Abstract
Background
Minimal data have previously emerged from studies regarding the factors associated with recurrence in patients with ypT0N0M0 status. The purpose of the study was to predict survival and recurrence in patients with pathological complete response (pCR) following chemoradiotherapy (CRT) and surgery for esophageal cancer (EC).
Methods
Among 2944 consecutive patients with EC operations in 30 centers between 2000 and 2010, patients treated with neoadjuvant CRT followed by surgery who achieved pCR (n = 191) were analyzed. The factors associated with survival and recurrence were analyzed using a Cox proportional hazard regression analysis.
Results
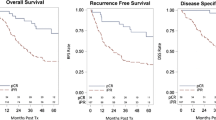
Among 593 patients who underwent neoadjuvant CRT followed by esophagectomy, pCR was observed in 191 patients (32.2 %). Recurrence occurred in 56 (29.3 %) patients. The median time to recurrence was 12 months. The factors associated with recurrence were postoperative complications grade 3–4 [odds ratio (OR): 2.100; 95 % confidence interval (CI) 1.008–4.366; p = 0.048) and adenocarcinoma histologic subtype (OR 2.008; 95 % CI 0.1.06–0.3.80; p = 0.032). The median overall survival was 63 months (95 % CI 39.3–87.1), and the median disease-free survival was 48 months (95 % CI 18.3–77.4). Age (>65 years) [hazard ratio (HR): 2.166; 95 % CI 1.170–4.010; p = 0.014), postoperative complications grades 3–4 [HR 2.099; 95 % CI 1.137–3.878; p = 0.018], and radiation dose (<40 Gy) (HR 0.361; 95 % CI 0.159–0.820; p = 0.015) were identified as factors associated with survival.
Conclusions
An intensive follow-up may be beneficial for patients with EC who achieve pCR and who develop major postoperative complications or the adenocarcinoma histologic subtype.
Similar content being viewed by others
References
Siegel R, Naishadham D, Jemal A. Cancer statistics, 2013. CA Cancer J Clin. 2013;63:11–30.
Berrino F, De Angelis R, Sant M, et al. Survival for eight major cancers and all cancers combined for european adults diagnosed in 1995-99: results of EUROCARE-4 Study. Lancet Oncol. 2007;8:773–83.
Allum WH, Stenning SP, Bancewicz J, et al. Long-term results of a randomized trial of surgery with or without preoperative chemotherapy in esophageal cancer. J Clin Oncol. 2009;27:5062–7.
Mariette C, Dahan L, Mornex F, et al. Surgery alone versus chemoradiotherapy followed by surgery for stage I and II esophageal cancer: final analysis of randomized controlled Phase III Trial FFCD 9901. J Clin Oncol. 2014;32:2416-22.
van Hagen P, Hulshof MCCM, van Lanschot JJB, et al. Preoperative chemoradiotherapy for esophageal or junctional cancer. N Eng J Med. 2012;366:2074–84.
Sjoquist KM, Burmeister BH, Smithers BM, et al. Survival after neoadjuvant chemotherapy or chemoradiotherapy for resectable oesophageal carcinoma: an updated meta-analysis. Lancet Oncol. 2011;12:681–92.
Stahl M, Mariette C, Haustermans K, et al. Oesophageal cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2013;24(Suppl 6):vi51–vi56.
Francis AM, Sepesi B, Correa AM, et al. The influence of histopathologic tumor viability on long term survival and recurrence rates following neoadjuvant therapy for esophageal adenocarcinoma. Ann Surg. 2013;258:500–7.
van Hagen P, Wijnhoven BPL, Nafteux P, et al. Recurrence pattern in patients with a pathologically complete response after neoadjuvant chemoradiotherapy and surgery for oesophageal cancer. Br J Surg. 2013;100:267–73.
Meredith KL, Weber JM, Turaga KK, et al. Pathologic response after neoadjuvant therapy is the major determinant of survival in patients with esophageal cancer. Ann Surg Oncol. 2010;17:1159–67.
Vallböhmer D, Hölscher AH, DeMeester S, et al. A multicenter study of survival after neoadjuvant radiotherapy/chemotherapy and esophagectomy for Ypt0n0m0r0 esophageal cancer. Ann Surg. 2010;252:744–9.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Edge SB, Byrd DR, Compton CC, et al. AJCC cancer staging manual, 7th edn. New York: Springer; 2010.
Ott K, Blank S, Becker K, et al. Factor predicting prognosis and recurrence in patients with esophago-gastric adenocarcinoma and histopathological response with less than 10 % residual tumor. Langenbecks Arch Surg. 2013;398:239–49.
Schneider PM, Baldus SE, Metzger R, et al. Histomorphologic tumor regression and lymph node metastases determine prognosis following neoadjuvant radiochemotherapy for esophageal cancer. Ann Surg. 2005;242:684–92.
