Abstract
μ-Conotoxin CnIIIC (conotoxin, CTX)–loaded chitosan nanoparticles (CTX-NPs) were prepared using the ionic cross-linking method. The CTX-NPs were spherical and well with a polydispersity index of 0.292 ± 0.039, drug loading efficiency of 25.9 ± 1.2%, and encapsulation efficiency of 95.6 ± 1.3%. In vitro release studies showed that the release behavior of CTX-NPs in a pH 5.0 acetate buffer followed zero-order kinetics. In vitro transdermal experiments using Franz diffusion cells mounted with mouse abdominal skin demonstrated that the cumulative intradermal deposition amount of CTX per unit area in 8 h (D8) and permeability coefficient (Pf) of CTX loaded on CTX-NPs were 2.30- and 7.71-times that of the CTX solution. In vivo transdermal experiments in mice showed that the amount of CTX deposited in the skin after 8 h of CTX saline administration was significantly lower than that of CTX deposited in the skin after administration of CTX-NPs. In vitro fluorescence labeling transdermal studies through Franz diffusion cells mounted with mouse abdominal skin indicated that CTX-NPs aggregated at hair follicles. Skin irritation tests in mice indicated that the irritation due to CTX-NPs was negligible. The cytotoxicity experiment showed that the viability of Balb/c 3T3 cells with CTX-NPs containing 230 μg/mL (0.08 μM) CTX was greater than 75%. CTX-NPs increase intradermal deposition of CTX by accumulating in hair follicles, which has positive implications for transdermal penetration of CTX.






Similar content being viewed by others
Data Availability
Data sharing is not applicable to this article as no new data were created or analyzed in this study.
Abbreviations
- CS:
-
Chitosan
- DMEM:
-
Dulbecco’s modified Eagle’s medium
- HPLC:
-
High-performance liquid chromatography
- NIH:
-
National Institutes of Health
- NLC:
-
Nanostructured lipid carriers
- OD:
-
Optical density
References
Favreau P, Benoit E, Hocking HG, Carlier L, D' hoedt D, Leipold E, et al. A novel micro-conopeptide, CnIIIC, exerts potent and preferential inhibition of NaV1.2/1.4 channels and blocks neuronal nicotinic acetylcholine receptors. Br J Pharmacol. 2012;166(5):1654–68. https://doi.org/10.1111/j.1476-5381.2012.01837.x.
Chen R, Robinson A, Chung SH. Mechanism of mu-conotoxin PIIIA binding to the voltage-gated Na+ channel NaV1.4. PLoS One. 2014;9(3):e93267. https://doi.org/10.1371/journal.pone.0093267.
Mahdavi S, Kuyucak S. Systematic study of binding of mu-conotoxins to the sodium channel NaV1.4. Toxins (Basel). 2014;6(12):3454–70. https://doi.org/10.3390/toxins6123454.
Del Rio-Sancho S, Cros C, Coutaz B, Cuendet M, Kalia YN. Cutaneous iontophoresis of mu-conotoxin CnIIIC-A potent NaV1.4 antagonist with analgesic, anaesthetic and myorelaxant properties. Int J Pharm. 2017;518(1–2):59–65. https://doi.org/10.1016/j.ijpharm.2016.12.054.
Dragicevic N, Maibach H. Combined use of nanocarriers and physical methods for percutaneous penetration enhancement. Adv Drug Deliv Rev. 2018;127:58–84. https://doi.org/10.1016/j.addr.2018.02.003.
Lin X, Wang Z, Ou H, Mitragotri S, Chen M. Correlations between skin barrier integrity and delivery of hydrophilic molecules in the presence of penetration enhancers. Pharm Res. 2020;37(6):100. https://doi.org/10.1007/s11095-020-02800-4.
Ita KB. Chemical penetration enhancers for transdermal drug delivery - success and challenges. Curr Drug Deliv. 2015;12(6):645–51. https://doi.org/10.2174/1567201812666150804104600.
Kovacik A, Kopecna M, Vavrova K. Permeation enhancers in transdermal drug delivery: benefits and limitations. Expert Opin Drug Deliv. 2020;17(2):145–55. https://doi.org/10.1080/17425247.2020.1713087.
Raphael AP, Wright OR, Benson HA, Prow TW. Recent advances in physical delivery enhancement of topical drugs. Curr Pharm Des. 2015;21(20):2830–47. https://doi.org/10.2174/1381612821666150428144852.
Elmowafy M. Skin penetration/permeation success determinants of nanocarriers: pursuit of a perfect formulation. Colloids Surf B Biointerfaces. 2021;203:111748. https://doi.org/10.1016/j.colsurfb.2021.111748.
Huang CS, Xu QC, Dai C, Wang L, Tien YC, Li F, et al. Nanomaterial-facilitated cyclin-dependent kinase 7 inhibition suppresses gallbladder cancer progression via targeting transcriptional addiction. ACS Nano. 2021;15(9):14744–55. https://doi.org/10.1021/acsnano.1c04570.
