23 August 2023: Clinical Research
Effect of Femoral Nerve Block with Different Concentrations of Chloroprocaine on Early Postoperative Rehabilitation Training After Total Knee Arthroplasty
Jiajia Li12BCE, Ruiqiang Xia12B, Chunchun Zhu12B, Hong Wu12B, Xutong Zhang12B, Jun Li12F, Jianfeng Ma12ADEG*DOI: 10.12659/MSM.939858
Med Sci Monit 2023; 29:e939858
Abstract
BACKGROUND: Patients experience severe pain in early postoperative rehabilitation after total knee arthroplasty (TKA). This study aimed to compare the effect of femoral nerve block with different concentrations of chloroprocaine on postoperative rehabilitation in patients with TKA.
MATERIAL AND METHODS: Ninety patients who only received unilateral TKA were randomly and equally divided into C1 (1% chloroprocaine 0.2 ml/kg), C2 (2% chloroprocaine 0.2 ml/kg), or NS (0.9% sodium chloride solution 0.2 ml/kg) groups. The patients received rehabilitation 3 times a day on days 3-6 after surgery, and femoral nerve block was performed with corresponding solution 10 min before each training session. We recorded the maximum knee flexion angles (MKFA) and maximum knee extension angles (MKEA) during active exercise on day 7 after surgery, as well as the incidence of MKFA ³100°, American knee society (AKS) scores, and postoperative rehabilitation satisfaction. Adverse effects after administration in each group were also recorded.
RESULTS: Compared with group NS, patients in group C1 and C2 had larger MKFA during active exercise on day 7 after TKA, and had better rehabilitation satisfaction (P<0.05). MKEA, the incidence of MKFA ≥100°, and AKS scores showed no significant differences in the 3 groups. There were more patients with decline of muscle strength in group C2 (P<0.05), and no other adverse reactions were recorded.
CONCLUSIONS: Chloroprocaine for femoral nerve block can be safely used in rehabilitation after TKA and to improve the knee flexion angle in the early postoperative period. Because they may have fewer adverse effects, 1% chloroprocaine 0.2 ml/kg may be preferred.
Keywords: Arthroplasty, Chloroprocaine, Femoral Nerve, Knee Joint, Rehabilitation, Humans, Arthroplasty, Replacement, Knee, Procaine, Drug-Related Side Effects and Adverse Reactions
Background
End-stage knee joint disease seriously affects quality of life and causes great pain. At present, TKA is one of the effective methods to restore knee function. Besides the influence of surgery, early postoperative rehabilitation plays an important role in recovery of knee joint function after surgery. Perioperative rehabilitation can exercise and strengthen muscles, improve local blood circulation, prevent complications such as nerve root adhesion, thrombosis, and knee stiffness, and promote rapid healing of the knee joint [1]. Patients’ return to daily activities can be accelerated with the early introduction of rehabilitation [2]. Additionally, other studies have shown that early rehabilitation training can effectively improve knee function after TKA [3,4], but it is difficult to complete essential rehabilitation because of the postoperative trauma and pain. Thus, a small number of patients might have joint stiffness that affects the normal movement of joints and produces adverse physiological effects [5,6]. Therefore, administration of good analgesia intervention has become a challenge in early functional exercises after TKA.
Postoperative analgesia (such as femoral nerve block) can be used to reduce pain during rehabilitation training after TKA, and a better functional exercise of the knee joint could be carried out, which has already been reported [7,8]. It is believed that the administration of an appropriate dose of local anesthetics to block the femoral nerve can significantly reduce pain during rehabilitation training and help patients overcome their fear of training. However, there is no literature introducing the whole process of postoperative functional exercise, especially the influence of the control of active pain 72 h after surgery on knee joint function, or the evaluation of functions that are important in daily life, such as squatting. As a short-acting local anesthetic, chloroprocaine has fast onset, strong analgesic efficacy, rapid metabolism, synchronous recovery of motor sensation after drug withdrawal, and low toxicity. In real-world clinical practice, the recommended concentration for nerve block is 1–2%, but the appropriate concentration and dose for femoral nerve block for post-TKA rehabilitation have not been studied. The purpose of this study was to investigate the effect of femoral nerve block with different concentrations of chloroprocaine on rehabilitation after TKA.
Material and Methods
ETHICS APPROVAL:
This study was approved by the Ethics Committee of the authors’ affiliated institution [2017 Clinical Scientific Research]. The trial was registered prior to patient enrollment at Clinical Trial Registry (ChiCTR-INR-17012787, Principal investigator: Jianfeng Ma, Date of registration: September 25, 2017). All participants were informed about the study and written consents were obtained.
STUDY DESIGN AND PARTICIPANTS:
We performed a prospective, randomized, controlled, single-center clinical study from September 2017 to December 2021. We selected consecutive 65–80-year-old patients who were scheduled for primary unilateral TKA with American Society of Anesthesiologists (ASA) classification I–II and body mass index (BMI) ≤30 kg/m2. The exclusion criteria were as follows: history of TKA, allergy to morphine or local anesthetic, continuous use of analgesics for 2 weeks or more, history of gastrointestinal ulcers or bleeding, peripheral neuropathy, platelet count <8×109/L, coagulation dysfunction, puncture site infection, history of mental illness, and inability to understand the visual analog scale (VAS). A total of 90 cases were enrolled and divided into 3 equal groups via random number table method. Large-angle rehabilitation training of the knee joint began 48 h after the operation. Before training, 1% chloroprocaine 0.2 ml/kg (group C1), 2% chloroprocaine 0.2 ml/kg (group C2), or 0.9% sodium chloride solution 0.2 ml/kg (group NS) was given through femoral nerve catheterization.
FEMORAL NERVE CATHETERIZATION:
After entering the operating room, the patient was monitored by pulse oximetry, non-invasive blood pressure, and ECG, then the vein access was established. Guided by a 12-mHz high-frequency linear probe (HFL 50/13-6 MHz, M-Turbo, SonoSite, Bothell, WA, USA) and a nerve stimulator (Stimuplex HNS 11, B Braun Medical, Melsongen, Germany), a femoral nerve catheter was introduced into the patient using a nerve stimulator kit (lot no. 1290, Pajunk, Geisingen, Germany).
After local infiltration anesthesia of the skin, a stimulating needle was inserted at a 30~45° angle to the skin about 0.5 cm outside of the ultrasonic probe using an in-plane technique. When the needle tip reached near the femoral nerve, the nerve stimulation current was turned to 0.5 mA to induce quadriceps contraction or patellar lift. Next, the current was reduced to 0.3 mA. If it still could cause to the above reactions, 0.9% sodium chloride solution 10 ml was injected, and a nerve catheter was inserted for about 11 cm. Then, the puncture needle was removed and the catheter secured properly. Finally, 1% lidocaine hydrochloride 15 ml was given. If it could decrease the pain or temperature sensation of skin on the surface of the knee joint within 15 min, the catheterization was confirmed to be successful; otherwise, the catheter was excluded. In addition, a depth of femoral nerve catheterization less than 8 cm suggested the catheter was pulled out.
