Abstract
Background
Extracapsular spread (ECS) is recognized to be a high-risk factor in melanoma patients with macrometastatic (N+) nodal disease; however, ECS risk in sentinel lymph node (SLN) biopsy, micrometastatic stage III disease is ambiguous.
Objective
The aim of this study was to examine ECS incidence and its prognostic significance.
Methods
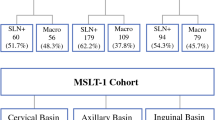
A two-center, retrospective analysis of all patients with micro/macrometastatic lymphadenopathy undergoing nodal surgery from 2008 to 2014 was performed. Patient demographics, tumor characteristics, nodal ECS status, and patient outcomes were collected.
Results
Overall, 515 patients with nodal disease were identified (males/females = 277/238); median age was 63 years (range 17–94). There was an increased frequency of ECS disease in N+ disease compared with SLN+ disease (52.4% vs. 16.2%; p < 0.0001). The absolute disease-specific survival (DSS) difference for SLN+ patients was approximately 30% at 10 years (66.2% vs. 37.2%; p < 0.0001), and the prognosis of SLN+/ECS+ patients was identical to N+/ECS− patients. Multivariate analysis demonstrated that ECS status was an independent prognostic indicator for DSS (hazard ratio 2.47, 95% confidence interval 1.87–3.26; p < 0.0001) in patients with SLN+ disease. There were significant differences in nodal burden according to ECS status between the SLN+ and N+ subgroups suggestive of differing biology in ECS+ tumors.
Conclusion
We found that ECS is a significant DSS, progression-free survival, and overall survival indicator in SLN+ and N+ disease. We demonstrated that ECS upstages stage III disease, similar to ulceration in primary melanoma (stage I/II disease). A simplified staging system substituting ECS for N stage accurately stages patients according to prognosis.


Similar content being viewed by others
References
Gershenwald JE, Scolyer RA. Melanoma staging: American joint committee on cancer (AJCC) 8th edition and beyond. Ann Surg Oncol. 2018;25(8):2105–10.
Clark JR, Shaw D. Extracapsular spread. In: Kountakis SE (ed). Encyclopedia of otolaryngology, head and neck surgery. Berlin: Springer; 2013, pp. 851–852. https://doi.org/10.1007/978-3-642-23499-6_200162.
Henderson MA, Burmeister BH, Ainslie J, et al. Adjuvant lymph-node field radiotherapy versus observation only in patients with melanoma at high risk of further lymph-node field relapse after lymphadenectomy (ANZMTG 01.02/TROG 02.01): 6-year follow-up of a phase 3, randomised controlled trial. Lancet Oncol. 2015;16(9):1049–60.
Agrawal S, Kane JM 3rd, Guadagnolo BA, Kraybill WG, Ballo MT. The benefits of adjuvant radiation therapy after therapeutic lymphadenectomy for clinically advanced, high-risk, lymph node-metastatic melanoma. Cancer. 2009;115(24):5836–44.
Lee RJ, Gibbs JF, Proulx GM, Kollmorgen DR, Jia C, Kraybill WG. Nodal basin recurrence following lymph node dissection for melanoma: implications for adjuvant radiotherapy. Int J Radiat Oncol Biol Phys. 2000;46(2):467–74.
Dewar DJ, Newell B, Green MA, Topping AP, Powell BWEM, Cook MG. The microanatomic location of metastatic melanoma in sentinel lymph nodes predicts nonsentinel lymph node involvement. J Clin Oncol. 2004;22(16):3345–9.
Starz H, Balda BR, Krämer KU, Büchels H, Wang H. A micromorphometry-based concept for routine classification of sentinel lymph node metastases and its clinical relevance for patients with melanoma. Cancer. 2001;91(11):2110–21.
van Akkooi ACJ, de Wilt JHW, Verhoef C, et al. Clinical relevance of melanoma micrometastases (< 0.1 mm) in sentinel nodes: are these nodes to be considered negative? Ann Oncol. 2006;17(10):1578–85. https://doi.org/10.1093/annonc/mdl176.
