Abstract
Background
The accuracy of sentinel lymph node dissection (SLND) in clinically node-positive patients who receive neoadjuvant chemotherapy has been investigated in clinical trials. This survey was designed to assess familiarity and impact of these trial findings into practice.
Methods
American Society of Breast Surgeons members were invited by e-mail to complete an anonymous online survey. A total of 642 members responded (21% of 3090 eligible members). Results were summarized as proportions based on the number of responses to each question.
Results
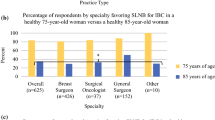
Respondents indicated knowledge of the Z1071 (86%), SENTINA (57%), and SN-FNAC (39%) trials. The published false negative rates (FNR) of the trials were correctly reported by 53% (336/638) of respondents. Before the trials, 45% (285/636) offered SLND compared with 85% (543/638) after the trials. In the 556 respondents who reported knowledge of at least one trial, 310 (56%) currently offer SLND to >50% of patients, 175 (31%) offer to <50%, and 70 (13%) routinely perform axillary lymph node dissection. Respondents who reported knowledge of the trials but did not change their practice to incorporate SLND (n = 67) cited concerns over lack of outcome data (64%), worries about FNR (42%), lack of resources (34%), or objections from radiation oncologists (25%), medical oncologists (18%), or other surgeons (8%).
Conclusions
The publication of trials evaluating SLND in clinically node-positive patients has resulted in changes in practice. Concerns over the FNR and lack of outcome data limit incorporation of SLND into practice by some surgeons.


Similar content being viewed by others
References
Boughey J, McCall L, Ballman K, et al. Tumor biology correlates with rates of breast-conserving surgery and pathologic complete response after neoadjuvant chemotherapy for breast cancer: findings from the ACOSOG Z1071 (Alliance) Prospective Multicenter Clinical Trial. Ann Surg. 2014;260(4):608–14.
Kuerer H, Sahin A, Hunt K, et al. Incidence and impact of documented eradication of breast cancer axillary lymph node metastases before surgery in patients treated with neoadjuvant chemotherapy. Ann Surg. 1999;230(1):72–8.
Buzdar A, Ibrahim N, Francis D, et al. Significantly higher pathologic complete remission rate after neoadjuvant therapy with trastuzumab, paclitaxel, and epirubicin chemotherapy: results of a randomized trial in human epidermal growth factor receptor 2-positive operable breast cancer. J Clin Oncol. 2005;23(16):3676–84.
Dominici L, Mittendorf E, Wang X, et al. Implications of constructed biologic subtype and its relationship to locoregional recurrence following mastectomy. Breast Cancer Res. 2012;14(3):R82.
Hennessy B, Hortobagyi G, Rouzier R, et al. Outcome after pathologic complete eradication of cytologically proven breast cancer axillary node metastases following primary chemotherapy. J Clin Oncol. 2005;23(36):9304–11.
Alvarado R, Yi M, Le-Petross H, et al. The role for sentinel lymph node dissection after neoadjuvant chemotherapy in patients who present with node-positive breast cancer. Ann Surg Oncol. 2012;19(10):3177–83.
Classe J, Bordes V, Campion L, et al. Sentinel lymph node biopsy after neoadjuvant chemotherapy for advanced breast cancer: results of Ganglion Sentinelle et Chimiotherapie Neoadjuvante, a French prospective multicentric study. J Clin Oncol. 2009;27(5):726–32.
Newman E, Sabel M, Nees A, et al. Sentinel lymph node biopsy performed after neoadjuvant chemotherapy is accurate in patients with documented node-positive breast cancer at presentation. Ann Sug Oncol. 2007;14(10):2946–52.
Mamounas E, Brown A, Anderson S, et al. Sentinel node biopsy after neoadjuvant chemotherapy in breast cancer: results from National Surgical Adjuvant Breast and Bowel Project Protocol B-27. J Clin Oncol. 2005;23(12):2694–702.
Balch G, Mithani S, Richards K, Beauchamp R, Kelley M. Lymphatic mapping and sentinel lymphadenectomy after preoperative therapy for stage II and III breast cancer. Ann Surg Oncol. 2003;10(6):616–21.
Vriens BE, Keymeulen KB, Kroep JR, et al. Axillary staging in breast cancer patients treated with neoadjuvant chemotherapy in two Dutch phase III studies. Oncotarget. 2017. doi:10.18632/oncotarget.15101.
Boughey J, Suman V, Mittendorf E, et al. Sentinel lymph node surgery after neoadjuvant chemotherapy in patients with node-positive breast cancer: the ACOSOG Z1071 (Alliance) clinical trial. JAMA. 2013;310(14):1455–61.