REHABILITATION TRAINING METHODS:
This was a double-blind, randomized, controlled study in which neither the subjects nor the trainers were aware of the drug used. The patients were randomly allocated to 1 of the 3 groups (group C1: 1% chloroprocaine 0.2 ml/kg, group C2: 2% chloroprocaine 0.2 ml/kg, and group NS: 0.9% sodium chloride solution 0.2 ml/kg) via computer-generated randomization conducted by a team member who was not involved in operations or rehabilitation training after surgery. This team member prepared opaque envelopes in which the intervention type was concealed. These envelopes were opened a few minutes before ultrasound-guided femoral nerve catheterization. Patients were anesthetized prior to surgery by 1 of the 2 physicians. Combined lumbar epidural anesthesia in the lumbar 3–4 intervertebral space was selected. The knee drainage tube and epidural analgesia pump (long-acting low-concentration local anesthetic + morphine/hydromorone) were removed 48 h after the operation, and large-angle rehabilitation training of the operative limb was started. Training and patient assessment were carried out by other members of the team who did not participate in randomization and anesthesia procedures. Flurbiprofen axetil injection 100 mg was administered routinely for intravenous analgesia twice a day in the morning and afternoon. Before rehabilitation, each participant underwent pulse oximetry, non-invasive arterial blood pressure, and electrocardiogram monitoring, followed by injection of corresponding drugs via the femoral nerve catheter. After 10 min, the patients were instructed to complete rehabilitation training (flexion and extension of the knee joint). The training began with passive exercises in which the therapists could help the patients to overcome fear and direct them to move the affected limbs, followed by active exercises. They received femoral nerve block and exercises 3 times every day, and the interval between each administration was at least 4 h. They performed 1 group of exercises every time on days 3 and 4, and 2 groups of exercises on days 5 and 6 after TKA. Each group of exercises included 10 active and 10 passive knee movements. The exercises were completed by a professional rehabilitation team consisting of 3 therapists. After completing the whole rehabilitation, the femoral nerve catheter was removed.
OUTCOME MEASURES:
On day 7 after surgery, the MKFA and MKEA, and the incidence of MKFA ≥100° in each group were recorded. Early start of knee joint mobilization after TKA has already been reported to improve range of motion of the knee, which can predict patient satisfaction after the operation [9,10]. Decreased knee extension and flexion range of motion can lead to functional deficits in many activities of daily life (eg, standing up, walking, stair climbing); therefore, the MKFA and MKEA were chosen to be the primary endpoints. The landmarks used to measure the angles were the greater trochanter of the femur, the proximal head of the fibula, and the lateral malleolus [11].
The VAS and AKS scores on day 7 after surgery were also recorded, as well as postoperative rehabilitation satisfaction (scores were 0~10: 0~2=very dissatisfied, 3~5=dissatisfied, 6~7=generally satisfied, 8~9=satisfactory, and 10=very satisfied). The pain assessment with VAS scores were performed when patients’ active knee motion reached the maximum angle, which were based on a walking scale of 0–10 cm, with 0 points for painless and 10 points for severe pain, and different degrees of pain in between. The patients marked their own pain. AKS scores consist of Knee Score (KS) and Knee Function Score (KFS). The KS rates pain, range of motion, and stability, and the KFS rates the patient’s ability to walk and climb stairs [12]. The pain assessment in KS and KFS do not require large-angle knee joint movement, and cannot reflect the pain of the knee joint at the maximum flexion and extension states.
On days 3–6 after TKA, VAS scores at the third session of active exercises before and after administration were also collected. In addition, we also recorded adverse effects (nausea, vomiting, irritability, drowsiness, confusion, catheter-associated infection, decline of muscle strength, and other complications related to the nervous system) after administration during rehabilitation. When patients could not complete active exercises after administration who had completed active exercises before administration, they were considered to have experienced a decline in muscle strength. In these cases, we waited for the patient’s muscle strength to return to the pre-administration level and then let them complete the exercises.
STATISTICAL ANALYSIS:
Data were statistically analyzed using SPSS software version 25 (SPSS, Inc., Chicago, IL, USA). The Kolmogorov-Smirnov test was used to assess whether variable distributions violated the assumption of normality. Normally distributed measurement data were presented as means±SD, and the inter-group statistical comparison between means were done using one-way analysis of variance. If the numerical variable had a nonnormal distribution or unequal variance, they were expressed as median with interquartile ranges (IQR) and compared by using a nonparametric test. Categorical data were tested by using the χ2 test. Bonferroni corrections were used for post hoc comparisons between any 2 groups. Significance was set at
SAMPLE SIZE ESTIMATION:
According to the pre-experiment results, the mean of MKFA in groups C1, C2, and NS on day 7 after surgery were 102.5±7.1°, 103.8±6.2°, and 97.7±5.8°, respectively. The sample size of each group calculated by PASS 15 software was 25 cases to provide 80% power with a two-sided alpha value of 0.05. A sample size of 30 participants per group was needed, assuming a 20% dropout rate.
Results
PARTICIPANT ENROLLMENT AND CHARACTERISTICS:
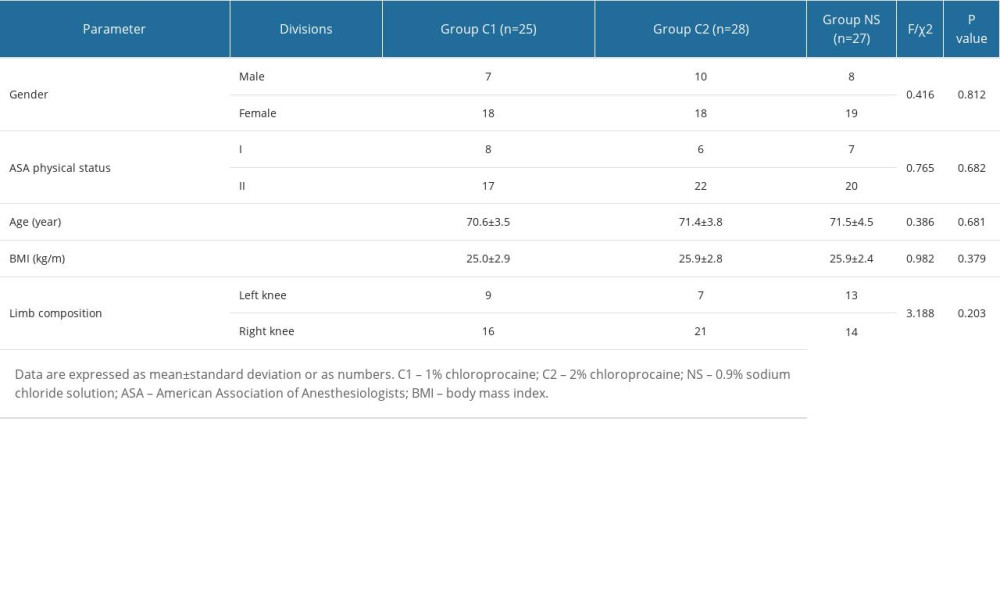
There were 90 patients approached for the study. Finally, 80 patients completed this study and their results were analyzed (Figure 1). In group C1, 3 patients dropped out due to early discharge, 1 patient had femoral nerve catheter blockage, and 1 patient withdrew due to postoperative delirium. In group C2, 1 patient dropped out due to early discharge, and 1 patient pulled out the femoral nerve catheter accidentally. In group NS, 2 patients refused training due to severe pain, and 1 patient unexpectedly pulled out the femoral nerve catheter.
