Abstract
Background or Purpose
Computed tomography-guided high-dose-rate brachytherapy (CT-HDRBT) is an emerging therapeutic option for irresectable liver tumours. However, its potentially negative effect on liver function has not yet been investigated. The aim of this study was to evaluate CT-HDRBT for potential liver damage and functional impairment by means of quantitative liver function tests, patient safety, and survival.
Methods
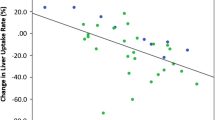
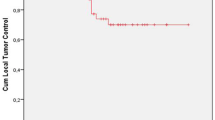
Sixty-nine patients receiving hepatic CT-HDRBT were investigated in a prospective study. The liver function was determined before and after intervention, and 6 and 12 weeks later. The study visits included liver function assessment by conventional biochemical parameters, the liver function capacity test based on 13C-Methacetin (MA) kinetics in µg/kg/hr (LiMAx test), and the indocyanine green plasma disappearance rate test. Tumour progression was re-staged by magnetic resonance imaging (MRI) twice. The 2-year-survival was analysed.
Results
A significant alteration of biochemical liver parameters was observed for liver enzymes and bilirubin directly after intervention, all biochemical parameters had normalised at the 6-week follow-up. There were no changes in LiMAx test values after the intervention, showing no effect on metabolic liver function capacity. In approximately two-thirds of the patients, MRI re-staging revealed a significant tumour response, and no local tumour recurrence occurred. No patient developed a radiation-induced liver disease.
Conclusion
CT-HDRBT for local tumour treatment has little impact on total liver function capacity by high patient safety and encouraging survival rates. Thus, it should be an important option in treating patients without a surgical alternative, especially when liver function is impaired due to previous surgery or chronic liver disease.




Similar content being viewed by others
References
Ricke J, Wust P. Computed tomography-guided brachytherapy for liver cancer. Semin Radiat Oncol. 2011;21:287–93.
Mohnike K, Wieners G, Schwartz F, et al. Computed tomography-guided high-dose-rate brachytherapy in hepatocellular carcinoma: safety, efficacy, and effect on survival. Int J Radiat Oncol Biol Phys. 2010;78:172–9.
Denecke T, Lopez Hanninen E. Brachytherapy of liver metastases. Recent Results Cancer Res. 2008;177:95–104.
Tselis N, Chatzikonstantinou G, Kolotas C, et al. Hypofractionated accelerated computed tomography-guided interstitial high-dose-rate brachytherapy for liver malignancies. Brachytherapy. 2012;11:507–14.
Tselis N, Chatzikonstantinou G, Kolotas C, et al. Computed tomography-guided interstitial high dose rate brachytherapy for central located liver tumours: a single institution study. Eur Radiol. 2013;23:2264–70.
Seidensticker M, Seidensticker R, Mohnike K, et al. Quantitative in vivo assessment of radiation injury of the liver using Gd-EOB-DTPA enhanced MRI: tolerance dose of small liver volumes. Radiat Oncol. 2011;6:40.
Dawson LA, Normolle D, Balter JM, et al. Analysis of radiation-induced liver disease using the Lyman NTCP model. Int J Radiat Oncol Biol Phys. 2002;53:810–21.
Emami B, Lyman J, Brown A, et al. Tolerance of normal tissue to therapeutic irradiation. Int J Radiat Oncol Biol Phys. 1991;21:109–22.
Marks LB, Yorke ED, Jackson A, et al. Use of normal tissue complication probability models in the clinic. Int J Radiat Oncol Biol Phys. 2010;76:10–9.
Stockmann M, Lock JF, Malinowski M, et al. The LiMAx test: a new liver function test for predicting postoperative outcome in liver surgery. HPB. 2010;12:139–46.
