Abstract
Background
Major pathologic response (MPR) following neoadjuvant therapy (NAT) in pancreatic ductal adenocarcinoma (PDAC) patients undergoing resection is associated with improved survival. We sought to determine whether racial disparities exist in MPR rates following NAT in patients with PDAC undergoing resection.
Methods
Patients with potentially operable PDAC receiving at least 2 cycles of neoadjuvant FOLFIRINOX or gemcitabine/nab-paclitaxel ± radiation followed by pancreatectomy (2010-2019) at 7 high-volume centers were reviewed. Self-reported race was dichotomized as Black and non-Black, and multivariable models evaluated the association between race and MPR (i.e., pathologic complete response [pCR] or near-pCR). Cox regression evaluated the association between race and disease-free (DFS) and overall survival (OS).
Results
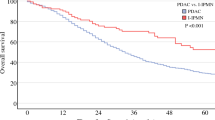
Results of 486 patients who underwent resection following NAT (mFOLFIRINOX 56%, gemcitabine/nab-paclitaxel 25%, radiation 29%), 67 (13.8%) patients were Black. Black patients had lower CA19-9 at diagnosis (median 67 vs. 204 U/mL; P = 0.003) and were more likely to undergo mild/moderate chemotherapy dose modification (40 vs. 20%; P = 0.005) versus non-Black patients. Black patients had significantly lower rates of MPR compared with non-Black patients (13.4 vs. 25.8%; P = 0.039). Black race was independently associated with worse MPR (OR 0.26, 95% confidence interval [CI] 0.10-0.69) while controlling for NAT duration, CA19-9 dynamics, and chemotherapy modifications. There was no significant difference in DFS or OS between Black and non-Black cohorts.
Conclusions
Black patients undergoing pancreatectomy appear less likely to experience MPR following NAT. The contribution of biologic and nonbiologic factors to reduced chemosensitivity in Black patients warrants further investigation.


Similar content being viewed by others
References
Rahib L, Smith BD, Aizenberg R, Rosenzweig AB, Fleshman JM, Matrisian LM. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 2014;74(11):2913–21.
Tesfaye AA, Philip PA. Adjuvant treatment of surgically resectable pancreatic ductal adenocarcinoma. Clin Adv Hematol Oncol. 2019;17(1):54–63.
Truty MJ, Kendrick ML, Nagorney DM, et al. Factors predicting response, perioperative outcomes, and survival following total neoadjuvant therapy for borderline/locally advanced pancreatic cancer. Ann Surg. 2021;273(2):341–9.
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7–33.
Vega EA, Kutlu OC, Salehi O, et al. Preoperative chemotherapy for pancreatic cancer improves survival and R0 rate even in early stage I. J Gastrointest Surg. 2020;24(10):2409–15.
Jang JY, Han Y, Lee H, et al. Oncological benefits of neoadjuvant chemoradiation with gemcitabine versus upfront surgery in patients with borderline resectable pancreatic cancer: a prospective, randomized, open-label, multicenter Phase 2/3 trial. Ann Surg. 2018;268(2):215–22.
Pecorelli N, Licinio AW, Guarneri G, et al. Prognosis of upfront surgery for pancreatic cancer: a systematic review and meta-analysis of prospective studies. Front Oncol. 2021;11:812102.
Singh RR, O’Reilly EM. New treatment strategies for metastatic pancreatic ductal adenocarcinoma. Drugs. 2020;80(7):647–69.
Lei F, Xi X, Batra SK, Bronich TK. Combination therapies and drug delivery platforms in combating pancreatic cancer. J Pharmacol Exp Ther. 2019;370(3):682–94.
Bilimoria KY, Bentrem DJ, Ko CY, et al. Multimodality therapy for pancreatic cancer in the U.S.: utilization, outcomes, and the effect of hospital volume. Cancer. 2007;110(6):1227–34.
Roland CL, Yang AD, Katz MH, et al. Neoadjuvant therapy is associated with a reduced lymph node ratio in patients with potentially resectable pancreatic cancer. Ann Surg Oncol. 2015;22(4):1168–75.
Taboada AGM, Lominchar PL, Roman LM, et al. Advances in neoadjuvant therapy for resectable pancreatic cancer over the past two decades. Ann Hepatobiliary Pancreat Surg. 2021;25(2):179–91.
Chawla A, Ferrone CR. Neoadjuvant therapy for resectable pancreatic cancer: an evolving paradigm shift. Front Oncol. 2019;9:1085.
Sohal DP, Walsh RM, Ramanathan RK, Khorana AA. Pancreatic adenocarcinoma: treating a systemic disease with systemic therapy. J Natl Cancer Inst. 2014;106(3):dju011.
Blinn P, Shridhar R, Maramara T, Huston J, Meredith K. Multi-agent neoadjuvant chemotherapy improves response and survival in patients with resectable pancreatic cancer. J Gastrointest Oncol. 2020;11(5):1078–89.