There were no significant differences in gender, ASA physical status, age, BMI, and limb composition among the 3 groups (P>0.05) (Table 1).
COMPARISON OF POSTOPERATIVE RECOVERY ON DAY 7 AFTER TKA: The MKFA of patients in group C1 and C2 on day 7 after surgery were significantly larger than those of patients in group NS (C1 vs NS, P=0.046; C2 vs NS, P=0.025) (Figure 2). There were no significant differences in MKEA of patients among the 3 groups (P>0.05) (Figure 2). The incidence of MKFA ≥100° on day 7 after surgery in the patients of 3 groups had significant differences (P=0.046); but compared with group NS, patients in groups C1 and C2 did not have significantly different incidences of MKFA ≥100° (P>0.05) (Figure 3).
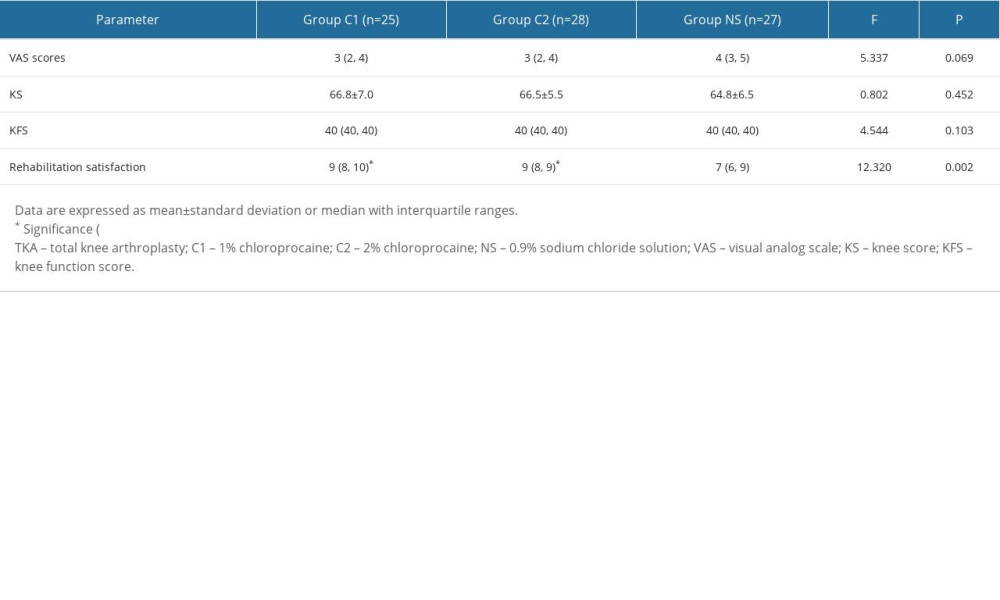
The VAS scores of patients among the 3 groups on day 7 after TKA had no significant differences (P>0.05), while patients in groups C1 and C2 showed higher rehabilitation satisfaction than those in group NS (C1 vs NS, P=0.005; C2 vs NS, P=0.012) (Table 2).
KS and KFS also showed no significant differences in the 3 groups on day 7 after surgery (P>0.05) (Table 2).
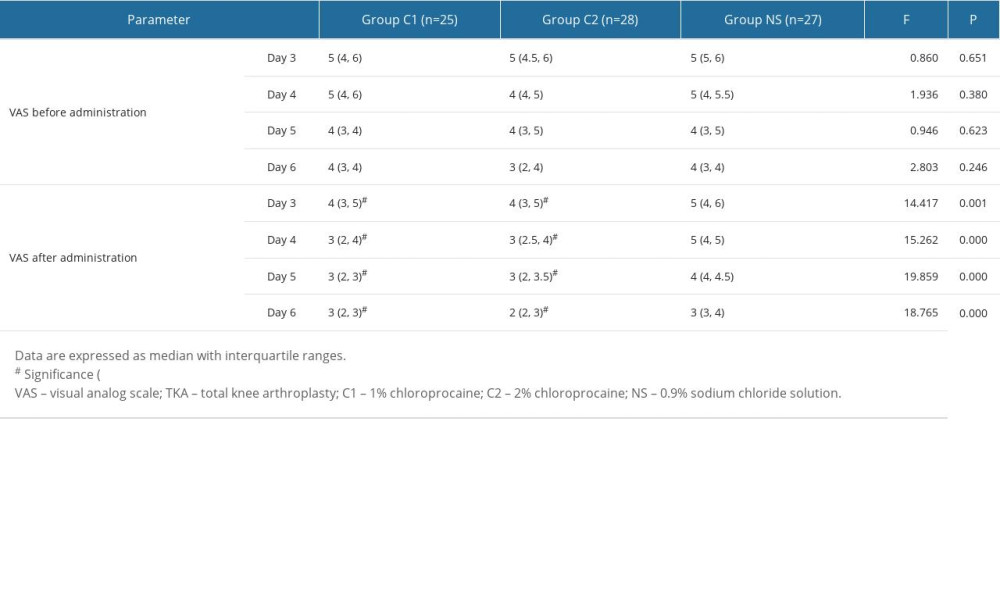
COMPARISON OF VAS SCORES ON DAYS 3–6 AFTER TKA: VAS scores after administration of patients in groups C1 and C2 were significantly lower than those in group NS at each time point (P<0.05). There were no significant differences in VAS scores before administration at each time point in the 3 groups (P>0.05) (Table 3).
COMPARISON OF ADVERSE REACTIONS:
Two patients had difficulty in active knee motion during training in group C1 due to decreased limb muscle strength, while in group C2, 10 patients had the same problem (
Discussion
The regional block technique plays an important role in multimode analgesia after TKA [13,14], as improper management of analgesia seriously affects the rehabilitation of patients and the treatment quality of surgery. In this study, the femoral nerve block with chloroprocaine was used to control pain during rehabilitation training, and it was found that the VAS scores in both groups after administration were significantly decreased. Therefore, both concentrations of chloroprocaine could significantly reduce pain during active exercise with the same effect.
