Abstract
Background
This study aimed to assess whether surgical case volume for lateral neck dissection has an impact on the survival of patients who have well-differentiated thyroid cancer (WDTC) with lateral cervical node metastases. The authors used a population-based cohort study design.
Methods
The study cohort consisted of WDTC patients in Ontario Canada who underwent thyroidectomy and lateral neck dissection. These patients were identified using both hospital- and surgeon-level administrative data between 1993 and 2017 (n = 1832). Surgeon and hospital volumes were calculated based on the number of cases managed in the year before the procedure by the physician and at the institution managing each case, respectively, and divided into tertiles. Multilevel Cox regression models were used to estimate the effect of volume on disease-free survival (DFS).
Results
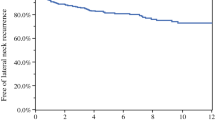
A crude model without patient or treatment characteristics demonstrated that DFS was associated with both higher surgeon volume tertiles (p < 0.01) and higher hospital volume tertiles (p < 0.01). After control for clustering, patient/treatment covariates, and hospital volume, the lowest surgeon volume tertile (range, 0–20/year; mean, 6.5/year) remained an independent statistically significant negative predictor of DFS (hazard ratio, 1.71; 95 % confidence interval, 1.22–2.4; p < 0.01).
Conclusion
Surgeon lateral neck dissection case volume is a predictor of better DFS for thyroid cancer patients, with the lowest surgeon volume tertile (<20 neck dissections per year) demonstrating poorer DFS.



Similar content being viewed by others
References
Bongers PJ, Verzijl R, Dzingala M, Vriens MR, Yu E, Pasternak JDRL. Preoperative computed tomography changes surgical management for clinically low-risk well-differentiated thyroid cancer. Ann Surg Oncol. 2019;26:4439–44.
Davies LWH. Increasing incidence of thyroid cancer in the United States, 1973–2002. JAMA. 2006;295:2164–7.
Stack BC, Ferris RL, Goldenberg D, et al. American Thyroid Association Consensus review and statement regarding the anatomy, terminology, and rationale for lateral neck dissection in differentiated thyroid cancer. Thyroid. 2012;22:5.
Eskander A, Merdad M, Irish JC, Hall SF, Groome PA, Freeman JL, Urbach DRGD. Volume–outcome associations in head and neck cancer treatment: a systematic review and meta-analysis Antoine. Head Neck. 2009;1188–1195.
Meltzer CJ, Irish J, Angelos P, et al. American Head and Neck Society Endocrine Section clinical consensus statement: North American quality statements and evidence-based multidisciplinary workflow algorithms for the evaluation and management of thyroid nodules. Head Neck. 2019;843–56.
Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016;26:1–133.
McMullen C, Rocke D, Freeman J. Complications of bilateral neck dissection in thyroid cancer from a single high-volume center. JAMA Otolaryngol Head Neck Surg. 2017;143:376–81.
Roh JL, Kim DHPC. Prospective identification of chyle leakage in patients undergoing lateral neck dissection for metastatic thyroid cancer. Ann Surg Oncol. 2008;15:424–9.
Shaha A. Complications of neck dissection for thyroid cancer. Ann Surg Oncol. 2008;15:397–9.
Pieracci FM, Fahey TJ. Effect of hospital volume of thyroidectomies on outcomes following substernal thyroidectomy. World J Surg. 2008;32:740–6.
Adam MA, Thomas S, Youngwirth L, et al. Is there a minimum number of thyroidectomies a surgeon should perform to optimize patient outcomes? Ann Surg. 2017;265:402–7.
Youngwirth LM, Adam MA, Scheri RP, Roman SA, Sosa JA. Patients treated at low-volume centers have higher rates of incomplete resection and compromised outcomes: analysis of 31,129 patients with papillary thyroid cancer. Ann Surg Oncol. 2016;23:403–9.
Youngwirth LM, Adam MA, Thomas SM, Roman SA, Sosa JA, Scheri RP. Pediatric thyroid cancer patients referred to high-volume facilities have improved short-term outcomes. Surgery. 2018;163:361–6.
Eskander A, Monteiro E, Irish J, Gullane P, Gilbert R, de Almeida J, et al. Adherence to guideline-recommended process measures for squamous cell carcinoma of the head and neck in Ontario: impact of surgeon and hospital volume. Head Neck. 2016;38(Suppl 1):E1987–92.
Eskander A, Irish J, Groome P, Freeman J, Gullane P, Gilbert R, et al. Volume-outcome relationships for head and neck cancer surgery in a universal health care system. Laryngoscope. 2014;124:2081–8.
Eskander A, Irish J, Groome PA, et al. Volume-outcome relationships for head and neck cancer surgery in a universal health care system. Laryngoscope. 2014;124:2081–8.
Gourin C, Tufano RF, et al. Volume-based trends in thyroid surgery. JAMA Otolaryngol Head Neck Surg. 2010;136:1191–8.
Kulkarni GS, Laupacis A, Urbach DR, Fleshner NEAP. Varied definitions of hospital volume did not alter the conclusions of volume-outcome analyses. J Clin Epidemiol. 2009;62:400–7.
Hall SF, Irish J, Groome P, Griffiths R, Hurlbut D. Do lower-risk thyroid cancer patients who live in regions with more aggressive treatments have better outcomes? Thyroid. 2017;27:1246–57.
Eskander A, Hall SF, Manduch M, Griffiths R, Irish J. A population-based study on NIFTP incidence and survival: is NIFTP really a “benign” disease? Ann Surg Oncol. 2019;26:1376–84.
Jonathan W. The Johns Hopkins ACG Case-Mix System Version 6.0 Release Notes. Johns Hopkins Univ Bloom Sch Public Heal Heal Serv Res Dev Center.
