Abstract
Background and Purpose
The extracapsular spread (ECS) of lymph node metastasis (LNM) reflects tumor aggressiveness and is associated with poor survival and risk of distant metastasis. In this study, we aimed to explore the prognostic significance of epithelial-mesenchymal transition (EMT) of ECS tumors in LNM of head and neck cancers.
Methods
We collected LNM samples from head and neck cancer patients (follow-up >2 years) and made 20 ECS(−): ECS(+) pairs (1:2) of LNM (N = 60), matched by the primary sites and by T and N classifications. Immunostaining of cytokeratin, E-cadherin, vimentin, and CD31 were performed and quantified to determine the epithelial-mesenchymal transition percent (EMT%), defined as vimentin(+)/cytokeratin(+) area of ECS. Univariate and multivariable analyses of clinic-pathologic factors, including EMT% of ECS, were conducted to identify the significant prognosticators. In addition, the anatomical relationship between CD31 vessels and ECS tumors was analyzed.
Results
Rather than the presence of ECS in LNM, higher EMT% (>50 %) of ECS strongly correlated with the worse overall and disease-free survival and had more frequent recurrence and distant dissemination in their clinical courses. ECS tumors intermingled closely with Ki-67(−) CD31(+) non-proliferating perinodal blood vessels. Particularly, vimentin(+) ECS areas exhibited a higher density of CD31(+) perinodal vessels than did vimentin(−) ECS.
Conclusion
High EMT scores of ECS tumors in LNM predict an unfavorable prognosis and systemic dissemination more accurately than the simple presence of ECS in LNM in head and neck cancer patients.




Similar content being viewed by others
References
de Carvalho BM. Quantitative analysis of the extent of extracapsular invasion and its prognostic significance: a prospective study of 170 cases of carcinoma of the larynx and hypopharynx. Head Neck. 1998;20:16–21.
Grandi C, Alloisio M, Moglia D, et al. Prognostic significance of lymphatic spread in head and neck carcinomas: therapeutic implications. Head Neck Surg. 1985;8:67–73.
Greenberg JS, Fowler R, Gomez J, et al. Extent of extracapsular spread: a critical prognosticator in oral tongue cancer. Cancer. 2003;97:1464–70.
Gruber G, Bonetti M, Nasi ML, et al. Prognostic value of extracapsular tumor spread for locoregional control in premenopausal patients with node-positive breast cancer treated with classical cyclophosphamide, methotrexate, and fluorouracil: long-term observations from International Breast Cancer Study Group Trial VI. J Clin Oncol. 2005;23:7089–97.
Gruber G, Cole BF, Castiglione-Gertsch M, et al. Extracapsular tumor spread and the risk of local, axillary and supraclavicular recurrence in node-positive, premenopausal patients with breast cancer. Ann Oncol. 2008;19:1393–401.
Heide J, Krull A, Berger J. Extracapsular spread of nodal metastasis as a prognostic factor in rectal cancer. Int J Radiat Oncol Biol Phys. 2004;58:773–8.
Johnson JT, Barnes EL, Myers EN, Schramm VL, Jr., Borochovitz D, Sigler BA. The extracapsular spread of tumors in cervical node metastasis. Arch Otolaryngol. 1981;107:725–9.
Johnson JT, Myers EN, Bedetti CD, Barnes EL, Schramm VL, Jr., Thearle PB. Cervical lymph node metastases. Incidence and implications of extracapsular carcinoma. Arch Otolaryngol. 1985;111:534–7.
Jose J, Coatesworth AP, Johnston C, MacLennan K. Cervical node metastases in squamous cell carcinoma of the upper aerodigestive tract: the significance of extracapsular spread and soft tissue deposits. Head Neck. 2003;25:451–6.
Liao CT, Wang HM, Chang JT, et al. Analysis of risk factors for distant metastases in squamous cell carcinoma of the oral cavity. Cancer. 2007;110:1501–8.
Metindir J, Bilir Dilek G. Evaluation of prognostic significance in extracapsular spread of pelvic lymph node metastasis in patients with cervical cancer. Eur J Gynaecol Oncol. 2008;29:476–8.
Shaw RJ, Lowe D, Woolgar JA, et al. Extracapsular spread in oral squamous cell carcinoma. Head Neck. 2010;32:714–22.
van der Velden J, van Lindert AC, Lammes FB, et al. Extracapsular growth of lymph node metastases in squamous cell carcinoma of the vulva. The impact on recurrence and survival. Cancer. 1995;75:2885–90.