The quality of knee recovery is not only related to the quality of the operation itself, but also depends on the early postoperative functional exercise. According to the results, it is worth mentioning that on day 7 when no drugs were given, the MKFAs were better in groups C1 and C2 than those in group NS, while on day 7 there were no significant differences in VAS scores among the 3 groups during training, which was in a completely natural state. Therefore, we believe that this method can improve the early motion of the knee joint. In many studies, range of motion was used as the main index, but it could not distinguish whether the improvement of knee motion was caused by the change of knee flexion or extension angle. In this study, it was found that femoral nerve block had a significant effect on the knee flexion angle; this was because the bending of the knee was dominated by the stretching of the quadriceps and other anterior muscles, while femoral nerve block could relax the anterior muscles and produce a good analgesic effect on the surface of the knee joint.
Knee extension angle is not only affected by postoperative pain, but also by preoperative knee extension angle, postoperative swelling, and other factors. Femoral nerve block in this study was only effective on the anterior muscle group of the thigh, so its influence on knee extension angle was relatively limited. This may be the reason why there was no difference in MKEA of patients in the 3 groups. Whether increasing the sample size will result in a different conclusion needs to be further studied. Previous studies have shown that functional deficits depend on decreasing the knee flexion angle [15]. The greater the knee flexion angle, the better ability to move. Escramilla et al [16] believed that knee flexion angle above 100° is considered to be able to squat, which enables people to complete kneeling and cross-legged sitting, which can greatly improve the quality of daily life. Thus, in our study, we further compared the number of patients with MKFA above 100° in the 3 groups, and we found that there were more patients in groups C1 and C2 than in group NS on day 7 after TKA. However, there were no significant differences in the incidence of MKFA ≥100° of pairwise comparisons after correction. This may be due to the small sample size. So, whether femoral nerve block for early postoperative rehabilitation will play a role in achieving high quality functions such as squatting needs further study. AKS scores are commonly used to evaluate knee joint function [17,18]. In our study, AKS scores on day 7 after surgery showed no significant difference among the 3 groups, which was consistent with the results reported by Sakai et al [19]. We noticed that pain assessment occupied a greater weight in KS, and KFS mainly focuses on daily basic functions (walking and climbing stairs) without squatting and other actions, that may result in negative results.
Previous studies [19,20] have focused on continuous femoral nerve block (CFNB) continuous infusion within 3 days after surgery. It is believed that the enhancement effect of CFNB on postoperative training is mainly through reducing postoperative pain, postoperative knee swelling, and muscle spasms. Combined with the results, the VAS scores on days 3~6 after TKA still showed active pain; thus, it was necessary to continue the use of nerve block to achieve a better training effect during this period.
A possible decline in the quadriceps femoris muscle strength is considered as a defect of CFNB [21,22]. Ilfeld et al [23] believed that continuous infusion will cause a decrease in quadriceps muscle strength, while other researchers [24,25] believed that it can improve the postoperative walking training ability and achieve the rehabilitation standards earlier. However, if local anesthetics affect the quadriceps muscle strength for a long time, it will not only increase the risk of falling [26], but also restrict early joint function exercise. Therefore, in this study, chloroprocaine with an onset time of 6–10 min and a duration of action of about 45–60 min was used as a local anesthetic. The results showed that there were patients in groups C1 and C2 who had difficulty in active knee joint movement during training due to the weakness of quadriceps femoris muscle and returned to normal levels within 1 h after administration. Adductor canal block (ACB) is considered to be a blocking method that can retain femoral nerve analgesia and has little influence on quadriceps femoris muscle strength [27,28]. However, some authors believed that femoral nerve block (FNB) was associated with the perception of less severe pain after TKA [29]. Kim et al [30] reported that FNB may be superior to ACB in analgesic intensity. In addition, further study is needed to determine if there is catheter displacement or detachment in the patients with ACB during training.
Long-term CFNB is considered to have a risk of infection [19,20]; thus, there are few reports about CFNB for more than 3 days. In our study, it took 6 days to remove the femoral nerve catheter, and none of the patients had local or systemic infections. This is closely related to strict aseptic operation during catheterization and replacement of the film. In addition, 65–80-old-year patients were recruited for this study. This was mainly based on the literature [31] and the age distribution of patients undergoing TKA in our hospital, and this group of people may more easily communicate and cooperate with the rehabilitation. Older people may be less compliant and the number of younger patients was small. Therefore, we think our age group is representative.
Limitations of this study are: small sample size; no long-term follow-up was performed while considering the influence of some objective factors, such as patients’ noncooperation leading to loss to follow-up, and differences in the implementation of patients’ rehabilitation after discharge that may have a big impact on the results; no specific evaluation of muscle strength was made; no comparison with the preoperative knee angle of patients was made, and the correlation with patient outcome could not be ruled out; and no further analysis of walking distance, climbing stairs and other activity performance after administration were made. In addition, AKS, which is widely used in TKA studies, is a good tool to evaluate the daily activities of the knee joint, but it is not sensitive to the nuances of the knee joint angles, so the selection of other scales that are more sensitive to the changes of the knee joint angles may produce more accurate results.
Conclusions
In conclusion, injection of 1% or 2% chloroprocaine 0.2 ml/kg through femoral nerve catheterization can relieve the pain of patients in early rehabilitation after TKA, and improve the knee flexion angle and the satisfaction of patients. The 1% concentration is less likely to decrease muscle strength, and may be more suitable for early postoperative rehabilitation.
Figures
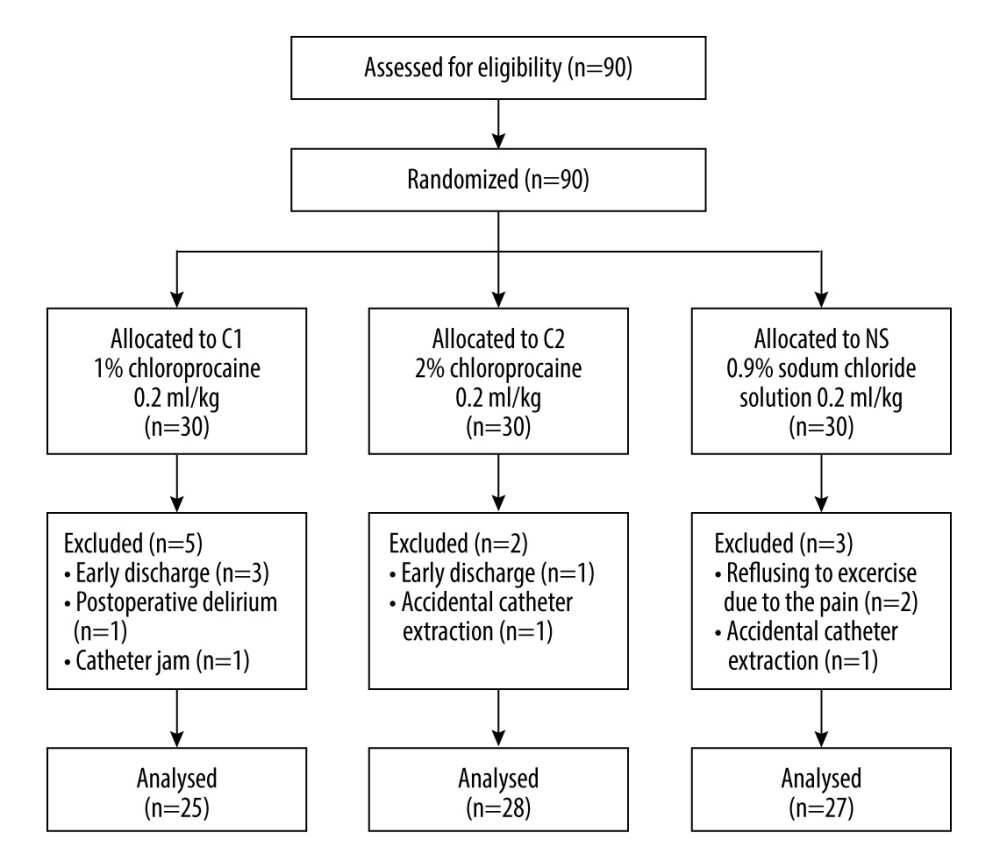 Figure 1. Consort flow diagram for study participation. C1 – 1% chloroprocaine; C2 – 2% chloroprocaine; NS – 0.9% sodium chloride solution.