Xinru You LW, Li Wang, Jun Wu. rebirth of aspirin synthesis by-broduct: prickly poly(salicylic acid) nanoparticles as self-anticancer drug carrier. Advanced Functional Materials. 2021;31(33). https://doi.org/10.1002/adfm.202100805.
Kahraman E, Gungor S, Ozsoy Y. Potential enhancement and targeting strategies of polymeric and lipid-based nanocarriers in dermal drug delivery. Ther Deliv. 2017;8(11):967–85. https://doi.org/10.4155/tde-2017-0075.
Yu YQ, Yang X, Wu XF, Fan YB. Enhancing permeation of drug molecules across the skin via delivery in nanocarriers: novel strategies for effective transdermal applications. Front Bioeng Biotechnol. 2021;9:646554. https://doi.org/10.3389/fbioe.2021.646554.
Jun Huang X, Xin P, Gu Z, Chen C, Wua J. Egg white as a natural and safe biomaterial for enhanced cancer therapy. Chinese Chem Lett. 2021;32(5):1737-42. https://doi.org/10.1016/j.cclet.2020.12.006.
Mu M, Liang X, Chuan D, Zhao S, Yu W, Fan R, et al. Chitosan coated pH-responsive metal-polyphenol delivery platform for melanoma chemotherapy. Carbohydr Polym. 2021;264:118000. https://doi.org/10.1016/j.carbpol.2021.118000.
Vllasaliu D, Exposito-Harris R, Heras A, Casettari L, Garnett M, Illum L, et al. Tight junction modulation by chitosan nanoparticles: comparison with chitosan solution. Int J Pharm. 2010;400(1–2):183–93. https://doi.org/10.1016/j.ijpharm.2010.08.020.
Nawaz A, Wong TW. Quantitative characterization of chitosan in the skin by Fourier-transform infrared spectroscopic imaging and ninhydrin assay: application in transdermal sciences. J Microsc. 2016;263(1):34–42. https://doi.org/10.1111/jmi.12371.
Shi L, Li Z, Liang Z, Zhang J, Liu R, Chu D, et al. A dual-functional chitosan derivative platform for fungal keratitis. Carbohydr Polym. 2022;275:118762. https://doi.org/10.1016/j.carbpol.2021.118762.
Takeuchi I, Takeshita T, Suzuki T, Makino K. Iontophoretic transdermal delivery using chitosan-coated PLGA nanoparticles for positively charged drugs. Colloids Surf B Biointerfaces. 2017;160:520–6. https://doi.org/10.1016/j.colsurfb.2017.10.011.
Nasti A, Zaki NM, de Leonardis P, Ungphaiboon S, Sansongsak P, Rimoli MG, et al. Chitosan/TPP and chitosan/TPP-hyaluronic acid nanoparticles: systematic optimisation of the preparative process and preliminary biological evaluation. Pharm Res. 2009;26(8):1918–30. https://doi.org/10.1007/s11095-009-9908-0.
Kim MH, Kim KT, Sohn SY, Lee JY, Lee CH, Yang H, et al. Formulation and evaluation of nanostructured lipid carriers (NLCs) of 20(S)-protopanaxadiol (PPD) by box-behnken design. Int J Nanomedicine. 2019;14:8509–20. https://doi.org/10.2147/IJN.S215835.
Ameeduzzafar, Alruwaili NK, Imam SS, Alotaibi NH, Alhakamy NA, Alharbi KS, et al. formulation of chitosan polymeric vesicles of ciprofloxacin for ocular delivery: Box-Behnken optimization, In Vitro Characterization, HET-CAM Irritation, and Antimicrobial Assessment. AAPS PharmSciTech. 2020;21(5):167. https://doi.org/10.1208/s12249-020-01699-9.
Pourtalebi Jahromi L, Ghazali M, Ashrafi H, Azadi A. A comparison of models for the analysis of the kinetics of drug release from PLGA-based nanoparticles. Heliyon. 2020;6(2):e03451. https://doi.org/10.1016/j.heliyon.2020.e03451.
Venter JP, Muller DG, du Plessis J, Goosen C. A comparative study of an in situ adapted diffusion cell and an in vitro Franz diffusion cell method for transdermal absorption of doxylamine. Eur J Pharm Sci. 2001;13(2):169–77. https://doi.org/10.1016/s0928-0987(01)00110-5.
Zhang H, Zhu X, Shen J, Xu H, Ma M, Gu W, et al. Characterization of a liposome-based artificial skin membrane for in vitro permeation studies using Franz diffusion cell device. J Liposome Res. 2017;27(4):302–11. https://doi.org/10.1080/08982104.2016.1231205.
Mundada AS, Avari JG. In vitro and in vivo characterization of novel biomaterial for transdermal application. Curr Drug Deliv. 2011;8(5):517–25. https://doi.org/10.2174/156720111796642264.
Sheshala R, Anuar NK, Abu Samah NH, Wong TW. in Vitro drug dissolution/permeation testing of nanocarriers for skin application: a comprehensive review. AAPS PharmSciTech. 2019;20(5):164. https://doi.org/10.1208/s12249-019-1362-7.