Richard JM, Sancho-Garnier H, Micheau C, Saravane D, Cachin Y. Prognostic factors in cervical lymph node metastasis in upper respiratory and digestive tract carcinomas: study of 1,713 cases during a 15-year period. Laryngoscope. 1987;97:97–101.
Ferlito A, Rinaldo A, Devaney KO, et al. Prognostic significance of microscopic and macroscopic extracapsular spread from metastatic tumor in the cervical lymph nodes. Oral Oncol. 2002;38:747–51.
Dobi E, Bazan F, Dufresne A, et al. Is extracapsular tumour spread a prognostic factor in patients with early breast cancer? Int J Clin Oncol. 2013;18:607–13.
Alakus H, Holscher AH, Grass G, et al. Extracapsular lymph node spread: a new prognostic factor in gastric cancer. Cancer. 2010;116:309–15.
Nakamura K, Ozaki N, Yamada T, et al. Evaluation of prognostic significance in extracapsular spread of lymph node metastasis in patients with gastric cancer. Surgery. 2005;137:511–7.
Myers JN, Greenberg JS, Mo V, Roberts D. Extracapsular spread. A significant predictor of treatment failure in patients with squamous cell carcinoma of the tongue. Cancer. 2001;92:3030–6.
Liao CT, Lee LY, Huang SF, et al. Outcome analysis of patients with oral cavity cancer and extracapsular spread in neck lymph nodes. Int J Radiat Oncol Biol Phys. 2011;81:930–7.
Michikawa C, Uzawa N, Sato H, Ohyama Y, Okada N, Amagasa T. Epidermal growth factor receptor gene copy number aberration at the primary tumour is significantly associated with extracapsular spread in oral cancer. Br J Cancer. 2011;104:850–5.
Prim MP, De Diego JI, Hardisson D, Madero R, Nistal M, Gavilan J. Extracapsular spread and desmoplastic pattern in neck lymph nodes: two prognostic factors of laryngeal cancer. Ann Otol Rhinol Laryngol. 1999;108:672–6.
Kuhnt T, Klockenbrink U, Knipping S, et al. Adjuvant low single dose cisplatin-based concurrent radiochemotherapy of oral cavity and oropharynx carcinoma: impact of extracapsular nodal spread on distant metastases. Strahlenther Onkol 2011;187:292–9.
Woolgar JA, Rogers S, West CR, Errington RD, Brown JS, Vaughan ED. Survival and patterns of recurrence in 200 oral cancer patients treated by radical surgery and neck dissection. Oral Oncol. 1999;35:257–65.
Rogers SN, Brown JS, Woolgar JA, et al. Survival following primary surgery for oral cancer. Oral Oncol. 2009;45:201–11.
Woolgar JA, Rogers SN, Lowe D, Brown JS, Vaughan ED. Cervical lymph node metastasis in oral cancer: the importance of even microscopic extracapsular spread. Oral Oncol. 2003;39:130–7.
Hellman S, Karnofsky Memorial Lecture. Natural history of small breast cancers. J Clin Oncol. 1994;12:2229–34.
Kawada K, Taketo MM. Significance and mechanism of lymph node metastasis in cancer progression. Cancer Res. 2011;71:1214–8.
Kim JM, Kim HJ, Koo BS, Rha KS, Yoon YH. Expression of matrix metalloproteinase-12 is correlated with extracapsular spread of tumor from nodes with metastasis in head and neck squamous cell carcinoma. Eur Arch Otorhinolaryngol. 2013;270:1137–42.
Brennan PA, Dennis S, Poller D, Quintero M, Puxeddu R, Thomas GJ. Inducible nitric oxide synthase: correlation with extracapsular spread and enhancement of tumor cell binvasion in head and neck squamous cell carcinoma. Head Neck. 2008;30:208–14.
Zhou X, Temam S, Oh M, et al. Global expression-based classification of lymph node metastasis and extracapsular spread of oral tongue squamous cell carcinoma. Neoplasia. 2006;8:925–32.
Smith A, Teknos TN, Pan Q. Epithelial to mesenchymal transition in head and neck squamous cell carcinoma. Oral Oncol. 2013;49:287–92.