Figure 1. Consort flow diagram for study participation. C1 – 1% chloroprocaine; C2 – 2% chloroprocaine; NS – 0.9% sodium chloride solution. 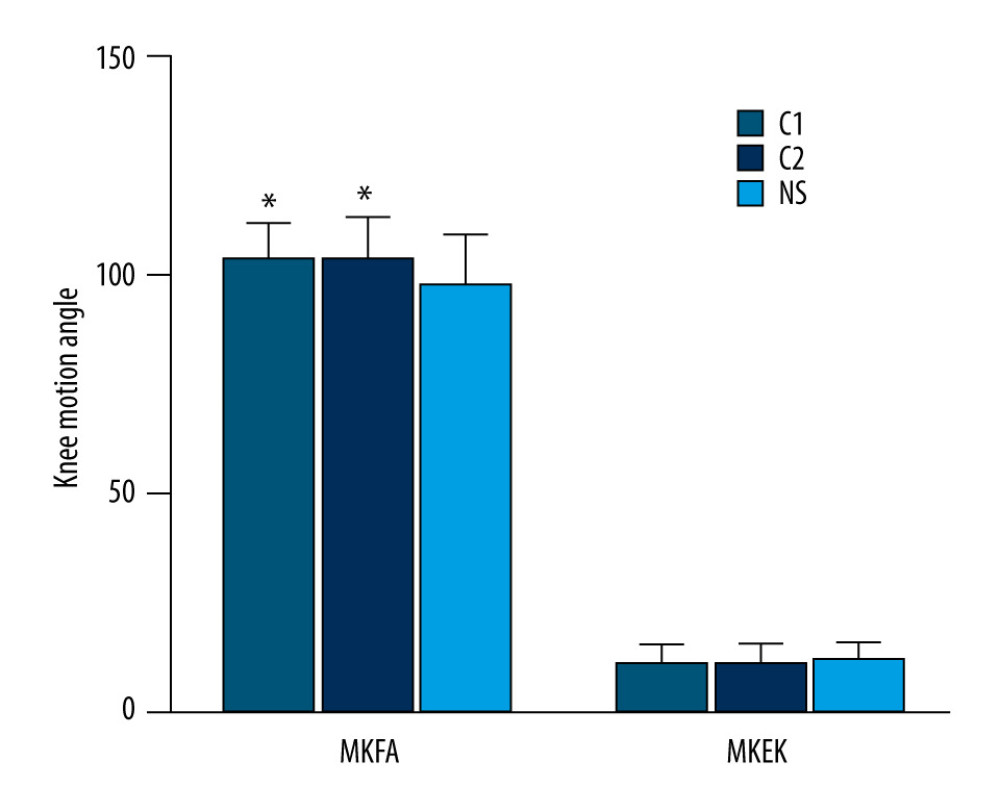 Figure 2. The knee motion angles of patients in the 3 groups on day 7 after TKA. * Significance (P<0.05) was found compared with group NS. TKA – total knee arthroplasty; MKFA – the maximum knee flexion angles; MKEA – the maximum knee extension angles; C1 – 1% chloroprocaine; C2 – 2% chloroprocaine; NS – 0.9% sodium chloride solution. Figures were generated using Prism by Graph Pad Dotmatics version 8.
Figure 2. The knee motion angles of patients in the 3 groups on day 7 after TKA. * Significance (P<0.05) was found compared with group NS. TKA – total knee arthroplasty; MKFA – the maximum knee flexion angles; MKEA – the maximum knee extension angles; C1 – 1% chloroprocaine; C2 – 2% chloroprocaine; NS – 0.9% sodium chloride solution. Figures were generated using Prism by Graph Pad Dotmatics version 8. 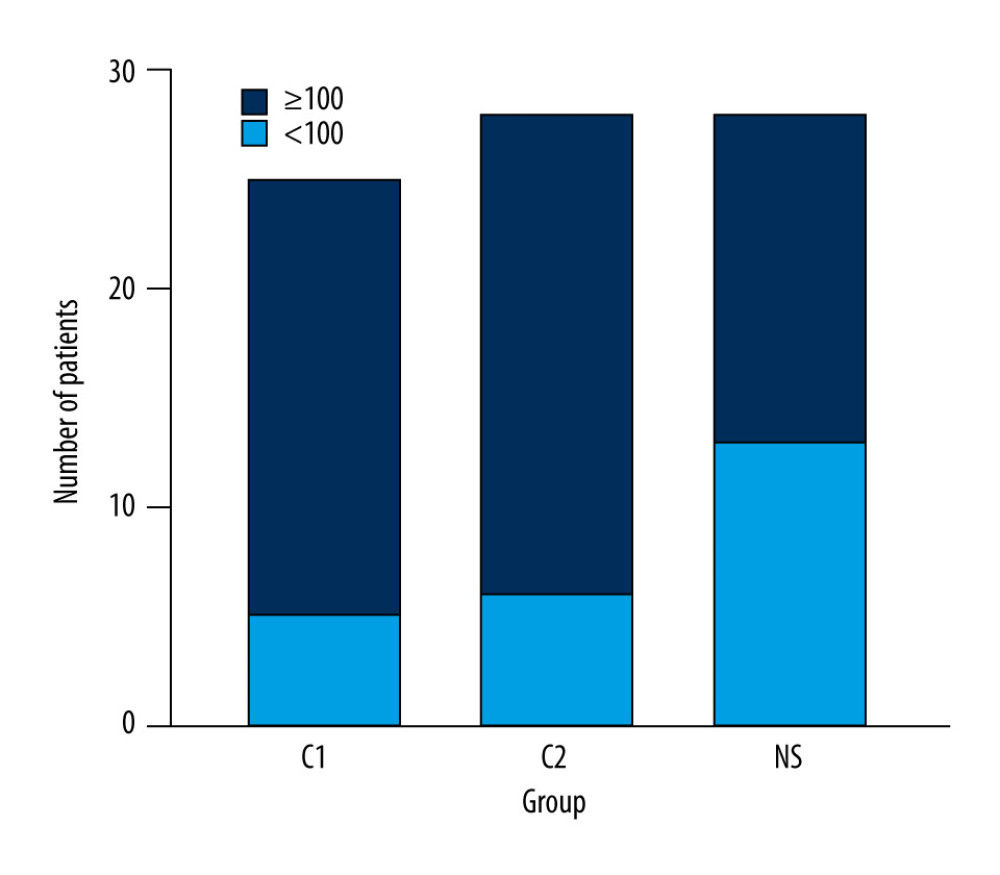 Figure 3. Comparison of the incidence of MKFA ≥100° in patients of the 3 groups on day 7 after TKA. * Significance (P<0.05) was found compared with the incidence of MKFA ≥100° in patients of group NS. TKA – total knee arthroplasty; MKFA – the maximum knee flexion angles; C1 – 1% chloroprocaine; C2 – 2% chloroprocaine; NS – 0.9% sodium chloride solution. Figures were generated using Prism by Graph Pad Dotmatics version 8.