Balzus B, Colombo M, Sahle FF, Zoubari G, Staufenbiel S, Bodmeier R. Comparison of different in vitro release methods used to investigate nanocarriers intended for dermal application. Int J Pharm. 2016;513(1–2):247–54. https://doi.org/10.1016/j.ijpharm.2016.09.033.
Solomon D, Gupta N, Mulla NS, Shukla S, Guerrero YA, Gupta V. role of In vitro release methods in liposomal formulation development: challenges and regulatory perspective. AAPS J. 2017;19(6):1669–81. https://doi.org/10.1208/s12248-017-0142-0.
Cetin M, Atila A, Kadioglu Y. Formulation and in vitro characterization of Eudragit(R) L100 and Eudragit(R) L100-PLGA nanoparticles containing diclofenac sodium. AAPS PharmSciTech. 2010;11(3):1250–6. https://doi.org/10.1208/s12249-010-9489-6.
Hasanovic A, Zehl M, Reznicek G, Valenta C. Chitosan-tripolyphosphate nanoparticles as a possible skin drug delivery system for aciclovir with enhanced stability. J Pharm Pharmacol. 2009;61(12):1609–16. https://doi.org/10.1211/jpp/61.12.0004.
Valenzuela P, Simon JA. Nanoparticle delivery for transdermal HRT. Maturitas. 2012;73(1):74–80. https://doi.org/10.1016/j.maturitas.2011.12.019.
Manikkath J, Sumathy TK, Manikkath A, Mutalik S. delving deeper into dermal and transdermal drug delivery: factors and mechanisms associated with nanocarrier-mediated strategies. Curr Pharm Des. 2018;24(27):3210–22. https://doi.org/10.2174/1381612824666180924122640.
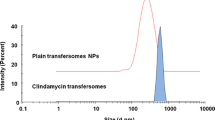
Tolentino S, Pereira MN, Cunha-Filho M, Gratieri T, Gelfuso GM. Targeted clindamycin delivery to pilosebaceous units by chitosan or hyaluronic acid nanoparticles for improved topical treatment of acne vulgaris. Carbohydr Polym. 2021;253:117295. https://doi.org/10.1016/j.carbpol.2020.117295.
Knorr F, Lademann J, Patzelt A, Sterry W, Blume-Peytavi U, Vogt A. Follicular transport route–research progress and future perspectives. Eur J Pharm Biopharm. 2009;71(2):173–80. https://doi.org/10.1016/j.ejpb.2008.11.001.
Yu Z, Meng X, Zhang S, Chen Y, Zhang Z, Zhang Y. Recent progress in transdermal nanocarriers and their Surface modifications. Molecules. 2021;26(11). https://doi.org/10.3390/molecules26113093.
Patzelt A, Lademann J. Recent advances in follicular drug delivery of nanoparticles. Expert Opin Drug Deliv. 2020;17(1):49–60. https://doi.org/10.1080/17425247.2020.1700226.
Abdel-Hafez SM, Hathout RM, Sammour OA. Tracking the transdermal penetration pathways of optimized curcumin-loaded chitosan nanoparticles via confocal laser scanning microscopy. Int J Biol Macromol. 2018;108:753–64. https://doi.org/10.1016/j.ijbiomac.2017.10.170.
Tak YK, Pal S, Naoghare PK, Rangasamy S, Song JM. Shape-dependent skin penetration of silver nanoparticles: does it really matter? Sci Rep. 2015;5:16908. https://doi.org/10.1038/srep16908.
Prow TW, Grice JE, Lin LL, Faye R, Butler M, Becker W, et al. Nanoparticles and microparticles for skin drug delivery. Adv Drug Deliv Rev. 2011;63(6):470–91. https://doi.org/10.1016/j.addr.2011.01.012.
Yang X, Yang K, Yu F, Chen X, Wu S, Zhu Z. Preparation of novel bilayer hydrogels by combination of irradiation and freeze–thawing and their physical and biological properties. polymer international. 2009;58(11):8. https://doi.org/10.1002/pi.2662.
Acknowledgements
We would like to express our gratitude to all laboratory members for their technical advice and assistance. We also thank Renrui Biotechnology Inc. for providing the reagents.
Funding
This work was supported by grants from the 2019 Linyi Key R&D Program Project (grant number 2019ZDYF007) , Rizhao Science and Technology Innovation Project (Project Number: 2019CXZX1205) and Shandong Province Small And Medium-sized Technology-based Enterprise Innovation Ability Improvement Project (Project Number: 2021TSGC1246).
Author information
Authors and Affiliations
Contributions
J.Z. and C.Z. conceived and designed study. Y.G. and J.H. conducted experiments. H. Z and Z.Z. analyzed data. H.L. and J.Y. wrote the manuscript. All authors read and approved the manuscript.
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, H., Yao, J., Guo, Y. et al. Preparation of Conotoxin-Encapsulated Chitosan Nanoparticles and Evaluation of Their Skin Permeability. AAPS PharmSciTech 24, 53 (2023). https://doi.org/10.1208/s12249-023-02509-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1208/s12249-023-02509-8