Rühl R, Lüdemann L, Czarnecka A, et. al. Radiobiological restrictions and tolerance doses of repeated single-fraction hdr-irradiation of intersecting small liver volumes for recurrent hepatic metastases. Radiat Oncol. 2010;5:44
Ricke J, Wust P, Wieners G, et al. Liver malignancies: CT-guided interstitial brachytherapy in patients with unfavorable lesions for thermal ablation. J Vasc Interv Radiol. 2004;15:1279–86.
Wieners G, Pech M, Rudzinska M, et. al. CT-guided interstitial brachytherapy in the local treatment of extrahepatic, extrapulmonary secondary malignancies. Eur Radiol. 2006;16:2586–2593.
Ricke J, Mohnike K, Pech M, et. al. Local response and impact on survival after local ablation of liver metastases from colorectal carcinoma by computed tomography-guided high-dose-rate brachytherapy. Int J Radiat Oncol Biol Phys. 2010;78:479–485
Schnapauff D, Denecke T, Grieser C, et al. Computed tomography-guided interstitial HDR brachytherapy (CT-HDRBT) of the liver in patients with irresectable intrahepatic cholangiocarcinoma. Cardiovasc Intervent Radiol. 2012;35:581–7.
Collettini F, Poellinger A, Schnapauff D, et al. CT-guided high-dose-rate brachytherapy of metachronous ovarian cancer metastasis to the liver: initial experience. Anticancer Res. 2011;31:2597–602.
Ruhl R, Seidensticker M, Peters N, et al. Hepatocellular carcinoma and liver cirrhosis: assessment of the liver function after Yttrium-90 radioembolization with resin microspheres or after CT-guided high-dose-rate brachytherapy. Dig Dis. 2009;27:189–99.
Stockmann M, Lock JF, Riecke B, et. al. Prediction of postoperative outcome after hepatectomy with a new bedside test for maximal liver function capacity. Ann Surg. 2009;250:119–25.
Stockmann M, Malinowski M, Lock JF, Seehofer D, Neuhaus P. Factors influencing the indocyanine green (ICG) test: additional impact of acute cholestasis. Hepatogastroenterology. 2009;56:734–8
Lock J, Malinowski M, Seehofer D, et al. Function and volume recovery after partial hepatectomy: influence of preoperative liver function, residual liver volume, and obesity. Langenbecks Arch Surg. 2012;397:1297–304.
Ricke J, Wust P, Wieners G, et al. Liver malignancies: CT-guided interstitial brachytherapy in patients with unfavorable lesions for thermal ablation. J Vasc Interv Radiol. 2004;15(11):1279–86.
Wieners G, Mohnike K, Peters N, et al. Treatment of hepatic metastases of breast cancer with CT-guided interstitial brachytherapy—a phase II-study. Radiother Oncol. 2011;100:314–9.
Llovet JM, Bruix J. Novel advancements in the management of hepatocellular carcinoma in 2008. J Hepatol. 2008;48 Suppl 1:20–37.
Stang A, Fischbach R, Teichmann W, et al. A systematic review on the clinical benefit and role of radiofrequency ablation as treatment of colorectal liver metastases. Eur J Cancer. 2009;45:1748–56.
Curley SA. Radiofrequency ablation versus resection for resectable colorectal liver metastases: time for a randomized trial? Ann Surg Oncol. 2008;15:11–3.
Disclosure
Martin Stockmann is the inventor of the LiMAx test and he has capital interest in Humedics, the company marketing the LiMAx test.
Author information
Authors and Affiliations
Corresponding author
Additional information
Georg Brinkhaus, Johan Friso Lock, Bernhard Gebauer and Martin Stockmann contributed equally to this work.
Rights and permissions
About this article
Cite this article
Brinkhaus, G., Lock, J.F., Malinowski, M. et al. CT-Guided High-Dose-Rate Brachytherapy of Liver Tumours Does Not Impair Hepatic Function and Shows High Overall Safety and Favourable Survival Rates. Ann Surg Oncol 21, 4284–4292 (2014). https://doi.org/10.1245/s10434-014-3835-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-014-3835-y