Boughey J, Ballman K, Le-Petross H, et al. Identification and resection of clipped node decreases the false-negative rate of sentinel lymph node surgery in patients presenting with node-positive breast cancer (T0-T4, N1-N2) who receive neoadjuvant chemotherapy: results from ACOSOG Z1071 (Alliance). Ann Surg. 2016;263(4):802–7.
Boughey J, Ballman K, Symmans W, et al. Methods impacting the false negative rate of sentinel lymph node surgery in patients presenting with node positive breast cancer (T0-T4,N1-2) who receive neoadjuvant chemotherapy—Results from a prospective trial—ACOSOG Z1071 (Alliance). San Antonio Breast Cancer Symposium 2014 2014; Poster Presentation. http://eposter.abstractsonline.com/sabcs. Accessed 31 Jan 2015.
Boileau JF, Poirier B, Basik M, et al. Sentinel node biopsy after neoadjuvant chemotherapy in biopsy-proven node-positive breast cancer: the SN FNAC Study. J Clin Oncol. 2015;33(3):258–64.
Kuehn T, Bauerfeind I, Fehm T, et al. Sentinel-lymph-node biopsy in patients with breast cancer before and after neoadjuvant chemotherapy (SENTINA): a prospective, multicentre cohort study. Lancet Oncol. 2013;14(7):609–18.
Boughey J, Ballman K, Hunt K, et al. Axillary ultrasound after neoadjuvant chemotherapy and its impact on sentinel lymph node surgery: results from the American College of Surgeons Oncology Group Z1071 Trial (Alliance). J Clin Oncol. 2015;33(30):3368–93.
Pilewskie M, Morrow M. Axillary nodal management following neoadjuvant chemotherapy: a review. JAMA Oncol. 2016;3(4):549–555.
Mittendorf E, Caudle A, Yang W, et al. Implementation of the american college of surgeons oncology group z1071 trial data in clinical practice: is there a way forward for sentinel lymph node dissection in clinically node-positive breast cancer patients treated with neoadjuvant chemotherapy? Ann Surg Oncol. 2014;21(8):2468–73.
Mamtani A, Barrio A, Van Zee K, et al. How often does neoadjuvant chemotherapy avoid axillary dissection in patients with histologically confirmed nodal metastases? Results of a prospective study. Ann Surg Oncol. 2016;23(11):3467–74.
Jatoi I, Benson J, Toi M. De-escalation of axillary surgery in early breast cancer. Lancet Oncol. Oct 2016;17(10):e430–441.
Schwentner L, Helms G, Neklijudova V, et al. Using ultrasound and palpation for predicting axillary lymph node status following neoadjuvant chemotherapy—results from the multi-center SENTINA trial. Breast. 2017;31:202–7.
Caudle A, Yang W, Krishnamurthy S, et al. Improved axillary evaluation following neoadjuvant therapy for patients with node-positive breast cancer using selective evaluation of clipped nodes: implementation of targeted axillary dissection. J Clin Oncol. 2016;34(10):1072–8.
Caudle A, Yang W, Mittendorf E, et al. Selective surgical localization of axillary lymph nodes containing metastases in patients with breast cancer: a prospective feasibility trial. JAMA Surg. 2014;34(10):1072–8.
Pass H, Klimberg S, Copeland E. Are “breast-focused” surgeons more competent? Ann Surg Oncol. 2008;15(4):953–5.
Acknowledgement
Laura Randel and the American Society of Breast Surgeons provided the administrative support for the survey. Grant Support was provided by a Cancer Center Support Grant from the NIH (CA16672).
Disclosure
The authors have no financial disclosures.
Author information
Authors and Affiliations
Corresponding author
Appendix 1: Survey Sent to American Society of Breast Surgeons Membership
Appendix 1: Survey Sent to American Society of Breast Surgeons Membership
1. Which best describes your clinical practice?
-
Private practice general or oncologic surgeon who performs breast surgeries
-
Private practice breast-only surgeon
-
Academic general or oncologic surgeon who performs breast surgeries
-
Academic breast-only surgeon
-
I do not provide clinical care
2. How long have you been in clinical practice?
-
0–5 years
-
5–10 years
-
10–15 years
-
15–20 years
-
Greater than 20 years
3. Are you familiar with these recent multi-institutional trials evaluating the accuracy of sentinel lymph node biopsy in clinically node positive breast cancer patients who receive neoadjuvant therapy? Please check all trials with which you are familiar:
-
Yes, I am familiar with the ACOSOG Z1071 trial results
-
Yes, I am familiar with the SENTINA trial results
-
Yes, I am familiar with the SN FNAC trial results
-
No, I am not familiar with any of these trial result
4. The ACOSOG Z1071, SENTINA and SN FNAC trials all enrolled patients with clinically node positive breast cancer who received neoadjuvant chemotherapy then went on to SLND with planned completion ALND in order to determine the false negative rate of SLND. For patients who presented with clinical N1 (cN1) disease and had their SLN(s) examined by hematoxylin and eosin staining, the false negative rates in all of these studies was:
-
Less than 5%
-
5–9%
-
10–15%
-
>15%
-
I am not familiar with these trial results
5. Before publication of these trial results, did you perform SLND on clinically node positive patients after neoadjuvant chemotherapy with the intent to omit axillary lymph node dissection (ALND) if no residual disease was identified in the SLN(s)?