Thiery JP. Epithelial-mesenchymal transitions in tumour progression. Nat Rev Cancer. 2002;2:442–54.
Kalluri R, Weinberg RA. The basics of epithelial-mesenchymal transition. J Clin Invest. 2009;119:1420–8.
Gunasinghe NP, Wells A, Thompson EW, Hugo HJ. Mesenchymal-epithelial transition (MET) as a mechanism for metastatic colonisation in breast cancer. Cancer Metastasis Rev. 2012;31:469–78.
Leemans CR, Tiwari R, Nauta JJ, van der Waal I, Snow GB. Regional lymph node involvement and its significance in the development of distant metastases in head and neck carcinoma. Cancer. 1993;71:452–6.
Carter RL, Barr LC, O’Brien CJ, Soo KC, Shaw HJ. Transcapsular spread of metastatic squamous cell carcinoma from cervical lymph nodes. Am J Surg. 1985;150:495–9.
Ferlito A, Rinaldo A, Buckley JG, Mondin V. General considerations on distant metastases from head and neck cancer. ORL J Otorhinolaryngol Relat Spec. 2001;63:189–91.
Ichii S, Imai Y, Irimura T. Initial steps in lymph node metastasis formation in an experimental system: possible involvement of recognition by macrophage C-type lectins. Cancer Immunol Immunother. 2000;49:1–9.
Cady B. Regional lymph node metastases; a singular manifestation of the process of clinical metastases in cancer: contemporary animal research and clinical reports suggest unifying concepts. Ann Surg Oncol. 2007;14:1790–800.
Acknowledgment
This work was supported by the National Research Foundation of Korea grant, the Korea government (MEST No. 2012R1A1A2040866), the Samsung Medical Center (Research Development Grant #GL1-B2-291-1), and the KIST-SMC Translational Research Project 2013.
Disclosure
The authors have declared no conflicts of interest.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Won-Yong Lee and Da-Yong Shin contributed equally as first author.
Electronic supplementary material
Below is the link to the electronic supplementary material.
10434_2014_3567_MOESM1_ESM.docx
Matched pairs of study subjects according to extra-capsular spread (ECS) status in lymph node metastasis (2:1 = ECS(+):ECS(-), N = 60) and follow-up outcomes Supplementary material 1 (DOCX 18 kb)
10434_2014_3567_MOESM2_ESM.tif
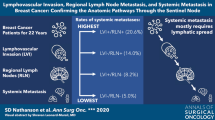
Enrollment of study subjects. Clinical characteristics of patients diagnosed with head and neck cancer and neck node metastasis (N = 110), including 84 extra-capsular spread (ECS)(+) tumors and 26 ECS(-) tumors. Subjects were divided into twenty 2:1 pairs (N = 60), exactly matched by primary sites, T and N classifications, with or without ECS; lymph node samples were used for analysis Supplementary material 2 (TIFF 1789 kb)
10434_2014_3567_MOESM3_ESM.tif
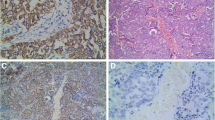
Quantification of the relative epithelial-mesenchymal transition (EMT) % in lymph node metastasis tumors.(A) To define the tumor area, we manually delineated a cytokeratin(+) area on slide scan images. For extra-capsular spread (ECS) tumor areas, we defined EMT % of ECS as the vimentin(+) areas divided by cytokeratin(+) ECS tumor areas, which were also manually determined.(B) EMT of intra-lymph node metastasis. Intra-lymph node metastases had peripheral vimentin(+) tumors around the deep portion of lymph nodes, whereas most of the tumor cells from the lymph node capsule were E-cadherin(+) and vimentin(-) Supplementary material 3 (TIFF 6471 kb)
10434_2014_3567_MOESM4_ESM.tif
Extent of ECS and patient prognosis. Survival curves showed that no significant differences between ECS(-), ECS(+) < 5 mm, and ECS(+) ≥ 5 mm in terms of overall survival Supplementary material 4 (TIFF 1096 kb)
Rights and permissions
About this article
Cite this article
Lee, WY., Shin, DY., Kim, H.J. et al. Prognostic Significance of Epithelial-Mesenchymal Transition of Extracapsular Spread Tumors in Lymph Node Metastases of Head and Neck Cancer. Ann Surg Oncol 21, 1904–1911 (2014). https://doi.org/10.1245/s10434-014-3567-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-014-3567-z