Faries MB, Thompson JF, Cochran AJ, et al. Completion dissection or observation for sentinel-node metastasis in melanoma. N Engl J Med. 2017;376(23):2211–22.
Leiter U, Stadler R, Mauch C, et al. Complete lymph node dissection versus no dissection in patients with sentinel lymph node biopsy positive melanoma (DeCOG-SLT): a multicentre, randomised, phase 3 trial. Lancet Oncol. 2016;17(6):757–67.
Melanoma: assessment and management. Guidance and guidelines. NICE. https://www.nice.org.uk/guidance/ng14. Accessed 22 Nov 2018.
Coit DG, Thompson JA, Albertini MR, et al. Cutaneous melanoma, version 2.2019, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2019;17(4):367–402.
U.S. Department of Health and Human Services: Food and Drug Administration. Clinical Trial Endpoints for the Approval of Cancer Drugs and Biologics. FDA.gov. https://www.fda.gov/media/71195/download. Published December 2108. Accessed 13 Jun 2020.
Gershenwald JE, Scolyer RA, Hess KR, et al. Melanoma staging: evidence-based changes in the American Joint Committee on Cancer eighth edition cancer staging manual. CA Cancer J Clin. 2017;67(6):472–92.
Debarbieux S, Duru G, Dalle S, Béatrix O, Balme B, Thomas L. Sentinel lymph node biopsy in melanoma: a micromorphometric study relating to prognosis and completion lymph node dissection. Br J Dermatol. 2007;157(1):58–67. https://doi.org/10.1111/j.1365-2133.2007.07937.x.
Sabel MS, Griffith K, Sondak VK, et al. Predictors of nonsentinel lymph node positivity in patients with a positive sentinel node for melanoma. J Am Coll Surg. 2005;201(1):37–47.
Moncrieff MD, Martin R, O’Brien CJ, et al. Adjuvant postoperative radiotherapy to the cervical lymph nodes in cutaneous melanoma: is there any benefit for high-risk patients? Ann Surg Oncol. 2008;15(11):3022–7.
Morton DL, Thompson JF, Cochran AJ, et al. Final trial report of sentinel-node biopsy versus nodal observation in melanoma. N Engl J Med. 2014;370(7):599–609.
Rao UNM, Ibrahim J, Flaherty LE, Richards J, Kirkwood JM. Implications of microscopic satellites of the primary and extracapsular lymph node spread in patients with high-risk melanoma: pathologic corollary of eastern cooperative oncology group trial E1690. J Clin Oncol. 2002;20(8):2053–7. https://doi.org/10.1200/jco.2002.08.024.
Calabro A, Singletary SE, Balch CM. Patterns of relapse in 1001 consecutive patients with melanoma nodal metastases. Arch Surg. 1989;124(9):1051–5.
Coit D. The enigma of regional lymph nodes in melanoma. N Engl J Med. 2017;376(23):2280–1.
Balch CM, Soong S-J, Gershenwald JE, et al. Prognostic factors analysis of 17,600 melanoma patients: validation of the American Joint Committee on Cancer melanoma staging system. J Clin Oncol. 2001;19(16):3622–34.
Thorsson V, Gibbs DL, Brown SD, et al. The immune landscape of cancer. Immunity. 2018;48(4):812–30.e14.
Chen DS, Mellman I. Elements of cancer immunity and the cancer-immune set point. Nature. 2017;541(7637):321–30.
Teng MWL, Ngiow SF, Ribas A, Smyth MJ. Classifying cancers based on T-cell infiltration and PD-L1. Cancer Res. 2015;75(11):2139–45.
Funding
Ryckie Wade is a Doctoral Research Fellow funded by the National Institute for Health Research (NIHR; DRF-2018-11-ST2-028). The views expressed in this article are those of the authors and not necessarily those of the UK National Health Service, NIHR, or Department of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lo, M., Robinson, A., Wade, R. et al. Extracapsular Spread in Melanoma Lymphadenopathy: Prognostic Implications, Classification, and Management. Ann Surg Oncol 28, 1642–1653 (2021). https://doi.org/10.1245/s10434-020-09099-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-020-09099-w