Figure 3. Comparison of the incidence of MKFA ≥100° in patients of the 3 groups on day 7 after TKA. * Significance (P<0.05) was found compared with the incidence of MKFA ≥100° in patients of group NS. TKA – total knee arthroplasty; MKFA – the maximum knee flexion angles; C1 – 1% chloroprocaine; C2 – 2% chloroprocaine; NS – 0.9% sodium chloride solution. Figures were generated using Prism by Graph Pad Dotmatics version 8. References
1. Franz A, Queitsch FP, Behringer M, Blood flow restriction training as a prehabilitation concept in total knee arthroplasty: A narrative review about current preoperative interventions and the potential impact of BFR: Med Hypotheses, 2018; 110; 53-59
2. Lisi C, Caspani P, Bruggi M, Early rehabilitation after elective total knee arthroplasty: Acta Biomed, 2017; 88(4S); 56-61
3. Bade MJ, Struessel T, Dayton M, Early high-intensity versus low-intensity rehabilitation after total knee arthroplasty: A randomized controlled trial: Arthritis Care Res (Hoboken), 2017; 69(9); 1360-68
4. Li R, Xu Z, Li Y, Luo J, Effect of acupuncture combined with early rehabilitation training on postoperative dysfunction and quality of life of patients undergoing total knee arthroplasty: Am J Transl Res, 2021; 13(6); 6407-14
5. Chua MJ, Hart AJ, Mittal R, Early mobilisation after total hip or knee arthroplasty: A multicentre prospective observational study: PLoS One, 2017; 12(6); e0179820
6. Zhu SA, Chen PF, Yang Chen Y, 3D-printed extracellular matrix/polyethylene glycol diacrylate hydrogel incorporating the anti-inflammatory phytomolecule honokiol for regeneration of osteochondral defects: Am J Sports Med, 2020; 48(11); 2808-18
7. Lee HH, Kwon HM, Lee WS, Effectiveness of ERAS (enhanced recovery after surgery) protocol via peripheral nerve block for total knee arthroplasty: J Clin Med, 2022; 11(12); 3354
8. Li DH, Alqwbani M, Wang QR, Efficacy of adductor canal block combined with additional analgesic methods for postoperative analgesia in total knee arthroplasty: A prospective, double-blind, randomized controlled study: J Arthroplasty, 2020; 35(12); 3554-62
9. Labraca NS, Castro-Sánchez AM, Matarán-Peñarrocha GA, Benefits of starting rehabilitation within 24 hours of primary total knee arthroplasty: Randomized clinical trial: Clin Rehabil 6, 2011; 25; 557-66
10. Van Onsem S, Verstraete M, Dhont S, Improved walking distance and range of motion predict patient satisfaction after TKA: Knee Surg Sports Traumatol Arthrosc, 2018; 26(11); 3272-79
11. Mutsuzaki H, Takeuchi R, Mataki Y, Target range of motion for rehabilitation after total knee arthroplasty: J Rural Med, 2017; 12(1); 33-37
12. Insall JN, Dorr LD, Scott RD, Rationale of the Knee Society clinical rating system: Clin Orthop Relat Res, 1989; 248; 13-14
13. Hsu YP, Hsu CW, Chu KCW, Efficacy and safety of femoral nerve block for the positioning of femur fracture patients before a spinal block – a systematic review and meta-analysis: PLoS One, 2019; 14(5); e0216337
14. Ghimire A, Bhattarai B, Koirala S, Analgesia before performing subarachnoid block in the sitting position in patients with proximal femoral fracture: A comparison between fascia iliaca block and femoral nerve block: Kathmandu Univ Med J, 2015; 13(50); 152-55
15. Magit D, Wolff A, Sutton K, Arthrofibrosis of the knee: J Am Acad Orthop Surg, 2007; 15(11); 682-94
16. Escamilla RF, Fleisig GS, Lowry TM, A three-dimensional biomechanical analysis of the squat during varying stance widths: Med Sci Sports Exerc, 2001; 33(6); 984-98
17. Sun ML, Zhang Y, Peng Y, Accuracy of a Novel 3D-printed patient-specific intramedullary guide to control femoral component rotation in total knee arthroplasty: Orthop Surg, 2020; 12(2); 429-41