-
Most of the time
-
In select patients
-
No, my standard practice was to perform ALND
6. What is your current practice in regards to surgical management of clinically node positive patients (cN1) who receive neoadjuvant chemotherapy?
-
In the majority of patients (>50%), I perform SLND with the intent of omitting ALND if no disease is identified in the SLN(s)
-
In a select group of patients (<50%), I perform SLND with the intent of omitting ALND if no residual disease is identified in the SLN(s)
-
My standard practice is to perform ALND in all patients (Skip to question 11)
7. The aim of the following question is to determine which clinicopathologic features impact your pre-operative decision in determining whether a patient is appropriate for SLND and consideration of omission of ALND if no metastases are seen in the SLN(s) after neoadjuvant therapy. Please check all variables that you consider when determining eligibility for SLND in these patients: (Please check all that apply)
-
Primary tumor size
-
Number of abnormal axillary lymph nodes seen on US performed at the time of diagnosis before initiation of neoadjuvant chemotherapy
-
Status of axillary lymph nodes seen on US performed preoperatively after completion of neoadjuvant chemotherapy
-
Tumor subtype (Hormone receptor positive, HER2 positive, triple negative)
-
Patient age
-
Planned postoperative radiation
-
I do not consider any of these variables in my decision
8. The following question is to understand technical aspects that you consider crucial to the accuracy of SLND in clinically node positive patients who receive neoadjuvant chemotherapy. I believe that the following components must be in place for SLND results to be accurate:
Dual tracer technique (i.e. blue dye and radioisotope) | Yes | No |
Removal of ≥2 SLNs | Yes | No |
Removal of ≥3 SLNs | Yes | No |
The biopsied node has a clip placed at the time of diagnosis and removal of the clipped node at surgery is confirmed | Yes | No |
Immunohistochemistry is performed to confirm no residual metastasis | Yes | No |
Preoperative ultrasonography following neoadjuvant chemotherapy showing normalization of nodes | Yes | No |
9. Do you routinely have a clip placed in axillary nodes with biopsy-proven metastases? (If your answer is no, please skip to question #11) | Yes | No |
10. If a clip is placed in the biopsied node, how is this clipped node handled intra-operatively?
-
We place clips but do not assess for their removal at surgery
-
I do not selectively remove the clipped node, but I perform an x-ray of the nodes to confirm clip removal
-
I localize clipped nodes with wire/needle localization
-
I localize clipped nodes with I125 seeds
-
I localize clipped nodes with a method other than wire or seed localization
-
We do not place clips in nodes
11. If you do not rely on SLND to stage clinically node positive patients after neoadjuvant chemotherapy, what has limited your use of this technique? (Please check all that apply)
-
I do not feel the reported false negative rates for SLND are low enough to accurately assess axillary nodes after neoadjuvant chemotherapy
-
I do not feel that we have adequate data regarding the long-term, oncologic outcomes when ALND is omitted in these patients
-
I feel that SLND may be appropriate in some patients, but my institution does not have the resources that I feel are essential to accuracy of the technique (such as clip placement in biopsied nodes, or inability to localize clipped nodes)
-
I feel that SLND may be appropriate in some patients, but medical oncologists in my institution do not feel this is appropriate
-
I feel that SLND may be appropriate in some patients, but radiation oncologists in my institution do not feel this is appropriate
-
I feel that SLND may be appropriate in some patients, but other surgeons in my practice do not feel this is appropriate
-
My institution is currently collecting internal data to determine the FNR of SLND in our institution
-
I use SLND in this population with omission of ALND when no metastases are identified
Rights and permissions
About this article
Cite this article
Caudle, A.S., Bedrosian, I., Milton, D.R. et al. Use of Sentinel Lymph Node Dissection After Neoadjuvant Chemotherapy in Patients with Node-Positive Breast Cancer at Diagnosis: Practice Patterns of American Society of Breast Surgeons Members. Ann Surg Oncol 24, 2925–2934 (2017). https://doi.org/10.1245/s10434-017-5958-4
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-017-5958-4