip pathology. However, the results have been equivocal. Parvizi et al[3] documented some changes in the SSPs, whereas Ben-Galim et al[13], Eyvazov et al[14], and Eguchi et al[15] did not observe any changes in SSPs despite improvement in the visual analogue score and Oswestry disability index score for LBP following THA[3,13-15].
Murata et al[5] described the "knee–spine syndrome" in 2003 and observed a significantly lower LL in patients with KFD more than 5°[5]. Additionally, the limitation of knee extension was more significant in patients with LL < 30°. Thus, degenerative knee joint changes could lead to LBP. Lee et al[6] used a motion-controlled knee brace bilaterally in a group of young men to simulate knee flexion contractures[6]. The SSPs were examined at 0°, 15°, and 30° of knee flexion. Femoropelvic angle and LL reduced significantly at 15° and 30° of knee flexion compared with full extension. Harato et al[16] performed a gait analysis in simulated knee flexion[16]. At 30° flexion, a backward inclination of the pelvis was observed during standing, whereas a forward inclination of the trunk and pelvis was observed during walking. Thus, flexion contracture of the knee could cause changes in SSA, thereby proving the effect of SSPs on KFD. Therefore, the present study evaluated these parameters.
The mean age of the patients in the present study was 61.5 years (range: 41–76), which is lesser than that exhibited in studies by Kim et al[17] (70.5 years) and Kitagawa et al[8] (75 years)[8,17]. This may be due to the habit of squatting, cross-legged sitting, and kneeling among Indian people, which predispose them to OA at an early age[9]. Of the 32 patients in the present study, 22 underwent bilateral TKA, whereas 10 underwent unilateral TKA. The present study was conducted in 23 women and 9 men, whereas the study by Lee et al[7] included only women[7].
The median preoperative KFD in the present study was 10° (IQR: 5–18.75, range: 0–30). Complete knee extension was achieved following TKA (IQR: 0°–5°, range: 0°–15°, P < 0.001). Lee et al[7], Kim et al[17], and Kitagawa et al[8] also reported a significant reduction in KFD after TKA[7,8,17].
Kim et al[17] (2020) defined lumbar flexibility (LF) as the difference in LL in extension and flexion, and pelvic flexibility (PF) as PI. They reported an increase in LL and improvement in SVA following TKA in patients exhibiting better LF. Patients with better PF exhibited an increase in SS[17]. Kitagawa et al[8] measured the difference between the PI and LL. A difference of > 10° was observed in a majority of their patients (> 50%). Additionally, a significant improvement was observed in SSPs following TKA with increased SS and reduced SVA and PT[8]. However, the present study did not observe a significant change in SSPs (PT, PI, SS, LL, SVA) following TKA (P > 0.05). In the present study, 16 patients exhibited global sagittal imbalance (SVA > 50 mm). Following TKA, 7 of these patients attained sagittal balance (SVA < 50 mm), whereas the sagittal imbalance was reduced but persisted in the remaining 9 patients. The present study exhibited a short follow-up period of 3 mo. Longer mobilization could result in more profound changes in the SSPs. The other possibility is that the spinal changes were irreversible, which has been observed in a few studies on SSPs following THA[13,14].
The present study divided the patients into two groups, namely group A comprising patients with KFD correction > 10° and group B comprising patients with KFD correction < 10°. Because 5° is too small to measure clinically, 10° was considered the critical angle. No significant difference was observed between these two groups regarding changes in SSPs (P > 0.05). Lee et al[7] reported a significant increase in SS in a few patients with > 10° deformity correction. However, a corresponding change in PT was not observed. The authors admitted that it was due to an error while taking the radiograph[7]. PI remained almost the same in all studies because it remains constant for a particular individual unless there is a sacroiliac dissociation.