He J, Blair AB, Groot VP, et al. Is a pathological complete response following neoadjuvant chemoradiation associated with prolonged survival in patients with pancreatic cancer? Ann Surg. 2018;268(1):1–8.
Bolton NM, Maerz AH, Brown RE, Bansal M, Bolton JS, Conway WC. Multiagent neoadjuvant chemotherapy and tumor response are associated with improved survival in pancreatic cancer. HPB (Oxford). 2019;21(4):413–8.
Macedo FI, Ryon E, Maithel SK, et al. Survival outcomes associated with clinical and pathological response following neoadjuvant FOLFIRINOX or gemcitabine/nab-paclitaxel chemotherapy in resected pancreatic cancer. Ann Surg. 2019;270(3):400–13.
Khawja SN, Mohammed S, Silberfein EJ, Musher BL, Fisher WE, Van Buren G 2nd. Pancreatic cancer disparities in African Americans. Pancreas. 2015;44(4):522-7.
Tavakkoli A, Singal AG, Waljee AK, et al. Racial disparities and trends in pancreatic cancer incidence and mortality in the United States. Clin Gastroenterol Hepatol. 2020;18(1):171-178.e110.
Wray CJ, Castro-Echeverry E, Silberfein EJ, Ko TC, Kao LS. A multi-institutional study of pancreatic cancer in Harris County, Texas: race predicts treatment and survival. Ann Surg Oncol. 2012;19(9):2776–81.
Heller DR, Nicolson NG, Ahuja N, Khan S, Kunstman JW. Association of treatment inequity and ancestry with pancreatic ductal adenocarcinoma survival. JAMA Surg. 2020;155(2):e195047.
Singal V, Singal AK, Kuo YF. Racial disparities in treatment for pancreatic cancer and impact on survival: a population-based analysis. J Cancer Res Clin Oncol. 2012;138(4):715–22.
Lutfi W, Zenati MS, Zureikat AH, Zeh HJ, Hogg ME. Health disparities impact expected treatment of pancreatic ductal adenocarcinoma nationally. Ann Surg Oncol. 2018;25(7):1860–7.
Scarton L, Yoon S, Oh S, et al. Pancreatic cancer-related health disparities: A commentary. Cancers (Basel). 2018;10(7):235.
Singh GK, Jemal A. Socioeconomic and racial/ethnic disparities in cancer mortality, incidence, and survival in the United States, 1950–2014: over six decades of changing patterns and widening inequalities. J Environ Public Health. 2017;2017:2819372.
Shavers VL, Harlan LC, Jackson M, Robinson J. Racial/ethnic patterns of care for pancreatic cancer. J Palliat Med. 2009;12(7):623–30.
Brotherton L, Welton M, Robb SW. Racial disparities of pancreatic cancer in Georgia: a county-wide comparison of incidence and mortality across the state, 2000–2011. Cancer Med. 2016;5(1):100–10.
Lutfi W, Hogg ME. ASO Author reflections: health disparities in pancreatic cancer. Ann Surg Oncol. 2018;25(Suppl 3):824–5.
von Elm E, Altman DG, Egger M, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335(7624):806–8.
Vauthey JN, Dixon E. AHPBA/SSO/SSAT consensus conference on resectable and borderline resectable pancreatic cancer: rationale and overview of the conference. Ann Surg Oncol. 2009;16(7):1725–6.
Compton CC, Henson DE. Protocol for the examination of specimens removed from patients with carcinoma of the exocrine pancreas: a basis for checklists. Cancer Committee, College of American Pathologists. Arch Pathol Lab Med. 1997;121(11):1129–36.
Oba A, Ho F, Bao QR, Al-Musawi MH, Schulick RD, Del Chiaro M. Neoadjuvant treatment in pancreatic cancer. Front Oncol. 2020;10:245.
Bandera EV, Lee VS, Rodriguez-Rodriguez L, Powell CB, Kushi LH. Racial/ethnic disparities in ovarian cancer treatment and survival. Clin Cancer Res. 2016;22(23):5909–14.
Boone BA, Steve J, Zenati MS, et al. Serum CA 19–9 response to neoadjuvant therapy is associated with outcome in pancreatic adenocarcinoma. Ann Surg Oncol. 2014;21(13):4351–8.
Ahmad SA, Duong M, Sohal DPS, et al. Surgical outcome results from SWOG S1505: A randomized clinical trial of mFOLFIRINOX versus gemcitabine/nab-paclitaxel for perioperative treatment of resectable pancreatic ductal adenocarcinoma. Ann Surg. 2020;272(3):481–6.
Funding
National Cancer Institute (NCI), Nipun B. Merchant T32CA211034, National Institutes of Health (NIH), Jashodeep Datta UL1TR002736
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ogobuiro, I., Collier, A.L., Khan, K. et al. Racial Disparity in Pathologic Response following Neoadjuvant Chemotherapy in Resected Pancreatic Cancer: A Multi-Institutional Analysis from the Central Pancreatic Consortium. Ann Surg Oncol 30, 1485–1494 (2023). https://doi.org/10.1245/s10434-022-12741-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-022-12741-4