Donohoe CL, O’Farell NJ, Grant T, et al. Classification of pathologic response to neoadjuvant therapy in esophageal and junctional cancer. Ann Surg. 2013;258:784–92.
Chirieac LR, Swicher SG, Ajani JA, et al. Posttherapy pathologic stage predicts survival in patient with esophageal carcinoma receiving preoperative chemoradiation. Cancer. 2005;103:1347–55.
Smit JK, Güler S, Beukema JC, et al. Different recurrence pattern after neoadjuvant chemoradiotherapy compared to surgery alone in esophageal cancer patients. Ann Surg Oncol. 2013;20:4008–15.
Meguid RA, Hooker CM, Taylor JT, et al. Recurrence after neoadjuvant chemoradiation and surgery for esophageal cancer: does the pattern of recurrence differ for patients with complete response and those with partial or no response?. J Thorac Cardiovasc Surg. 2009;138:1309–17.
Chao YK, Chan SC, Liu YH, et al. Pretreatment T3–4 stage in an adverse prognostic factor in patients with esophageal squamous cell carcinoma who achieve pathological complete response following preoperative chemoradiotherapy. Ann Surg. 2009;249:392–6.
Zanoni A, Verlato G, Giacopuzzi S, et al. Neoadjuvant concurrent chemoradiotherapy for locally advanced esophageal cancer in a single high-volume center. Ann Surg Oncol. 2013;20:1993–9.
Oppedijk V, van der Gaast A, van Lanschot JJB, et al. Patterns of recurrence after surgery alone versus preoperative chemoradiotherapy and surgery in the CROSS trials. J Clin Oncol. 2014;32:385–91.
Speicher PJ, Englum BR, Ganapathi AM, et al. Adjuvant chemotherapy is associated with improved survival after esophagectomy without induction therapy for node-positive adenocarcinoma. J Thorac Oncol. 2015;10:181–8.
Lagarde SM, de Boer JD, ten Kate FJ, et al. Postoperative complications after esophagectomy for adenocarcinoma of the esophagus are related to timing of death due to recurrence. Ann Surg. 2008;247:71–6.
Lerut T, Moons J, Coosemans W, et al. Postoperative complications after transthoracic esophagectomy for cancer of the esophagus and gastroesophageal junction are correlated with early cancer recurrence. Ann Surg. 2009;250:798–807.
Luc G, Durand M, Chiche L, et al. Major post-operative complications predict long-term survival after esophagectomy in patients with adenocarcinoma of the esophagus. World J Surg. 2015;39:216–22.
Miyata H, Yamasaki M, Kurokawa Y, et al. Prognostic value of an inflammation-based score in patients undergoing pre-operative chemotherapy followed by surgery for esophageal cancer. Exp Ther Med. 2011;2:879–85.
Balkwill F, Mantovani A. Inflammation and cancer: back to Virchow?. Lancet. 2001;357:539–45.
Mantovani A, Allavena P, Sica A, et al. Cancer-related inflammation. Nature. 2008;454:436–44.
Mandard AM, Dalibard F, Mandard JC, et al. Pathologic assessment of tumor regression after preoperative chemoradiotherapy of esophageal carcinoma: clinicopathologic correlations. Cancer. 1994;73:2680–6.
Disclosure
None declared.
Author information
Authors and Affiliations
Corresponding author
Additional information
On behalf of the FREGAT (French Eso-Gastric Tumors) working group—FRENCH (Fédération de Recherche EN CHirurgie)—AFC (Association Française de Chirurgie). The members of the FREGAT (French Eso-Gastric Tumors) working group, FRENCH (Fédération de Recherche EN CHirurgie) and AFC (Association Française de Chirurgie) are given in Appendix.
Appendix
Appendix
The members of the FREGAT (French Eso-Gastric Tumors) working group, FRENCH (Fédération de Recherche EN CHirurgie) and AFC (Association Française de Chirurgie) are given below.