PI positively correlated with PT, SS, and LL among the preoperative parameters. SVA exhibited a positive correlation with SS. No significant correlation was observed between flexion deformity and preoperative SSPs, whereas a significant positive correlation was observed between postoperative flexion deformity and PI and SS. No significant correlation was observed between correction in flexion deformity and SSP changes. Kitagawa et al[8] reported a significant positive correlation of the KFA with SVA and a negative correlation with SS and LL[8]. The present study conducted a subgroup analysis between patients undergoing unilateral and bilateral TKA. However, the difference was statistically non-significant (P > 0.05).
The present study considered TKA and SSPs in the Indian population. The study is novel because literature regarding this aspect among the Indian population is scarce. All patients with concomitant spinal disease or previous surgery were excluded from the present study to reduce bias. Subgroup analysis was conducted to evaluate the difference between unilateral and bilateral TKA. However, the present study has certain limitations. The lateral radiograph measurements in a neutral standing position of the whole spine were from a static capture, not representative of functional performance. Perhaps the degree of pre-operative KFD could have also played a role in the pre-operative SSA. Also, other factors may more readily determine the SSA, like physical activity exposure related to standing-walking, posture habits in general, and long-term body schema memory, establishing a certain deformity permanently (due to a long term knee-flexion contracture), which would be impossible to reverse even in a 3-mo post-surgery timeframe. Since the TKA was performed unilaterally in several patients, perhaps a frontal spino-pelvic alignment could have also been examined. A small sample size and a short follow-up period prevent the generalization of the study findings. Additionally, LBP was not substantiated using a score despite an improvement in LBP in the follow-up. Further comprehensive multicenter studies with a larger sample size, longer follow-up time, and clinical LBP scores will strengthen the findings of this study.
SSPs, such as PI, PT, SS, LL, and SVA, do not change significantly following TKA in end-stage knee OA despite a significant correction (> 10°) in KFD. Thus, routine determination of the SSPs may not be required in patients undergoing TKA.
Sagittal alignment of the spine, pelvis, and lower extremities is essential for stable and efficient posture and walking. An imbalance in any element results in compensatory changes in other elements. Knee flexion, a compensatory mechanism for sagittal alignment of the spine and pelvis, is significantly affected in severe knee osteoarthritis (OA). Correction of knee flexion deformity (KFD) by total knee arthroplasty (TKA) results in complementary changes in sagittal spine-pelvic parameters (SSPs).
To evaluate and validate changes in SSPs following the correction of KFD by TKA.
The present study determined the sagittal spinopelvic parameters changes in patients with knee osteoarthritis, with or without knee flexion deformity, undergoing total knee arthroplasty.
The study was conducted in 32 patients who underwent TKA. A neutral standing whole-spine lateral radiograph was performed before surgery and 3 mo after surgery in these patients. Subjects were divided into two groups (group 1 obtained > 10° corrections in KFD; group B obtained < 10° correction). The pelvic tilt (PT), pelvic incidence (PI), sacral slope (SS), lumbar lordosis (LL), and sagittal vertical axis (SVA) were measured.
The median of change in PT, PI, SS, LL, and SVA was 0.20 mm, 1.00 mm, 2.20 mm, −0.40 mm, and 6.8 mm, respectively. The difference in the change in SSPs between the two groups was statistically non-significant.
SSPs, such as PI, PT, SS, LL, and SVA, do not change significantly following TKA in end-stage knee OA despite a significant correction (> 10°) in KFD.
