Abstract
Introduction
Microwave energy is another energy source than can be used to precoagulate hepatic tissue during hepatic resection. The aim of this study was to develop an optimal microwave precoagulation technique in a porcine model and then validate the technique during hepatic resection in patients.
Methods
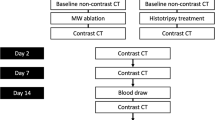
Institutional Animal Care and Use and Institutional Review Board (IRB)-approved protocols were utilized for hepatic resection in a porcine model and validation in patients using microwave energy for precoagulation. Different numbers of antennas (one, two or three; spaced 5 mm apart) and ablation times (20, 30, 40, and 60 s) were evaluated to identify an optimal technique that effectively provided precoagulation.
Results
Animal studies: Two antennas for 30 s provided the optimal ablation time, ablation width, mean size of largest vessel coagulated, and minimal bleeding when compared with other techniques. However, given that this is not an optimal technique for laparoscopic precoagulation, one antenna for 60 s was found to provide similar precoagulation success. Patient validation: To validate these techniques, three patients underwent open hepatectomy using two antennas with 5 mm spacing for 30 s, demonstrating successful precoagulation up to inflow/outflow vessels of 10 mm size or greater, which were controlled with a vascular stapler. In addition three patients underwent laparoscopic hepatectomy using one antenna for 60 s and demonstrated successful precoagulation up to inflow/outflow vessels of 8 mm or greater, which were controlled with a vascular stapler.
Conclusion
Microwave energy is a safe and effective precoagulation device to achieve good hemostasis during hepatic resection with both open and laparoscopic technique.





Similar content being viewed by others
References
Jarnagin WR, Gonen M, Fong Y, et al. Improvement in perioperative outcome after hepatic resection: analysis of 1,803 consecutive cases over the past decade. Ann Surg. 2002;236:397–407.
Lin TY. A simplified technique for hepatic resection: the crush method. Ann Surg. 1974;180:285–90.
Jiao LR, Ayav A, Navarra G, et al. Laparoscopic liver resection assisted by the laparoscopic Habib Sealer. Surgery. 2008;144:770–4.
Pai M, Jiao LR, Khorsandi S, et al. Liver resection with bipolar radiofrequency device: Habibtrade mark 4X. HPB (Oxford). 2008;10:256–60.
Poon RT. Current techniques of liver transection. HPB (Oxford). 2007;9:166–73.
Satoi S, Matsui Y, Kitade H, et al. Long-term outcome of hepatocellular carcinoma patients who underwent liver resection using microwave tissue coagulation. HPB (Oxford). 2008;10:289–95.
Martin RC, Scoggins CR, McMasters KM. A phase II study of radiofrequency ablation of unresectable metastatic colorectal cancer with hepatic arterial infusion pump chemotherapy. J Surg Oncol. 2006;93:387–93.
Martin RC, Scoggins CR, McMasters KM. Microwave hepatic ablation: initial experience of safety and efficacy. J Surg Oncol. 2007;96:481–6.
Martin R, Paty P, Fong Y, et al. Simultaneous liver and colorectal resections are safe for synchronous colorectal liver metastasis. J Am Coll Surg. 2003;197:233–41.
Martin RC, Edwards MJ, McMasters KM. Morbidity of adjuvant hepatic arterial infusion pump chemotherapy in the management of colorectal cancer metastatic to the liver. Am J Surg. 2004;188:714–21.
Hering J, Garrean S, Saied A, et al. Use of radiofrequency hepatic parenchymal transection device in hepatic hemangioma resection: early experience and lessons learned. HPB (Oxford). 2007;9:319–23.
Abouljoud MS, Arenas J, Yoshida A, et al. New application of the bipolar vapor plasma coagulation system for laparoscopic major liver resections. Surg Endosc. 2008;22:426–9.
Romano F, Garancini M, Caprotti R, et al. Hepatic resection using a bipolar vessel sealing device: technical and histological analysis. HPB (Oxford). 2007;9:339–44.
Goldberg SN, Charboneau JW, Dodd GD III, et al. Image-guided tumor ablation: proposal for standardization of terms and reporting criteria. Radiology. 2003;228:335–45.
Diederich CJ. Thermal ablation and high-temperature thermal therapy: overview of technology and clinical implementation. Int J Hyperthermia. 2005;21:745–53.
Funding Support
Unrestricted education grant from Covidien, Inc.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Reuter, N.P., Martin, R.C.G. Microwave Energy as a Precoagulative Device to Assist in Hepatic Resection. Ann Surg Oncol 16, 3057–3063 (2009). https://doi.org/10.1245/s10434-009-0688-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-009-0688-x