Abdennahceur Dhahri, MD, PhD, Delphine Lignier, MD, Cyril Cossé, MD, Jean-Marc Regimbeau, MD, PhD, Department of Digestive Surgery Amiens, France; Magalie Cabau, MD, Department of Digestive Surgery Bordeaux, France; Jacques Jougon MD, PhD, Department of Thoracic Surgery Bordeaux, France; Bogdan Badic, MD, Patrick Lozach, MD, Jean Pierre Bail, MD, Department of Digestive Surgery, Brest, France; Serge Cappeliez, MD, PhD, Issam El Nakadi, MD, PhD, Department of Digestive Surgery, Brussel ULB Erasme Bordet University, Brussel, Belgium; Gil Lebreton, MD, Arnaud Alves, MD, PhD, Department of Digestive Surgery, Caen, France; Renaud Flamein, MD, Denis Pezet, MD, PhD, Department of Digestive Surgery, Clermont-Ferrand, France; Federica Pipitone, MD, Bogdan Stan-Iuga, MD, Nicolas Contival, MD, Eric Pappalardo, MD, Simon Msika, MD, PhD, Department of Digestive Surgery, Louis Mourier University Hospital, Colombes, France; Styliani Mantziari, MD, Nicolas Demartines, Department of Digestive Surgery, Lausanne University Hospital, Lausanne, Switzerland; Flora Hec, MD, Marguerite Vanderbeken, MD, Williams Tessier, MD, Nicolas Briez, MD, Department of Digestive Surgery, Lille, France; Fabien Fredon, MD, Alain Gainant, MD, Muriel Mathonnet, MD, PhD, Department of Digestive Surgery, Limoges, France; Salim Mezoughi, MD, Christian Ducerf, MD, Jacques Baulieux, MD, Jean-Yves Mabrut, MD, PhD, Department of Digestive Surgery, Croix Rousse University Hospital, Lyon, France; Arnaud Pasquer, MD, Oussama Baraket, MD, Gilles Poncet, MD, Mustapha Adam, MD, PhD, Department of Digestive Surgery, Edouard Herriot University Hospital, Lyon, France; Delphine Vaudoyer, MD, Peggy Jourdan Enfer, MD, Laurent Villeneuve, MD, Olivier Glehen, MD, PhD, Department of Digestive Surgery, Lyon Sud University Hospital, Lyon, France; Thibault Coste, MD, Jean-Michel Fabre, MD, Department of Digestive Surgery, Montpellier, France; Frédéric Marchal, MD, Department of Digestive Surgery, Institut de cancérologie de Lorraine, Nancy, France; Romain Frisoni, MD, Ahmet Ayav, MD, PhD, Laurent Brunaud, MD, PhD, Laurent Bresler, MD, Department of Digestive Surgery, Nancy, France; Charlotte Cohen, MD, Olivier Aze, MD, Nicolas Venissac, MD, Daniel Pop, MD, Jérôme Mouroux, MD, Department of Thoracic Surgery, Nice, France; Ion Donici, MD, Michel Prudhomme, MD, PhD, Department of Digestive Surgery, Nîmes, France; Emanuele Felli, MD, Stéphanie Lisunfui, MD, Marie Seman, MD, Gaelle Godiris Petit, MD, Mehdi Karoui, MD, PhD, Christophe Tresallet, MD, PhD, Fabrice Ménégaux, MD, PhD, Jean-Christophe Vaillant, MD, Laurent Hannoun, MD, Department of Digestive Surgery, Pitié-Salpétrière University Hospital, Paris, France; Brice Malgras, MD, Denis Lantuas, MD, Karine Pautrat, MD, Marc Pocard, MD, PhD, Patrice Valleur, MD, Department of Digestive Surgery, Lariboisière University Hospital, Paris, France; Najim Chafai, MD, Pierre Balladur, MD, Magalie Lefrançois, MD, Yann Parc, MD, PhD, François Paye, MD, PhD Emmanuel Tiret, MD Department of Digestive Surgery, Saint-Antoine University Hospital, Paris, France; Marius Nedelcu, MD, Letizia Laface, MD, Thierry Perniceni, MD, Brice Gayet, MD, Department of Digestive Surgery, Institut Mutualiste Montsouris, Paris, France; Bernard Meunier, MD, Department of Digestive Surgery, Rennes, France; Alexandre Filipello, MD, Jack Porcheron, MD, Olivier Tiffet, MD, PhD, Department of Digestive Surgery, Saint-Etienne, France; Noémie Kamlet, MD, Rodrigue Chemaly, MD, Amandine Klipfel, MD, Patrick Pessaux, MD, PhD, Cecile Brigand, MD, PhD, Serge Rohr MD, Department of Digestive Surgery, Strasbourg, France; Nicolas Carrère, MD, PhD, Department of Digestive Surgery, Toulouse, France; Chiara Da Re, MD, Frédéric Dumont, MD, Diane Goéré, MD, PhD, Dominique Elias, MD, Department of Digestive Surgery Institut Gustave-Roussy,Villejuif, France; Claude Bertrand, MD, Mont-Godinne University Hospital, Yvoir, Belgium.
Rights and permissions
About this article
Cite this article
Luc, G., Gronnier, C., Lebreton, G. et al. Predictive Factors of Recurrence in Patients with Pathological Complete Response After Esophagectomy Following Neoadjuvant Chemoradiotherapy for Esophageal Cancer: A Multicenter Study. Ann Surg Oncol 22 (Suppl 3), 1357–1364 (2015). https://doi.org/10.1245/s10434-015-4619-8
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-015-4619-8