Austin PC, Van Walraven C, Wodchis WP. Using the Johns Hopkins aggregated diagnosis groups (ADGs) to predict mortality in a general adult population cohort in general adult population cohort in Ontario, Canada. Med Care. 2015;49:932–9.
Durbin A, Moineddin R, Lin E, et al. Examining the relationship between neighbourhood deprivation and mental health service use of immigrants in Ontario, Canada: a cross-sectional study. BMJ Open. 2015;5:e006690.
Austin P. A tutorial on multilevel survival analysis: methods, models, and applications. Int Stat Rev. 2017;85:185–203.
Zhang X, Loberiza FR, Klein JP, Zhang MJ. A SAS macro for estimation of direct adjusted survival curves based on a stratified Cox regression model. Comput Methods Programs Biomed. 2007;88:95–111.
Gail MH, Byar DP. Variance calculations for direct adjusted survival curves, with applications to testing for no treatment effect. Biometrical J. 1986;28:587–99.
Makuch RW. Adjusted survival curve estimation using covariates. J Chronic Dis. 1982;35:437–43.
Desquilbet L, Mariotti F. Dose-response analyses using restricted cubic spline functions in public health research. Stat Med. 2010;29:1037–57.
Birkmeyer JD, Stukel TA, Siewers AE, Goodney PP, Wennberg DELF. Surgeon volume and operative mortality in the United States. N Engl J Med. 2003;349:2117–27.
Chereau N, Buffet C, Tresallet C, Tissier F, Leenhardt L, Menegaux F. Recurrence of papillary thyroid carcinoma with lateral cervical node metastases: predictive factors and operative management. Surgery. 2016;159:755–62.
Nunes JHV, Clark JR, Gao K, et al. Prognostic implications of lymph node yield and lymph node ratio in papillary thyroid carcinoma. Thyroid. 2013;23:7.
Heaton C, Chang J, Orloff L. Prognostic implications of lymph node yield in central and lateral neck dissections for well-differentiated papillary thyroid carcinoma. Thyroid. 2016;26:434–40.
Zengaa J, Divib V, Stadlera M, et al. Lymph node yield, depth of invasion, and survival in node-negative oral cavity cancer. Oral Oncol. 2019;98:125–31.
Lemieux A, Kedarisetty S, Raju S, Orosco RCC. Lymph node yield as a predictor of survival in pathologically node-negative oral cavity carcinoma. Otolaryngol Head Neck Surg. 2016;154:465–72.
Yip L. Association of number of dissected lymph nodes with survival in clinically node-negative oral cavity squamous cell carcinoma patients undergoing primary surgery: a population-based analysis. JAMA Otolaryngol Head Neck Surg. 2017;143:1049–52.
Divi V, et al. Lymph node count from neck dissection predicts mortality in head and neck cancer. J Clin Oncol. 2016;34:3892–7.
White MG, Applewhite MK, Kaplan EL. A tale of two cancers: traveling to treat pancreatic and thyroid cancer. J Am Coll Surg. 2017;225:125–36.
Gourin CG, Forastiere AA, Sanguineti G, Marur S, Koch WMBR. Volume-based trends in laryngeal cancer surgery. Laryngoscope. 2011;121:77–84.
Gourin CG, Forastiere AA, Sanguineti G, Marur S, Koch WMBR. Volume-based trends in surgical care of patients with oropharyngeal cancer. Laryngoscope. 2011;121:738–45.
Eskander A, Irish JC, Groome P, Urbach DRGD. Head and neck cancer in Ontario: ICES research atlas. In press.
Bendzsak AM, Baxter NN, Darling GE, Austin PCUD. Regionalization and outcomes of lung cancer surgery in Ontario, Canada. J Clin Oncol. 2017;35(24):2772–80.
Simunovic M, Urbach D, Major D, Sutradhar R, Baxter N, To T, Brown A, Davis DLM. Assessing the volume-outcome hypothesis and region-level quality improvement interventions: pancreas cancer surgery in two Canadian provinces. Ann Surg Oncol. 2010;10:2537–44.
Acknowledgments
This study was supported by the ICES, which is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care (MOHLTC). The opinions, results, and conclusions reported in this article are those of the authors and are independent from the funding sources. Parts of this material are based on data and information provided by CCO and the Canadian Institute for Health Information (CIHI). We thank Immigration, Refugees and Citizenship Canada (IRCC) for providing access to the database used in this study. We also thank Service Ontario for the use of the Office of the Registrar General for information on deaths. The analyses, conclusions, opinions, and statements reported in this article are those of the authors and do not necessarily reflect those of CCO or CIHI. No endorsement by the ICES or the MOHLTC or CCO or CIHI is intended or should be inferred. We acknowledge Dr. Jiming Fang at ICES Central for assisting in statistical design.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Dr. Eskander received research funds from Merck and was a paid consultant for Bristol-Myers. Dr. Noel receives salary support through a CIHR Doctoral Award, an Ontario Ministry of Health Clinician Investigator Award, an Ontario Graduate Scholarship, the Chapnik Freeman Friedberg Clinician Scientist Award, the Raymond H.W. Ng PhD Scholarship, and the Waratah Hold’em for Life Oncology Fellowship. Dr. Eskander also is supported by a Terry Fox Research Institute New Investigator Grant. Dr. Siu receives support through the Chapnik Freeman Friedberg Clinician Scientist Award. Dr. Austin is supported by a Mid-Career Investigator Award from the Heart and Stroke Foundation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Siu, J., Griffiths, R., Noel, C.W. et al. Surgical Case Volume has an Impact on Outcomes for Patients with Lateral Neck Disease in Thyroid Cancer. Ann Surg Oncol 29, 1141–1150 (2022). https://doi.org/10.1245/s10434-021-10923-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-021-10923-0