18. Tiwari V, Lee J, Sharma G, Temporal patterns of commonly used clinical outcome scales during a 5-year period after total knee arthroplasty: J Orthop Traumatol, 2019; 20(1); 16-25
19. Sakai N, Inoue T, Kunugiza Y, Continuous femoral versus epidural block for attainment of 120° knee flexion after total knee arthroplasty: A randomized controlled trial: J Arthroplasty, 2013; 28(5); 807-14
20. Zinkus J, Mockutė L, Gelmanas A, Comparison of 2 analgesia modalities in total knee replacement surgery: Is there an effect on knee function rehabilitation?: Med Sci Monit, 2017; 23; 3019-25
21. Pelt CE, Anderson AW, Anderson MB, Postoperative falls after total knee arthroplasty in patients with a femoral nerve catheter: Can we reduce the incidence?: J Arthroplasty, 2014; 29(6); 1154-57
22. Tian Y, Tang S, Sun S, Comparison between local infiltration analgesia with combined femoral and sciatic nerve block for pain management after total knee arthroplasty: J Orthop Surg Res, 2020; 15(1); 41-44
23. Ilfeld BM, Moeller LK, Mariano ER, Continuous peripheral nerve blocks: Is local anesthetic dose the only factor, or do concentration and volume influence infusion effects as well?: Anesthesiology, 2010; 112(2); 347-54
24. Ilfeld BM, Le LT, Meyer RS, Ambulatory continuous femoral nerve blocks decrease time to discharge readiness after tricompartment total knee arthroplasty: A randomized, triple-masked, placebo-controlled study: Anesthesiology, 2008; 108(4); 703-13
25. Ilfeld BM, Mariano ER, Girard PJ, A multicenter, randomized, triple-masked, placebo-controlled trial of the effect of ambulatory continuous femoral nerve blocks on discharge-readiness following total knee arthroplasty in patients on general orthopaedic wards: Pain, 2010; 150(3); 477-84
26. Luo ZY, Yu QP, Zeng WN, Adductor canal block combined with local infiltration analgesia with morphine and betamethasone show superior analgesic effect than local infiltration analgesia alone for total knee arthroplasty: A prospective randomized controlled trial: BMC musculoskel dis, 2022; 23(1); 468
27. Rodriguez-Patarroyo FA, Cuello N, Molloy R, A guide to regional analgesia for total knee arthroplasty: EFORT Open Rev, 2021; 6(12); 1181-92
28. Grosso MJ, Murtaugh T, Lakra A, Adductor canal block compared with periarticular bupivacaine injection for total knee arthroplasty: a prospective randomized trial: J Bone Joint Surg, 2018; 100(13); 1141-46
29. Borys M, Domagała M, Wencław K, Continuous femoral nerve block is more effective than continuous adductor canal block for treating pain after total knee arthroplasty: A randomized, double-blind, controlled trial: Medicine, 2019; 98(39); e17358
30. Kim DH, Lin Y, Goytizolo EA, Adductor canal block versus femoral nerve block for total knee arthroplasty: A prospective, randomized, controlled trial: Anesthesiology, 2014; 120(3); 540-50
31. Postler A, Lützner C, Beyer F, Analysis of total knee arthroplasty revision causes: BMC Musculoskel Dis, 2018; 19(1); 55
Figures
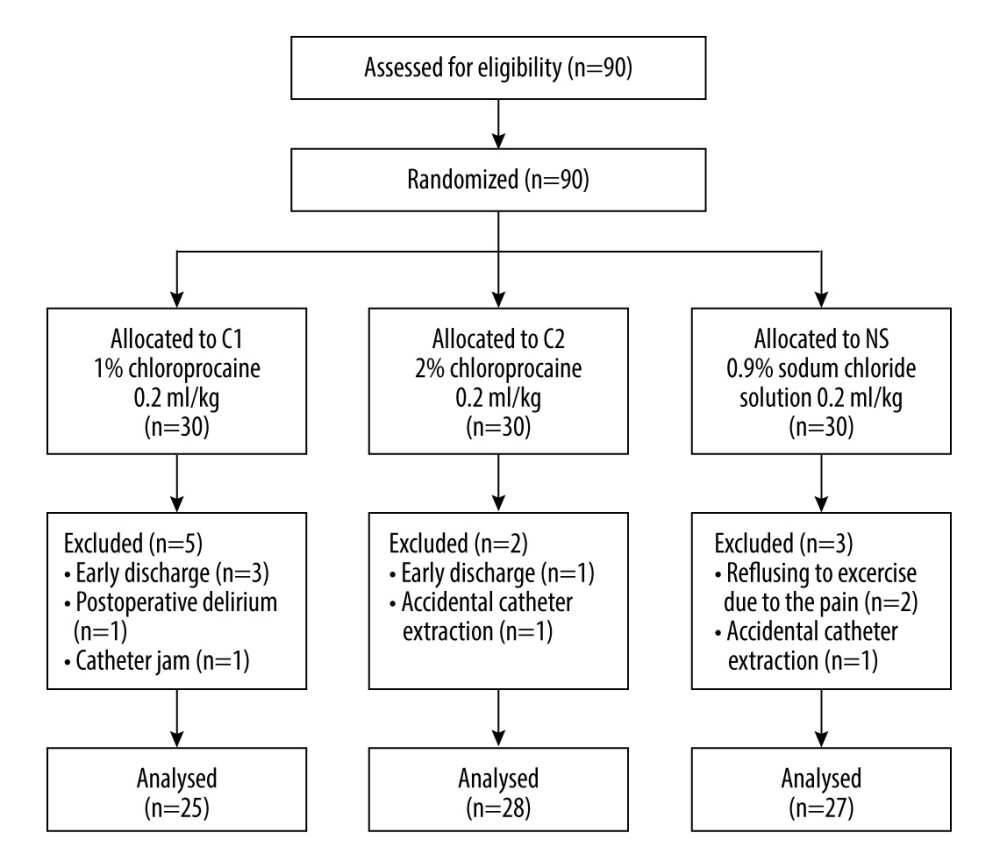 Figure 1. Consort flow diagram for study participation. C1 – 1% chloroprocaine; C2 – 2% chloroprocaine; NS – 0.9% sodium chloride solution.
Figure 1. Consort flow diagram for study participation. C1 – 1% chloroprocaine; C2 – 2% chloroprocaine; NS – 0.9% sodium chloride solution.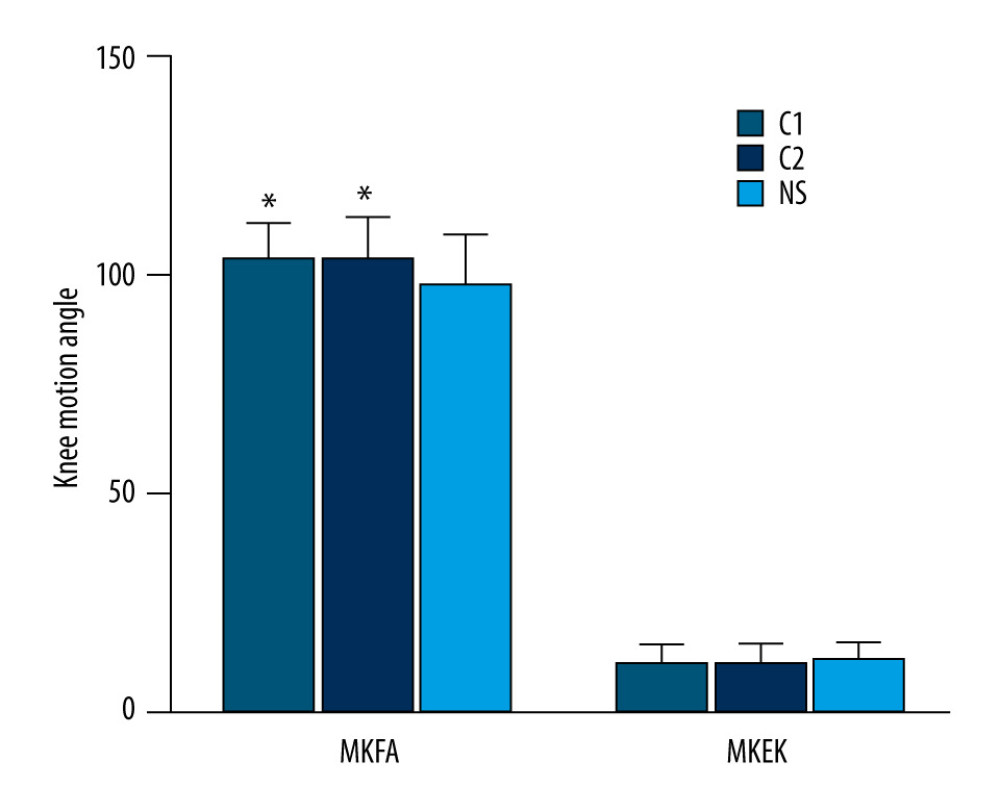 Figure 2. The knee motion angles of patients in the 3 groups on day 7 after TKA. * Significance (P<0.05) was found compared with group NS. TKA – total knee arthroplasty; MKFA – the maximum knee flexion angles; MKEA – the maximum knee extension angles; C1 – 1% chloroprocaine; C2 – 2% chloroprocaine; NS – 0.9% sodium chloride solution. Figures were generated using Prism by Graph Pad Dotmatics version 8.
Figure 2. The knee motion angles of patients in the 3 groups on day 7 after TKA. * Significance (P<0.05) was found compared with group NS. TKA – total knee arthroplasty; MKFA – the maximum knee flexion angles; MKEA – the maximum knee extension angles; C1 – 1% chloroprocaine; C2 – 2% chloroprocaine; NS – 0.9% sodium chloride solution. Figures were generated using Prism by Graph Pad Dotmatics version 8.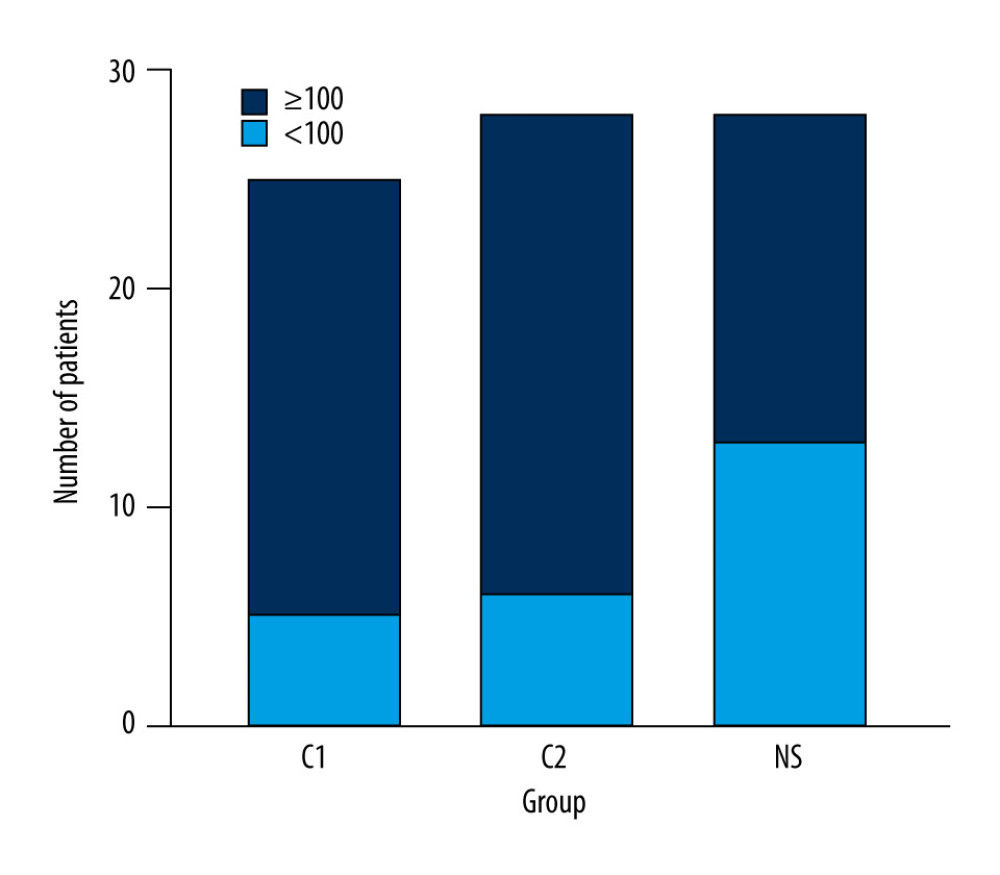 Figure 3. Comparison of the incidence of MKFA ≥100° in patients of the 3 groups on day 7 after TKA. * Significance (P<0.05) was found compared with the incidence of MKFA ≥100° in patients of group NS. TKA – total knee arthroplasty; MKFA – the maximum knee flexion angles; C1 – 1% chloroprocaine; C2 – 2% chloroprocaine; NS – 0.9% sodium chloride solution. Figures were generated using Prism by Graph Pad Dotmatics version 8.
Figure 3. Comparison of the incidence of MKFA ≥100° in patients of the 3 groups on day 7 after TKA. * Significance (P<0.05) was found compared with the incidence of MKFA ≥100° in patients of group NS. TKA – total knee arthroplasty; MKFA – the maximum knee flexion angles; C1 – 1% chloroprocaine; C2 – 2% chloroprocaine; NS – 0.9% sodium chloride solution. Figures were generated using Prism by Graph Pad Dotmatics version 8. Tables
In Press
08 Mar 2024 : Animal Research
Modification of Experimental Model of Necrotizing Enterocolitis (NEC) in Rat Pups by Single Exposure to Hyp...Med Sci Monit In Press; DOI: 10.12659/MSM.943443
18 Apr 2024 : Clinical Research
Comparative Analysis of Open and Closed Sphincterotomy for the Treatment of Chronic Anal Fissure: Safety an...Med Sci Monit In Press; DOI: 10.12659/MSM.944127
08 Mar 2024 : Laboratory Research
Evaluation of Retentive Strength of 50 Endodontically-Treated Single-Rooted Mandibular Second Premolars Res...Med Sci Monit In Press; DOI: 10.12659/MSM.944110
11 Mar 2024 : Clinical Research
Comparison of Effects of Sugammadex and Neostigmine on Postoperative Neuromuscular Blockade Recovery in Pat...Med Sci Monit In Press; DOI: 10.12659/MSM.942773
Most Viewed Current Articles
17 Jan 2024 : Review article
Vaccination Guidelines for Pregnant Women: Addressing COVID-19 and the Omicron VariantDOI :10.12659/MSM.942799
Med Sci Monit 2024; 30:e942799
14 Dec 2022 : Clinical Research
Prevalence and Variability of Allergen-Specific Immunoglobulin E in Patients with Elevated Tryptase LevelsDOI :10.12659/MSM.937990
Med Sci Monit 2022; 28:e937990
16 May 2023 : Clinical Research
Electrophysiological Testing for an Auditory Processing Disorder and Reading Performance in 54 School Stude...DOI :10.12659/MSM.940387
Med Sci Monit 2023; 29:e940387
01 Jan 2022 : Editorial
Editorial: Current Status of Oral Antiviral Drug Treatments for SARS-CoV-2 Infection in Non-Hospitalized Pa...DOI :10.12659/MSM.935952
Med Sci Monit 2022; 28:e935952