The direction of further studies should include a larger sample size, longer follow-up time, and clinical lower back pain scores to strengthen the findings of this study.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Jennane R, France; Koumantakis GA, Greece; Ni GX, China A-Editor: Yao QG, China S-Editor: Fan JR L-Editor: Filipodia P-Editor: Fan JR
| 1. | Hussain SM, Neilly DW, Baliga S, Patil S, Meek R. Knee osteoarthritis: a review of management options. Scott Med J. 2016;61:7-16. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 100] [Cited by in F6Publishing: 108] [Article Influence: 13.5] [Reference Citation Analysis (0)] |
| 2. | Offierski CM, MacNab I. Hip-spine syndrome. Spine (Phila Pa 1976). 1983;8:316-321. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 324] [Cited by in F6Publishing: 310] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 3. | Parvizi J, Pour AE, Hillibrand A, Goldberg G, Sharkey PF, Rothman RH. Back pain and total hip arthroplasty: a prospective natural history study. Clin Orthop Relat Res. 2010;468:1325-1330. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 116] [Cited by in F6Publishing: 117] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 4. | Schwab F, Lafage V, Patel A, Farcy JP. Sagittal plane considerations and the pelvis in the adult patient. Spine (Phila Pa 1976). 2009;34:1828-1833. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 518] [Cited by in F6Publishing: 511] [Article Influence: 34.1] [Reference Citation Analysis (0)] |
| 5. | Murata Y, Takahashi K, Yamagata M, Hanaoka E, Moriya H. The knee-spine syndrome. Association between lumbar lordosis and extension of the knee. J Bone Joint Surg Br. 2003;85:95-99. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 94] [Cited by in F6Publishing: 96] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 6. | Lee CS, Park SJ, Chung SS, Lee KH. The effect of simulated knee flexion on sagittal spinal alignment: novel interpretation of spinopelvic alignment. Eur Spine J. 2013;22:1059-1065. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 25] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Lee SM, Yoon MG, Moon MS, Lee BJ, Lee SR, Seo YH. Effect of correction of the contractured flexed osteoarthritic knee on the sagittal alignment by total replacement. Asian Spine J. 2013;7:204-211. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 8. | Kitagawa A, Yamamoto J, Toda M, Hashimoto Y. Spinopelvic Alignment and Low Back Pain before and after Total Knee Arthroplasty. Asian Spine J. 2021;15:9-16. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 9. | Kumar H, Pal CP, Sharma YK, Kumar S, Uppal A. Epidemiology of knee osteoarthritis using Kellgren and Lawrence scale in Indian population. J Clin Orthop Trauma. 2020;11:S125-S129. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | Surgimap. Surgimap software. [cited 10 January 2022]. Available from: https://www.surgimap.com. [Cited in This Article: ] |
| 11. | Akbar M, Terran J, Ames CP, Lafage V, Schwab F. Use of Surgimap Spine in sagittal plane analysis, osteotomy planning, and correction calculation. Neurosurg Clin N Am. 2013;24:163-172. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 89] [Cited by in F6Publishing: 92] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 12. | Miranda SF, Corotti VGP, Menegaz P, Ueda W, Vialle EN, Vialle LR. Influence of total hip arthroplasty on sagittal lumbar-pelvic balance: Evaluation of radiographic parameters. Rev Bras Ortop (Sao Paulo). 2019;54:657-664. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Ben-Galim P, Ben-Galim T, Rand N, Haim A, Hipp J, Dekel S, Floman Y. Hip-spine syndrome: the effect of total hip replacement surgery on low back pain in severe osteoarthritis of the hip. Spine (Phila Pa 1976). 2007;32:2099-2102. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 160] [Cited by in F6Publishing: 143] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 14. | Eyvazov K, Eyvazov B, Basar S, Nasto LA, Kanatli U. Effects of total hip arthroplasty on spinal sagittal alignment and static balance: a prospective study on 28 patients. Eur Spine J. 2016;25:3615-3621. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 15. | Eguchi Y, Iida S, Suzuki C, Shinada Y, Shoji T, Takahashi K, Ohtori S. Spinopelvic Alignment and Low Back Pain after Total Hip Replacement Arthroplasty in Patients with Severe Hip Osteoarthritis. Asian Spine J. 2018;12:325-334. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 16. | Harato K, Nagura T, Matsumoto H, Otani T, Toyama Y, Suda Y. A gait analysis of simulated knee flexion contracture to elucidate knee-spine syndrome. Gait Posture. 2008;28:687-692. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 63] [Cited by in F6Publishing: 55] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 17. | Kim SC, Kim JS, Choi HG, Kim TW, Lee YS. Spinal Flexibility Is an Important Factor for Improvement in Spinal and Knee Alignment after Total Knee Arthroplasty: Evaluation Using a Whole Body EOS System. J Clin Med. 2020;9. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |