Abstract
Background
When non-curative resection is confirmed after endoscopic resection (ER) of early gastric cancer (EGC), delayed surgery is recommended because it provides favorable survival outcomes. Long-term outcome after surgery of EGC with or without previous ER has not been evaluated.
Objective
The aim of this study was to compare the long-term oncologic safety between primary surgery and delayed surgery after ER.
Methods
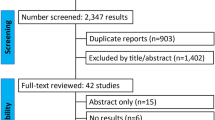
Patients who had undergone curative surgery (R0) for EGC were included and were divided into primary and delayed surgery groups. Primary surgery was defined as gastrectomy without ER for EGC, whereas delayed surgery was defined as additional curative gastrectomy due to non-curative resection after ER; an average delay of 21.5 days (range 1–195) was observed. Propensity score matching was performed. The primary outcome was overall survival (OS) and the secondary outcomes were cancer-specific survival (CSS) and disease-free survival (DFS).
Results
After propensity score matching, 1439 patients were included, of whom 1042 (72.4%) were in the primary surgery group and 397 (27.6%) were in the delayed surgery group. The OS (hazard ratio [HR] 0.87, 95% confidence interval [CI] 0.59–1.27; p = 0.459), CSS (HR 0.47, 95% CI 0.15–1.47; p = 0.196), and DFS (HR 0.54, 95% CI 0.15–1.90; p = 0.334) were not different.
Conclusions
The long-term outcomes of delayed surgery after non-curative ER for EGC were non-inferior to primary surgery. Therefore, an attempt for ER of EGC that satisfies the absolute and expanded indication seems justified for preventing gastrectomy. In case of non-curative resection after ER, additional delayed surgery should be performed.



Similar content being viewed by others
References
Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer. 2017;20:1–19.
Abdelfatah MM, Barakat M, Lee H, et al. The incidence of lymph node metastasis in early gastric cancer according to the expanded criteria in comparison with the absolute criteria of the Japanese Gastric Cancer Association: a systematic review of the literature and meta-analysis. Gastrointest Endosc. 2018;87:338–47.
Park CH, Yang DH, Kim JW, et al. Clinical practice guideline for endoscopic resection of early gastrointestinal cancer. Clin Endosc. 2020;53:142–66.
Pyo JH, Lee H, Min YW, et al. Indication for endoscopic treatment based on the risk of lymph node metastasis in patients with Siewert type II/III early gastric cancer. Gastric Cancer. 2018;21:672–9.
Lee S, Choi KD, Han M, et al. Long-term outcomes of endoscopic submucosal dissection versus surgery in early gastric cancer meeting expanded indication including undifferentiated-type tumors: a criteria-based analysis. Gastric Cancer. 2018;21:490–9.
Jeon HK, Kim GH, Lee BE, et al. Long-term outcome of endoscopic submucosal dissection is comparable to that of surgery for early gastric cancer: a propensity-matched analysis. Gastric Cancer. 2018;21:133–43.
Pyo JH, Lee H, Min BH, et al. Long-term outcome of endoscopic resection vs. surgery for early gastric cancer: a non-inferiority-matched cohort study. Am J Gastroenterol. 2016;111:240–9.
Pyo JH, Lee H, Min BH, et al. Comparison of long-term outcomes after non-curative endoscopic resection in older patients with early gastric cancer. Ann Surg Oncol. 2017;24:2624–31.
Kim YI, Kim YA, Kim CG, et al. Serial intermediate-term quality of life comparison after endoscopic submucosal dissection versus surgery in early gastric cancer patients. Surg Endosc. 2018;32:2114–22.
Takenaka R, Kawahara Y, Okada H, et al. Risk factors associated with local recurrence of early gastric cancers after endoscopic submucosal dissection. Gastrointest Endosc. 2008;68:887–94.
Hirasawa K, Kokawa A, Oka H, et al. Risk assessment chart for curability of early gastric cancer with endoscopic submucosal dissection. Gastrointest Endosc. 2011;74:1268–75.
Jung H, Bae JM, Choi MG, Noh JH, Sohn TS, Kim S. Surgical outcome after incomplete endoscopic submucosal dissection of gastric cancer. Br J Surg. 2011;98:73–8.
Suzuki S, Gotoda T, Hatta W, et al. Survival benefit of additional surgery after non-curative endoscopic submucosal dissection for early gastric cancer: a propensity score matching analysis. Ann Surg Oncol. 2017;24:3353–60.
Lai JF, Kim S, Kim K, et al. Prediction of recurrence of early gastric cancer after curative resection. Ann Surg Oncol. 2009;16:1896–902.
Lee HJ, Kim YH, Kim WH, et al. Clinicopathological analysis for recurrence of early gastric cancer. Jpn J Clin Oncol. 2003;33:209–14.
Youn HG, An JY, Choi MG, Noh JH, Sohn TS, Kim S. Recurrence after curative resection of early gastric cancer. Ann Surg Oncol. 2010;17:448–54.
Li ZY, Zhang QW, Teng LM, Zhang CH, Huang Y. Comparable rates of lymph node metastasis and survival between diffuse type and intestinal type early gastric cancer patients: a large population-based study. Gastrointest Endosc. 2019;90:84–95.e10.
Zhao B, Zhang J, Zhang J, et al. Risk factors associated with lymph node metastasis for early gastric cancer patients who underwent non-curative endoscopic resection: a systematic review and meta-analysis. J Gastrointest Surg. 2019;23:1318–28.
Niwa H, Ozawa R, Kurahashi Y, et al. The eCura system as a novel indicator for the necessity of salvage surgery after non-curative ESD for gastric cancer: a case–control study. PLoS One. 2018;13:e0204039.
Author information
Authors and Affiliations
Contributions
Study concept and design: Hyuk Lee. Acquisition, analysis, or interpretation of data: Ji Eun Na, Yeong Gi Kim, Tae Jun Kim, and Hyuk Lee. Writing and drafting of the manuscript: Ji Eun Na and Tae Jun Kim. Critical revision of the manuscript for important intellectual content: Tae Jun Kim, Hyuk Lee, Yang Won Min, Byung-Hoon Min, Jun Haeng Lee, Poong-Lyul Rhee, and Jae J. Kim. Statistical analysis: Seon Yeong Baek and Min Su Park. All authors approved the final submission.
Corresponding authors
Ethics declarations
Disclosures
Ji Eun Na, Yeong Gi Kim, Tae Jun Kim, Hyuk Lee, Yang Won Min, Byung-Hoon Min, Jun Haeng Lee, Seon Yeong Baek, Min Su Park, Poong-Lyul Rhee, and Jae J. Kim disclose no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Na, J.E., Kim, Y.G., Kim, T.J. et al. Long-Term Safety of Delayed Surgery After Upfront Endoscopic Resection for Early Gastric Cancer: A Propensity Matched Study. Ann Surg Oncol 28, 106–113 (2021). https://doi.org/10.1245/s10434-020-08769-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-08769-z